Epidural Catheter and Radiofrequency Therapy in Spinal Cord Injury Patients: Series of Case Reports
by by Mohammad Moulhem Arous1*, Ismail Moulhem Arous1, Basel AlAkhras1, Raed Al-Zoubi2,3, Aksam Yassin4,5
1Departmentr of Speciality Centre for Neurosurgery Prof. & Dr. Arous, Hamburg, Germany
2Departmentr of Surgical Research Section, Department of Surgery, Hamad Medical Corporation, Doha, Qatar
3Department of Biomedical Sciences, QU-Health, College of Health Sciences, Qatar University, Doha, 2713, Qatar
4Department of Surgery, Division of Urology/Andrology & Men;s Health Unit, Aisha Al Attiyah Hospital, Qatar
5Dresden International University, Center of Medicine and Health Sciences, Dresden 01069, Germany
*Corresponding author: Mohammad Moulhem Arous, Departmentr of Speciality Centre for Neurosurgery Prof. & Dr. Arous, Hamburg, Germany
Received Date: 30 April 2025
Accepted Date: 05 May 2025
Published Date: 07 May 2025
Citation: Arous MM, Arous IM, AlAkhras B, Al-Zoubi R, Yassin A (2025) Epidural Catheter and Radiofrequency Therapy in Spinal Cord Injury Patients: Series of Case Reports. J Surg 10: 11327 https://doi.org/10.29011/2575-9760.011327
Abstract
Aims: Epidural catheter therapy (ECT) has emerged as a promising treatment option for patients with degenerative spinal conditions and associated syndromes. Its potential in improving rehabilitation outcomes for spinal cord injury (SCI) patients has been increasingly recognized, although literature documenting its efficacy remains limited. In this study, we report the clinical benefits observed in three SCI patients following repeated ECT sessions, supplemented with various minimally invasive adjuvant therapies.
Methods: Three patients with debilitating SCI underwent a comprehensive course of ECT, complemented by variable minimally invasive adjuvant treatments. Clinical outcomes were systematically assessed to evaluate the efficacy and safety of the treatment regimen.
Results: All three SCI patients exhibited significant improvements in clinical symptoms and functional outcomes following the treatment protocol. These improvements encompassed enhancements in sensory function, motor function, and pain relief, along with notable advancements in bladder and bowel control. Additionally, no significant adverse effects or complications were reported during treatment.
Conclusions: Our findings suggest that repeated ECT sessions, combined with adjuvant therapies, hold promises in improving clinical outcomes for SCI patients. Further research is warranted to elucidate the optimal treatment protocols and long-term effects of this therapeutic approach.
Keywords: Neurological disorders; Paraplegia; Rehabilitation; Spinal cord injuries; Tetraplegia
Abbreviations: APRP: Autologous Platelet-rich Plasma; AIS: American Spinal Injury Association Impairment Scale; ASIA: American Spinal Injury Association; FJDT: Facet Joint Denervation Therapy; CSCI: Complete Spinal Cord Injury; CT: Computed Tomography; ECT: Epidural Catheter Therapy; ISCI: Incomplete Spinal Cord Injury; MRI: Magnetic Resonance Imaging, SCI: Spinal Cord Injury.
Introduction
Spinal Cord Injury (SCI) is characterized by damage to the spinal cord resulting from traumatic or non-traumatic causes. It is classified into two main types: complete SCI (CSCI), involving a total loss of sensory and motor function below the injury site, and Incomplete SCI (ISCI), where some sensory and/or motor function remains.
SCI occurs in two phases: the primary phase involves immediate physical damage to the spinal cord, such as contusion, laceration, or compression, leading to disruption of nerve cells, blood vessels, and tissue structure. Additionally, scarring may develop, triggered by the inflammatory response and lesion formation, potentially impeding nerve regeneration and functional recovery [1]. The secondary phase encompasses a cascade of events following the initial injury, exacerbating tissue damage and functional impairment. This phase involves inflammation, edema, ischemia, excitotoxicity, free radical formation, apoptosis, axonal degeneration, and disruption of the blood-spinal cord barrier, further contributing to neural tissue damage and neurodegeneration [2].
With over 15 million individuals worldwide affected by SCI, the condition profoundly impacts their quality of life. SCI significantly affects the physical, social, and psychological aspects of each patient. These patients suffer from paralysis, loss of sensation, and autonomic function disturbances. Moreover, patients of SCI experience chronic pain. These physical consequences also lead to secondary health complications, such as decubitus ulcers, respiratory complications, and urinalysis tract infections. Psychologically, patients are prone to experiencing anxiety and depression. Socially, social isolation and financial strains due to inability to participate in work, recreation, and social interactions as before [2]. Diagnostic methods include magnetic resonance imaging (MRI), myelography, computed tomography (CT) scans, and X-ray scans. Current conservative therapeutic approaches offer limited improvement in SCI recovery, with no established treatments. In this study, we present the outcomes of SCI patients who underwent Epidural Catheter Therapy (ECT) supplemented by adjuvant therapies such as radiofrequency therapy (RT) and facet joint denervation therapy (FJDT). Over 15 years, the therapy evolved from a single-session ECT to simultaneous cranial and caudal applications, later incorporating PRP and adjuvant therapies such as RT [3-8].
Materials & Methods
Study design and Population
This retrospective study included three patients at Speciality Center for Neurosurgery Prof und Dr Arous from 2022 to 2024 who were all previously diagnosed with complete spinal cord injury (CSCI). Inclusion criteria comprised a history of traumatic CSCI, severe sensory and motor function impairment, exhaustion of conventional therapy options, and a minimum post-injury duration of four years. The exclusion criteria were pediatric patients and non-traumatic SCI.
Clinical Evaluation & Data Collection
Patients underwent comprehensive evaluation at our facility, involving detailed medical history assessment, physical examinations, diagnostic tests, and imaging studies. A review of prior medical records provided additional insights into each patient's clinical trajectory. Regular follow-ups are allowed for continuous monitoring of patients' physical and clinical status, including CRP measurements and wound care.
Surgical Procedures
Epidural Catheter Therapy: The ECT procedure began with patients positioned in the abdominal prone position, undergoing CT-guided measurements to locate the spinal canal. Following anesthesia administration and skin sterilization, the catheter needle was meticulously inserted into the sacral canal under CT guidance. Confirmation of proper placement was ensured via control CT scans. Subsequent saline solution injection dissolved any adhesions before catheter insertion. A contrast medium was then injected, followed by anti-inflammatory, anesthetic, and anti-edematous medication administration along with autologous Platelet-Rich-Plasma (PRP). Post-procedure, patients received regular dosages through the catheter probe, with subsequent removal on the fifth day and follow-up appointments scheduled.
Radiofrequency Therapy: Like the ECT, patients of RT were positioned and underwent CT-guided measurements for precise probe placement. Sensory and motor stimulation confirmed accurate positioning before pulsed Radiofrequency initiation, followed by medication administration like that in the ECT. Post-procedure, patients received regular dosages through the catheter probe, with subsequent removal on the third day and follow-up appointments scheduled.
Facet Joint Denervation Therapy: Patients undergoing FJDT were positioned in the abdominal prone position and underwent CT-guided measurements for precise needle placement near the facet joint. Following anesthesia administration and needle confirmation via imaging, anti-inflammatory, anesthetic, and viscoelastic medication was applied to disrupt nerve function, along with PRP administration. Control CT scans were performed to assess outcomes before needle removal and post-procedure monitoring (Figure 1).
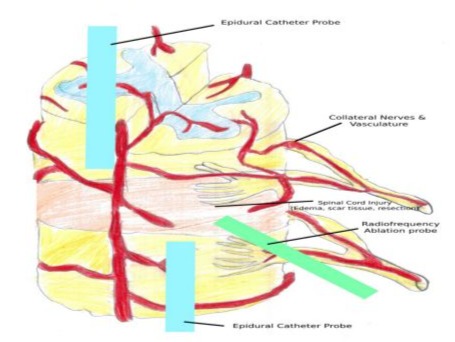
Figure 1: Arous Therapy Scheme (two epidural catheter probes are guided cranially and caudally towards the inflicted region, while a radiofrequency ablation probe is placed directly).
Case Presentation
Case 1 - Patient A: Patient A sustained a complete cervical spinal cord injury (CSCI) at the thoracic spine T8-T9 level due to a war splinter injury in 2012. MRI imaging revealed a significant spinal cord separation with atrophic changes extending from thoracic spine T5 downward, resulting in paraplegia of the lower limbs, along with urinary and fecal incontinence. In 2021, Patient A began experiencing fasciculations, muscle pain, and increased spasm in both legs, indicating a shift in neurological symptomatology. During examination, Patient A appeared fully oriented but demonstrated a complete loss of muscle strength in the lower limbs, with a grade of 0/5. Additionally, sensory deficits were noted, presenting as anesthesia bilaterally, along with flaccidity. Deep tendon reflexes were absent, and both the anal wink and bulbocavernosus reflexes were also absent. The patient reported significant bladder, bowel, and sexual dysfunction. Spasticity was graded as 1 on the Modified Ashworth Scale (MAS), indicating a slight increase in muscle tone. On November 13, 2023, percutaneous ECT was performed on T8/9 without complications. Further treatment on November 30, 2023, involved RT of the thoracic spine alongside PRP therapy. During the follow-up on February 20, 2024, the patient reported experiencing slight sensation in the right leg and transient sensation in the previously affected thoracic spine area, indicating ongoing monitoring and potential implications for the treatment approach. During a consultation on May 10, 2024, the patient reported improvement in continence and sexual function, with an estimated enhancement of more than 50%, according to the patient. Additionally, improvement in thermoception and proprioception in the left lower limb was noted. On May 14, 2024, RT was performed in the region of thoracic spine T8-T9, and during the follow-up on May 24, 2024, the patient reported further proprioceptive improvement in the left lower limb and slight improvement in the right lower limb. During the subsequent appointment on May 31, 2024, the patient underwent the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) examination, which highlighted the return of motor function in the right hallux and a delayed response in the left hallux.
Case 2 - Patient T: Patient T experienced a compression fracture and luxation of the cervical vertebrae C5-C6 in 2016 due to a swimming accident, resulting in a spinal cord contusion at the cervical vertebrae C4-C7 level and complete spinal cord resection at the C5-C6 level. This injury led to tetraplegia, accompanied by anesthesia, anhidrosis, chronic intractable pain, motor disturbance of pelvic organs, sexual dysfunction, urinary incontinence, and fecal incontinence. Upon presentation to the clinic on June 6, 2023, MRI scans revealed cervical spine misalignment, degenerative changes in the cervical vertebrae C4-C6 segment, and atrophy of the spinal cord extending from cervical vertebrae level C4 to the lower third of C7. On July 3, 2023, percutaneous ECT of the cervical spine, specifically at the C5/6 level, was performed, followed by RT at the same level with PRP on July 10, 2023. Significant alleviation of symptoms was observed during the follow-up on September 4, 2023. Additionally, the patient reported improvements in sensory function, reductions in spasticity, and the return of diaphoresis. On October 2, 2023, RT of the cervical spine, specifically at the C5/6 level, with PRP was performed. A follow-up appointment on October 10, 2023, physical examination revealed an improvement in tactile sensation in the thoracic region and upper thigh, more prominently on the right side. On January 15, 2024, ECT of the cervical spine at the C5/6 level was repeated, combined with RT and PRP. On January 25, 2024, adjuvant FJDT with PRP was performed. During the follow-up on January 31, 2024, the patient reported further improvement in delayed proprioception, more prominently in the left thoracic region. The most recent follow-up on March 25, 2024, indicated additional improvement in tactile perception of the fingers, more prominently on the right side, as well as visceral awareness of the bladder.
Case 3 - Patient V: Patient V sustained a severe spinal cord injury (SCI) in a swimming accident in 2017. The patient presented cervicobrachialgia on both sides, tetraplegia (unspecified as flaccid or spastic), chronic intractable pain, radiculopathy, and sensory disturbances in the C6, C7, and C8 dermatomes bilaterally. Additionally, the patient experienced weakness in both arms, as well as episodes of dizziness and headaches. Previous interdisciplinary therapy provided temporary relief. Examination on July 4, 2022, revealed restricted cervical spine mobility, tenderness over the cervical vertebrae and facet joints. Reflexes were absent, and spasticity was present. Anesthesia from C5 downward was noted. On August 8, 2022, percutaneous ECT of the cervical spine at level C5/6 was administered, followed by RT of the same cervical spine level on August 16, 2022. Additionally, on August 23, 2022, PRP therapy targeting the C5/6 vertebrae bilaterally was conducted. Further interventions included FJDT combined with PRP therapy targeting the cervical spine from C4/5 downward on September 1, 2022. On October 4, 2022, RT therapy was administered targeting the cervical spine at level C5/6, followed by infiltration therapy of the sacroiliac joints bilaterally on October 6, 2022. Observations on November 8, 2022, during the routine follow-up, revealed bilateral light sensory perception extending up to the upper thigh region and a notable bowel movement episode without assistance. Subsequent interventions on January 11, 2023, and April 12, 2023, focused on RT therapy targeting the cervical region. Noteworthy sensory improvements were documented on October 19, 2023, and January 23, 2024, showing sensory perception in specific nerve distributions and muscle contraction responses. These improvements included sensation in the ulnar region and complete normal sensation in the left upper limb, impaired proprioception in the ulnar region of the upper limbs, light sensation, and diaphoresis throughout the thoracic region, along with sporadic fasciculations and contractions in the upper limbs. Based on these positive developments, a recommendation was made for ECT of the cervical region combined with PRP therapy on February 12, 2024. Follow-up RT on February 20, 2024, aimed to sustain the therapeutic benefits. On May 13, 2024, a subsequent RT with PRP of the cervical region was performed. During the follow-up assessment on July 17, 2024, Patient V reported disturbed light sensations in the right digits, sparing the fifth digit, along with complete light sensation in the left ulnar region and disturbed light sensation in the remaining digits of the left upper limb. The patient also noted a return of light sensation in the feet, knees, and genital region. Most notably, the patient could consistently micturate voluntarily and reported a return of deep anal pressure sensation. On September 12, 2024, RT of the cervical region with PRP was performed and repeated on November 18, 2024. During the most recent follow-up on November 27, 2024, the patient can now rotate the wrists, elevate and abduct the shoulders, along with impaired finger flexion and extension.
Discussion
Our current findings suggest that our combination therapy, primarily consisting of ECT and RT, holds promise in mitigating the aftermath of the secondary phase in SCI while aiding in the recovery of the affected area. The precise and guided nature of our treatment approach, coupled with the combination of medications, appears to play a pivotal role in this observed effect (Table 1). By reducing swelling and adhesions, our therapy potentially facilitates the resumption of the body's natural recovery processes.
|
Sensory Function |
Motor Function |
Diaphoresis |
Bladder Function |
Bowel Function |
Sexual Function |
|
|
Patient A |
Absent from T8/9 |
Paraplegia |
Unaffected |
Incontinence |
Incontinence |
Poor (<20%) |
|
Patient T |
Absent from |
Tetraplegia |
Anhidrosis in affected area |
Incontinence |
Incontinence |
Absent |
|
Patient V |
Absent from |
Tetraplegia |
Anhidrosis in affected area |
Incontinence |
Incontinence |
Absent |
Table 1: Neurological and Autonomic Function Pre-treatment Assessments in Patients with Spinal Cord Involvement.
The secondary phase of SCI is characterized by a cascade of events, including inflammation, edema, ischemia, excitotoxicity, and apoptosis, which exacerbate tissue damage and functional impairment. Our combination therapy offers a targeted and multifaceted approach to address these challenges. ECT, through its direct delivery of medications to the epidural space, can effectively target inflammatory processes and reduce tissue edema. Meanwhile, RT provides neuromodulation and stimulation to promote neural regeneration and functional recovery. By synergistically combining these therapies, we aim to address both the acute and chronic consequences of SCI, leading to improved clinical outcomes for our patients. While our findings are promising, it is important to acknowledge the limitations of our study, including its small sample size, retrospective design, and lack of a control group. Additionally, the heterogeneity of interventions and variability in treatment response among patients may influence the generalizability of our results (Table 2). Future research efforts should focus on larger, prospective studies with longer follow-up periods to further elucidate the efficacy and mechanisms of action of our combination therapy approach.
|
|
Sensory Function |
Motor Function |
Diaphoresis |
Bladder Function |
Bowel Function |
Sexual Function |
|
Patient A |
Improved tactile sensation, thermoception and proprioception |
Improved, 3/5 muscle grade in L5 and S1 region |
Unaffected |
Improved (>50%) |
Improved |
Improved (>50%) |
|
Patient T |
Improved tactile sensation, thermoception and proprioception |
No improvement |
Hypohidrosis |
Improved |
Improved |
No improvement |
|
Patient V |
Improved tactile sensation, thermoception and proprioception |
Improved, 3/5 muscle grade from C6-T1 regions |
Hypohidrosis |
Improved |
Improved |
No improvement |
Table 2: Post-Intervention Changes in Neurological and Autonomic Function Across Patients.
Conclusion
The therapies and techniques employed in our study show promise in the treatment of SCI patients, particularly due to their minimally invasive nature, significantly reduced risks compared to macro surgeries, and repeatability. All patients who received the combination of therapies reported improvements in tactile sensation, proprioception, and autonomic functions. While our findings are encouraging, further research and the implementation of novel, albeit experimental techniques, are necessary to address the challenges posed by the primary phase of SCI. Rehabilitating astrogliosis and addressing the initial injury cascade could prove immensely beneficial in SCI therapy. It remains to be seen whether the therapeutic benefits of our interventions will reach a plateau over time.
In conclusion, our study underscores the potential of combination therapies in improving outcomes for SCI patients. Continued efforts to refine and optimize these approaches, along with the exploration of new treatment modalities, are essential to advancing the field of SCI rehabilitation and enhancing the quality of life for individuals living with this debilitating condition. OR In conclusion, our study provides preliminary evidence supporting the effectiveness of combination therapy involving ECT and RT in mitigating the secondary phase of SCI and promoting recovery. Continued research in this area holds the potential to significantly impact the management and rehabilitation of individuals with SCI, ultimately improving their quality of life and functional outcomes.
References
- Fleming JC, Norenberg MD, Ramsay DA, Dekaban GA, Marcillo AE, et al. (2006) The cellular inflammatory response in human spinal cords after injury. Brain 129: 3249-3269.
- David S, Kroner A (2011) Repertoire of microglial and macrophage responses after spinal cord injury. Nat Rev Neuroscience 12: 388-399.
- Gadot R, Smith DN, Prablek M, Grochmal JK, Fuentes A, et al. (2022) Established and emerging therapies in acute spinal cord injury. Neurospine 19: 283-296.
- Schwab ME, Bartholdi D (1996) Degeneration and regeneration of axons in the lesioned spinal cord. Physiological Reviews 76: 319-370.
- Torregrossa F, Sallì M, Grasso G (2020) Emerging therapeutic strategies for traumatic spinal cord injury. Pine Health Special Section 11: 283.
- Arous MM, Arous IM, Alwani M, Daise MA, Haki B, et al. (2023) EpiduralSteroids Injection: A Mini Review 14: 2023.
- Arous MM, Arous IM, Alwani M, Daise MA, Haki B, et al. (2023) EpiduralSteroids Injection: A Mini Review 14: 2023.
- Arous MM (2023) BOOK: Minimal Invasive Procedure in Neuro-Spine-Surgery 2023.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.