Epistaxis as an Unusual Sentinel Event for Chronic Subdural Hematoma: A Case Report
by Anamaria Rama*, Sabina Sherri, Edmond Zefi, Elsuida Prendi
Department of Neurology, University Hospital, Tirana, Albania
*Corresponding author: Anamaria Rama, Department of Neurology, University Hospital, Tirana, Albania
Received Date: 13 September 2025
Accepted Date: 18 September 2025
Published Date: 22 September 2025
Citation: Rama A, Sherri S, Zefi E, Prendi E. (2025). Epistaxis as an Unusual Sentinel Event for Chronic Subdural Hematoma: A Case Report. Ann Case Report. 10: 2416. https://doi.org/10.29011/2574-7754.102416
Introduction
Epistaxis is commonly attributed to local factors or systemic conditions such as hypertension and coagulopathy. However, it can also though rarely signal an underlying intracranial pathology. This case report presents a 55- year old patient who experienced two consecutive episodes of epistaxis, linked to an undiagnosed subdural hematoma.
Case Report
Referred by a cardiologist, this patient came to our clinic due to his sudden bleeding episodes, which could not be explained by elevated blood pressure, neither from an othorinolaringologic exam. Apart from being a chronic etilist, he had previously enjoyed good health and had never experienced nosebleeds before. He did not report other complaints, but upon insistent questioning, he also reported episodes of headaches, characterized by a moderate, tension, like sensation radiating from the occipital region, with a pain level of 7, sometimes 8 out of 10. These persistent headaches, occurring both day and night, with only slight relief from analgesics, raised our suspicions further. The patient didn`t suffer from any particular condition, except being a chronic etilist.
The patient recalled a car accident three months prior, during which he might have sustained a head injury, but no imaging study was performed at that time. This context made us reconsider his symptoms, and a brain CT was performed, showing a left subdural hematoma (Figure 1).
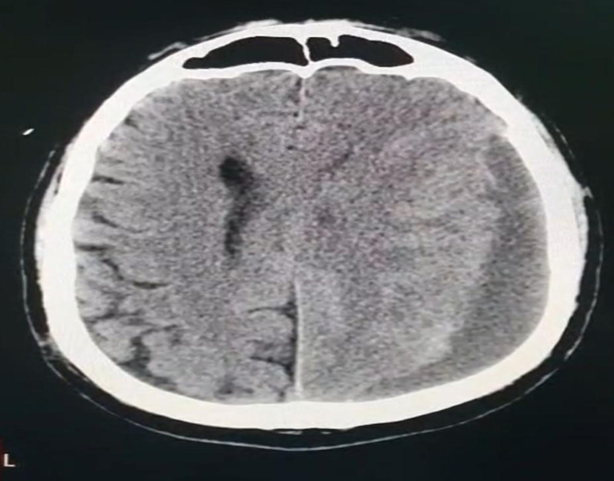
Figure 1: Non-contrast brain CT demonstrating a left chronic subdural hematoma. The axial section shows a crescent-shaped, hypodense collection along the left cerebral hemisphere, consistent with chronic subdural hematoma, causing mild mass effect and midline shift.
Discussion
We often associate nosebleed episodes with hypertension, leading to a typical diagnostic path that includes consultations with ENT specialists, allergists, or infectious disease experts. However, it is uncommon to refer a case of epistaxis to a neurologist, particularly when no other neurological symptoms, such as headache, are present.
Several risk factors can predispose patients to nosebleeds, including the use of antiplatelet or anticoagulant medications, alcohol consumption, and either coagulopathy or thrombocytopenia [1]. While nosebleeds can occasionally derive from intracranial causes, it is almost impossible for them to be linked directly to a subdural hematoma. Typically, such episodes are associated with false traumatic aneurysms resulting from skull fractures. Oley et al. reported two cases where facial trauma led to the formation of a pseudoaneurysm in the sphenopalatine artery [2]. Nevertheless, trauma is not a ´sine qua non´ prerequisite for aneurysm development. For example, Honeybul et al. described a significant epistaxis in a 56-year-old patient caused by a true aneurysm of the left internal carotid artery, which protruded through a bony deficiency of the sphenoid [3].
In our case, neither a false nor a true aneurysm was identified. A thorough literature review revealed no documented instances of chronic subdural hematoma manifesting with epistaxis. This led us to consider that the two episodes of nosebleeds might have been incidental and occurred purely by chance. Notably, 70-80% of epistaxis cases are classified as idiopathic [4]. However, the patient did possess a significant risk factor: he was a chronic alcohol user. A review by McGarry et al. highlighted that even low levels of alcohol consumption, such as 1 to 10 units per week, can lead to prolonged bleeding times and hemostatic abnormalities [5].
Conclusion
Even when a particular finding, appear to be incidental, it should be furtherly investigated, especially when we don´t find a logical explanation of this symptom, or this symptom is present in the context of other associating features or a suspicious anamnesis. In our case, epistaxis, while it may not be directly correlated with the underlying pathology, still served as the main ´spy´ of the pathology.
This case highlights the necessity of a holistic approach in patient care. It is essential for specialists to go beyond their specific clinical focus and consider the patient as a whole.
While we found no direct literature linking subdural hematoma to episodes of epistaxis, this should not stop future exploration. It is possible that there are cases yet to be documented, highlighting a gap in current medical understanding. As such, we should remain open to the idea that existing knowledge may evolve as more cases are assessed.
References
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.