Endoscopic Total Extraperitoneal Mesh Repair of Spieghelian Hernia - A Case Report and Case Series of 19 Patients with Review of the Recent Literature
by Leweke Rhea*, Schill Corbinian, Glatze Joerg
Department of General Surgery, Klinik für Allgemein- und Viszeralchirurgie, Mainaustr. 35, 78464 Konstanz, Germany
*Corresponding author: Rhea Leweke, Department of General Surgery, Klinik für Allgemein- und Viszeralchirurgie, Mainaustr. 35, 78464 Konstanz, Germany
Received Date: 25 July 2025
Accepted Date: 29 July 2025
Published Date: 31 July 2025
Citation: Rhea L, Corbinian S, Joerg G. (2025). Endoscopic Total Extraperitoneal Mesh Repair of Spieghelian Hernia - A Case Report and Case Series of 19 Patients with Review of the Recent Literature. Ann Case Report. 10: 2355. https://doi.org/10.29011/2574-7754.102355
Abstract
Due to the low incidence of Spieghelian Hernias, no standardized surgical procedure has been universally recommended to date. In this article, we describe an endoscopic total extraperitoneal (TEP) mesh repair technique for Spieghelian Hernia, which we performed in 19 patients between 2017 and 2025. In our experience, this technique offers advantages over alternative approaches, particularly in terms of safety and patient satisfaction.
Keywords: Spieghelian Hernia; Abdominal wall hernia; Total extraperitoneal (TEP) technique; Minimally invasive hernia treatment.
Introduction
The Spieghelian Hernie, located at the junction of the semilunar line and the arcuate line (Figure 1a), has an incidence of 0.11 percentage of all abdominal wall hernias [12]. There is no established standardized surgical procedure for the repair of Spieghelian Hernias [1, 10]. In this article, we describe an endoscopic total extraperitoneal (TEP) mesh repair technique for Spieghelian Hernia (SH), which we performed in 19 patients between 2017 and 2025 in our clinic. In our experience, minimally invasive TEP approach offers advantages over alternative approaches especially over open surgery, particularly in terms of safety and patient satisfaction.
Exemplary case presentation and results of the case series
The first patient in our series was a 64-year-old, Caucasian male of normal weight (BMI 21.9 kg/m²), who presented with movementdependent pain in the lower left quadrant of the abdomen. The pain had initially been attributed to muscular irritation in the context of a recent pneumonia, which had also led to a weight loss of 12 kg. Apart from a hip endoprosthesis, the patient had no history of chronic illness or prior abdominal surgeries.
On physical examination, the patient presented with localized pain and a palpable bulge at the level of the left anterior superior iliac spine. A computed tomography (CT) scan confirmed the clinical suspicion of a Spieghelian hernia. Incarceration of bowel loops was excluded (Figure 1b).
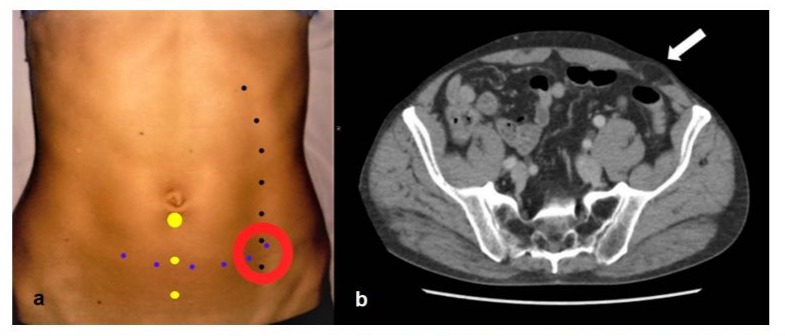
Figure 1: a. anatomical landmarks: black dotted line: semilunar line; blue dotted line: arcuate line; red circle: typical localisation of SH; yellow dots: trocar position. b. CT scan showing a SH with prolapsed preperitoneal fat (arrow).
Manual reduction of the hernia was achieved under analgesia. An early elective surgical repair was scheduled using a TEP approach, following the protocol we typically use for the minimally invasive extraperitoneal inguinal hernia repair.
The procedure was performed with the patient in the supine position under general anaesthesia. Prophylactic antibiotics were administered as a single 1.5 g dose of cefuroxime.
The laparoscopic tower was positioned on the side of the hernia, with the surgeon and assistant standing on the contralateral side. The initial infraumbilical incision was made, and the left rectus muscle was lateralized to allow blunt dissection of the preperitoneal space along the midline, thus minimizing the risk of injury to the epigastric vessels. A Hasson trocar was inserted, and a preperitoneal pneumodissection was established at an insufflation pressure of 12 mmHg. Under direct visualization using a 30° laparoscope, two additional 5 mm trocars were placed: one 5 cm inferior to the camera port, and another 4 cm superior to the pubic symphysis along the midline, in accordance with the standard TEP technique (Figure 1a).
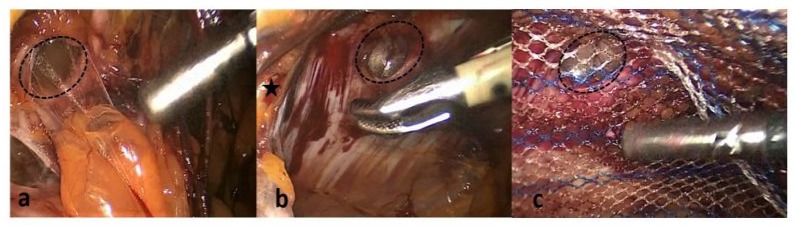
Dissection of the arcuate line and semilunar line (linea Spiegheli) revealed herniated preperitoneal fat in the typical location (Figure 2a). The peritoneum was dissected cranially to the defect to create sufficient space for mesh implantation. The hernia contents were reduced (Figure 2b).
A 15 × 10 cm polyglecaprone-25/polypropylene composite mesh (Ultrapro, Ethicon, J & J) was inserted, providing at least 5 cm overlap in all directions over the 1 × 1 cm defect. To prevent early mesh displacement, two resorbable synthetic straps (Secure Strap, Ethicon J&J) were used to fix the mesh medially and cranially. Final inspection confirmed optimal, tension-free placement of the mesh, which remained stable upon deflation of the pneumopreperitoneum (Figure 2c).
The patient was mobile and pain-free with low-dose NSAIDs immediately after surgery and was discharged.
Three weeks postoperatively, the patient reported mild discomfort medial to the original hernia site, most likely due to the fixation straps. In ultrasound, the mesh was in the correct position without any sign of seroma or hematoma.
At the routine follow-up three months after surgery, the patient reported full mobility without pain, even during regular physical activity. Wound healing was uneventful. Ultrasound still showed correct mesh position. Two years postoperatively, the patient remained asymptomatic and free of recurrence.
Over the subsequent eight years, we performed the same minimally invasive TEP procedure on 19 patients with Spieghelian hernia, aged 46 to 86 years (median 69 years). In ten cases, SH was located on the left side, in nine on the right. Four patients underwent simultaneous minimally invasive TEP repair of an inguinal hernia, two others of an umbilical hernia, one with suture, the other one with sublay mesh repair. One patient had a laparoscopic tubal ligation after the hernia repair.
All Patients were evaluated three months to two years after surgery using the Herniamed Quality Assurance Study follow-up questionnaire (Herniamed, Berlin, Germany).
Two patients reported mild pain during physical activity, which resolved three months after surgery. The patient, who underwent sublay mesh repair of an umbilical hernia, developed a small postoperative umbilical hematoma. At the most recent follow-up, all patients reported no chronic pain or hernia recurrence.
Discussion
SH was first described in 1764 by J. Klinkosch as a rare abdominal wall hernia occurring at the intersection of the arcuate line and the semilunar line [4]. The condition is named after Adriaan van den Spieghel, a Belgian anatomist who identified the transition from muscle to aponeurosis in the transversus abdominis muscle, later termed the semilunar line (Linea Spiegheli) (Figure 1a). The Spieghelian fascia - the origin site of the hernia - is defined as the aponeurosis of the transversus abdominis, bounded medially by the lateral edge of the rectus muscle and laterally by the semilunar line.
Due to its rare occurrence and often vague symptoms, SH diagnosis is frequently delayed, resulting in a relatively high complication rate [5, 11]. Accordingly, current literature includes only a few studies focused on this hernia and its treatment. One of the few retrospective analyses with long-term follow-up was published by Larson and Farley in 2002. Among 76 cases, only one was treated with a laparoscopic technique [5].
In the same year, Moreno-Egea recommended endoscopic total extraperitoneal repair for small, non-incarcerated SHs in a retrospective randomized study of 22 patients [8,9]. However, in 2015, he proposed laparoscopic intraperitoneal onlay mesh (IPOM) repair as the gold standard for SH, citing easier execution and marginally lower material costs, with similar outcomes in morbidity and patient satisfaction [7]. In that study, surgical technique (minimally invasive versus open surgery) was selected based on the size and location of the hernia, which limits generalizability. Thus, we question whether IPOM can be recommended as the gold standard for all SH repairs, since we have shown in our case series of 19 patients, that all patients were sufficiently treated by a minimally invasive extraperitoneal procedure.
In 2011, F. Mainik introduced a hybrid extraperitoneallaparoscopic approach [6]. While combining the benefits of TEP and laparoscopy, this technique may be especially useful when bowel incarceration is suspected and intra-abdominal inspection is necessary. However, laparoscopy inherently carries a risk of bowel injury. Additionally, peritoneal perforation can impair visualization during preperitoneal dissection due to insufflated air separating tissue planes. Therefore, we do not consider this hybrid approach suitable as a standard method for SH repair.
The minimally invasive TEP technique remains the least studied approach for SH [7]. In our series, we used the same polyglecaprone 25/polypropylene composite mesh that we employ for inguinal hernia TEP repairs. In inguinal hernia repair, mesh fixation is typically omitted, following current European Hernia Society guidelines [2], whereas it is usually used in other ventral hernia repair [3]. However, in SH repair, we chose to fix the mesh craniomedially using resorbable straps. Unlike the inguinal region, the area surrounding SH is not enclosed by stable anatomical structures, increasing the risk of early mesh displacement before the preperitoneal space fully re-adheres. Careful attention must be paid to avoid injuring nearby nerves and vessels during fixation.
Midline trocar placement proved most effective, as it provides sufficient working distance for dissection, hernia reduction, and mesh positioning from an optimal angle. If conversion to intraperitoneal laparoscopy becomes necessary, the same trocar sites can be used without modification.
Conclusion
In summary, we consider minimally invasive TEP mesh repair to be a safe and feasible option for the treatment of uncomplicated Spieghelian hernia. Patient satisfaction and clinical outcomes appear promising. For irreducible or incarcerated hernias, conversion to laparoscopy can be performed easily. Further studies are warranted to assess TEP repair in larger cohorts and to explore variations in mesh positioning, fixation techniques, or the use of self-adhering meshes in optimizing surgical outcomes.
Conflict of Interests
The authors declare that there is no potential conflict of interest that could have influenced the results or interpretations presented in this manuscript.
References
- Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, et al. (2014). Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)-part 1. Surg Endosc; 28: 2-29.
- Bittner R, Montgomery MA, Arregui E, Bansal V, Bingener J, et al. (2014). Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society). Surg Endosc; 29: 289-321.
- Earle D, Roth JS, Saber A, Haggerty S, Bradley 3rd JF, et al. (2016). SAGES guidelines for laparoscopic ventral hernia repair. Surg Endosc; 30: 3163-3183.
- Klinkosch JT. (1964). Divisionem herniarum novamque hernia ventralis proponit. Dissertationum Medicorum. 1764: 184.
- Larson DW, Farley DR. (2002). Spigelian hernias: repair and outcome for 81 patients. World J Surg; 26: 1277-1281.
- Mainik F, Flade-Kuthe R, Kuthe A. (2011). Combined endoscopic treatment of Spigelian hernia: laparoscopy - total extraperitoneal patch plasty - laparoscopy. Chirurg; 82: 934-945.
- Moreno-Egea A, Campillo-Soto A, Morales-Cuenca G. (2015). Which should be the gold standard laparoscopic technique for handling Spigelian hernias? Surg Endosc; 29: 856-862.
- Moreno-Egea A, Carrasco L, Girela E. (2002). Open vs laparoscopic repair of spigelian hernia: a prospective randomized trial. Arch Surg; 137: 1266-1268.
- Moreno-Egea, A Torralba, JA Aguayo (1999). Totally extraperitoneal laparoscopic repair of spigelian hernia. Eur J Coeliosurg. 3283-3284.
- Silecchia G, Campanile FC, Sanchez L (2015). Laparoscopic ventral/ incisional hernia repair: updated Consensus Development Conference based guidelines [corrected]. Surg Endosc; 29: 2463-84.
- Spangen L. (1989) Spigelian hernia. World J Surg; 13: 573-580.
- Shrestha G, Adhil I, Adhikari SB, Ranabhat N, Ghimire B. (2023). Spigelian hernia: A rare case presentation and review of literature. Int J Surg Case Rep. 105: 108079.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.