Epiploic Appendagitis Mimicking Diverticulitis in an Elderly Male: A Case Report
by Brandon Gaffoor*, Vasanthi Arumugam
Internal Medicine, Get Well Medical PC, Jamaica, NY, USA
*Corresponding author: Brandon Gaffoor, Internal Medicine, Get Well Medical PC, Jamaica, NY, USA
Received Date: 17 June, 2025
Accepted Date: 26 June, 2025
Published Date: 30 June, 2025
Citation: Gaffoor B, Arumugam V (2025) Epiploic Appendagitis Mimicking Diverticulitis in an Elderly Male: A Case Report. Arch Gastroenterol Hepatol 5: 113. https://doi.org/10.29011/AGEH-113.000113
Abstract
Epiploic appendagitis (EA) is an uncommon and often underrecognized cause of acute abdominal pain, resulting from inflammation or infarction of the epiploic appendages, which are fat-filled, serosa-covered peritoneal structures that are located on the surface of the colon. These appendages are susceptible to torsion or spontaneous venous thrombosis due to their narrow vascular stalks, which can lead to localized ischemia. Clinically, EA often presents suddenly with localized abdominal pain that may mimic more prevalent conditions such as diverticulitis, appendicitis, or cholecystitis. Because it lacks distinguishing systemic symptoms like fever, nausea, vomiting, or leukocytosis, EA is frequently misdiagnosed, resulting in unnecessary use of antibiotics, hospital admissions, or even surgical intervention. With the growing use of abdominal computed tomography (CT) in emergency departments, EA is now more readily identified based on characteristic imaging findings, enabling healthcare providers to distinguish it from other causes of acute abdominal pain and manage it conservatively.
Keywords: Epiploic Appendagitis; Appendages; Thrombosis; Abdominal Pain; Diverticulitis
Introduction
Epiploic appendagitis (EA) is an uncommon and frequently underrecognized cause of acute abdominal pain that can mimic more serious abdominal conditions. It involves inflammation of the epiploic appendages—small, fat-filled, serosa-covered peritoneal outpouchings that project from the surface of the colon. These appendages, which range in size from 0.5 to 5 cm, are attached to the colon via a narrow vascular stalk, making them susceptible to torsion or spontaneous venous thrombosis, which can lead to localized ischemia and infarction [1-4].
Due to its nonspecific clinical presentation, EA is often misdiagnosed as appendicitis, diverticulitis, or cholecystitis, especially when abdominal pain is localized to a single quadrant. Unlike these more common surgical conditions, EA is self-limited and typically managed without invasive procedures. Misdiagnosis may result in unnecessary imaging, antibiotic use, hospital admission, or surgical intervention, highlighting the importance of heightened clinical awareness and appropriate use of imaging [3,5].
The increased use of CT imaging in emergency settings has improved the recognition of EA and helped reduce overtreatment. This case illustrates a presentation of EA in a patient whose symptoms initially suggested a more common abdominal pathology, ultimately highlighting the essential role of imaging and clinical analysis in reaching an accurate diagnosis.
Case Presentation
A 75-year-old male with a past medical history of hypertension, hypercholesterolemia, and second metatarsophalangeal joint instability presented to the emergency department with five days of sudden-onset abdominal pain. The patient was initially advised to seek care on 6/19/24 but delayed presentation until 6/22/24. He described the pain as constant, sharp, non-radiating, and likened it to “pins and needles,” rating the intensity as 10/10. The pain was most severe in the left lower quadrant (LLQ), exacerbated by moving from sitting to standing, and relieved in the supine position. The pain began after heavy lifting. The patient denied taking any medications or home remedies for symptom relief.
He denies any fever, nausea, vomiting, diarrhea, constipation, inflammation, or skin changes. He had no surgical history and reported no similar episodes of pain in the past. Medications included metoprolol and atorvastatin; he reported no known allergies. Notably, the pain resolved spontaneously after approximately one week without intervention.
In the emergency department, a CT scan of the abdomen and pelvis revealed mild colonic diverticulosis without signs of acute diverticulitis and left mid-abdomen antimesenteric focal fat infiltration in the epiploic appendages. The figures below are CT scans of the transverse and coronal abdominal views, respectively, illustrating antimesenteric focal fat infiltration in the left mid-abdomen, which suggests EA (Figures 1 and 2). The scan also revealed right lower lobe pulmonary nodules measuring up to 0.6 cm, with a recommendation for chest CT follow-up in 6–12 months. Prominent vascular calcifications were evident in the aortoiliac arteries. A transthoracic echocardiogram (TTE) performed subsequently demonstrated a trileaflet aortic valve with reduced systolic excursion, moderate calcific aortic stenosis, and trace aortic regurgitation. The patient left the ED prior to receiving a formal diagnosis and was later informed of the findings by his internist.
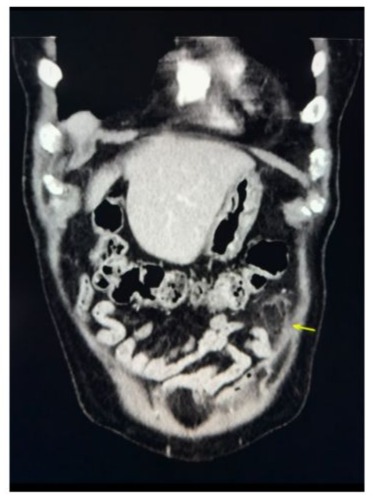
Figure 1: Coronal view of EA with arrow pointing to left mid-abdomen antimesenteric focal fat infiltration.

Figure 2: Transverse view of EA pointing to left mid-abdomen antimesenteric focal fat infiltration.
Discussion
Epiploic appendages are small, fat-filled pouches of visceral peritoneum that extend from the colon’s surface. Arranged in two rows adjacent to the anterior and posterior tenia coli, they are particularly abundant in the transverse and sigmoid colon [1,4]. Their narrow vascular stalk can make them more susceptible to torsion or spontaneous venous thrombosis, resulting in ischemia or infarction [6].
Abdominal pain is one of the most common complaints reported in the emergency department, and EA is often overlooked due to its rarity and symptom overlap with other acute abdominal conditions. Typical EA presents with localized, non-radiating, severe LLQ pain without fever, gastrointestinal upset, or systemic inflammation [3,5]. It tends to occur more frequently in obese, middle-aged males and has associations with diverticulosis, strenuous exercise, and hernias [1,7].
EA is best visualized on CT, where it appears as an ovoid fat-density lesion adjacent to the colon, often surrounded by a thin hyperattenuating ring of inflamed visceral peritoneum—a distinct feature known as the "hyperattenuating ring sign" [2,6]. The absence of surrounding bowel wall thickening helps distinguish EA from diverticulitis.
Management of EA is conservative. Since it is self-limited, treatment typically involves NSAIDs for pain control. Antibiotics and surgery are discouraged unless complications arise or the diagnosis is uncertain. The estimated annual incidence of EA is approximately 8.8 per million people, although the true number is likely underestimated due to its benign course and the fact that many patients recover without seeking medical care [1,6]. Increased use of abdominal CT and ultrasound has contributed to better recognition and has reduced the frequency of unnecessary interventions.
Conclusion
We report a case of EA that is particularly notable because the patient not only had findings of EA but also coinciding diverticulosis, signs suggestive of cystitis, and moderate calcific aortic stenosis. Epiploic appendagitis is a rare but important differential diagnosis in patients presenting with acute, localized abdominal pain, especially in the absence of fever or gastrointestinal symptoms. While benign and self-limiting, failure to recognize EA can lead to inappropriate use of antibiotics, unwarranted hospital admissions, and unnecessary surgical procedures.
CT imaging remains integral for accurate diagnosis, with the “hyperattenuating ring sign” and adjacent fat-density lesion serving as key radiologic features. Early and accurate identification facilitates appropriate, conservative management and avoids escalation of care.
This case underscores the clinical relevance of EA as a mimic of more serious abdominal pathology and emphasizes the value of imaging assessment and detailed clinical history in preventing overtreatment. Greater awareness among emergency providers and internists can improve patient outcomes for this underdiagnosed condition.
Declarations
Contributors: All authors contributed to planning, literature review and conduct of the review article. All authors have reviewed and agreed on the final manuscript.
Competing interests: None
Patient consent for publication: Informed consent was obtained from the patient
Ethics approval and consent to participate: Not Applicable
Availability of data and materials: Not applicable
Funding: Not Applicable
References
- Akubudike JTE, Egigba OF, Kobalava B (2021) Epiploic Appendagitis: A Commonly Overlooked Differential of Acute Abdominal Pain. Cureus 13: e12807.
- Aljilly S, Ahmed Z (2021) Epiploic appendagitis of the vermiform appendix––An unusual mimic of acute appendicitis. Radiol Case Rep 16: 511-515.
- Chin J, Oseguera B, Hon K, Lomiguen CM, McBride T (2022) Epiploic Appendagitis Mimicking Acute Appendicitis: An Osteopathic Case Report. Cureus 14: e32499.
- Gaur S, Jawahar RP, Prasad R, Prabakaran M (2021) Epiploic appendagitis - a rare cause of acute lower abdominal pain. Radiol Case Rep 16: 1144-1147.
- Nakagawa H, Miyata Y (2022) Abdominal pain caused by epiploic appendagitis. CMAJ 194: E942-E942.
- Patel M, Haider I, Cheung A (2023) Primary Epiploic Appendagitis: A Mimicker of Abdominal Pain. Clin Med Res 21: 159-162.
- Slaiki S, Afdil M, El Bouhaddouti H, Benjelloun EB, Ousadden A, et al. (2020) Epiploic appendagitis: a rare cause of acute abdomen. Pan Afr Med J 36: 149.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.