Endoscopic Dacryorhinostomy Surgical Intervention Method at the “Albanian Eye Center”
by Orjeta Tonuzi1*, Ali Tonuzi2,Evis Bendo1
1Mother Theresa University Hospital Center, Tirana, Albania
2Associate Professor, Mother Theresa University Hospital Center, Faculty of Medicine, Tirana, Albania
*Corresponding author: Orjeta Tonuzi, Mother Theresa University Hospital Center, Tirana, Albania.
Received Date: 29 April, 2025
Accepted Date: 05 May, 2025
Published Date: 08 May, 2025
Citation: Tonuzi O, Tonuzi A, Bendo E (2025) Endoscopic Dacryorhinostomy Surgical Intervention Method at the “Albanian Eye Center”. Ophthalmol Res Rep 09: 10165. https://doi.org/10.29011/2475-5605.110165
Abstract
Chronic dacryocystitis is an infection of the lacrimal sac due to blockage of the nasolacrimal duct, which includes two types: congenital blockage and acquired blockage. The main symptom of nasolacrimal duct blockage is “Epiphora”, which is a tear drainage disease and is caused as a result of anatomical and functional disorders. Congenital blockage of the lacrimal drainage system generally occurs from the membranous valve of Hasner, which covers the end of the nasolacrimal duct. Acquired blockage is caused by nasal-orbital trauma, chronic sinusitis, rhinitis, nasal polyps, septal deviation, neoplasms of the lacrimal sac, and concomitant dacryocystitis.
For many patients with nasolacrimal duct obstruction, their treatment is done with surgical intervention, and this type of intervention is called Dacryocystorhinostomy (DCRS). This type of surgical intervention is done to manage Epiphora as best as possible. This is a procedure that consists of creating a new communication of the lacrimal sac with the nasal cavity. Surgical indications of this nature include: persistent tear flow, recurrent dacryocystitis, recurrent mucous discharge, and painful distension of the lacrimal sac.
Over a 4-year period (2019-2024), 174 patients were treated with the Endoscopic Dacryorhinostomy (DCRS) method, achieving positive results in 157 patients (90%) of the cases in which no recurrence was observed.
The placement of a silicone tube was requested and performed in 23 patients (13%) of the cases, while in 151 patients (87%) of the cases, the silicone tube was not placed. The time of control of the patients ranged from one week to one year. During this period, 161 patients presented with full passage of saline in the lacrimal test, while in 11 patients the saline passed with difficulty, and in 2 patients the saline did not pass at all.
The treatment of the patients was carried out by applying the Endoscopic Dacryorhinostomy (DCRS) method, which resulted in success in 92.5% of the cases-patients treated and analyzed.
Keywords: Dacryocystitis; Surgical intervention; Endoscopic tearing and direct stimulation of the lacrimal gland; and b] dacryorhinostomy; etc. Epiphora, which is decreased tear drainage and can be caused by diseases of the lacrimal system.
Introduction
Symptoms of ocular drainage disorders affect ocular function, ocular health, and social function. A thorough understanding of the lacrimal system is essential to understanding the physiology of tear flow. The lacrimal system has two functions: a] Hyperlacrimation, which is increased tear production and can be caused by reflex tearing and direct stimulation of the lacrimal gland; and b] Epiphora, which is decreased tear drainage and can be caused by diseases of the lacrimal system.
The causes of Epiphora are generally: Punctal anomalies, stenosis, ectropion, and punctal agenesis. However, other causes of Epiphora include lacrimal pump dysfunction, eyelid ptosis, orbicularis oculi muscle weakness, canalicular stenosis, and lacrimal duct obstruction [1,2].
Epiphora, as a result of nasolacrimal duct obstruction, is classified into three degrees:
Grade 1: Temporary external Epiphora caused by cold and windy weather;
Grade 2: Permanent external Epiphora;
Grade 3: Temporary internal and external Epiphora.
The diagnosis of Epiphora is made based on: Patient history, external examination and palpation, evaluation of punctures and probing. Additional radiological examinations such as contrast dacryocystography, scintigraphy and magnetic resonance imaging are often required to evaluate the lacrimal ducts [3] Figures 1 and 2.
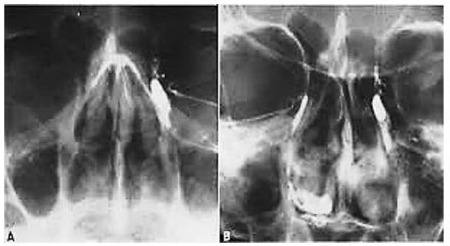
Figure 1: Contrast Radiography of the lacrimal duct.
In cases of nasolacrimal duct obstruction, endoscopic surgical intervention is necessary and should be performed, according to the Endoscopic Dacryocystorhinostomy (DCRS) method, which consists of creating a communication between the lacrimal sac and the nasal cavity to enable tear drainage. Endoscopic DCRS surgery has several obvious advantages compared to external surgery.
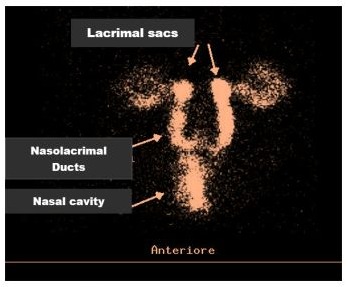
Figure 2: Scintigraphy of the lacrimal paths.
a) This type of surgery does not allow the formation of cicatrices on the skin; b) it allows for the simultaneous correction of nasal pathologies; and c) it does not damage the medial canthus since it preserves the pump mechanism of the orbicularis oculi muscle and is valuable in facilitating the performance of revision surgeries.
In our surgical practices, we have generally applied the indications for performing Endoscopic Dacryocystorhinostomy (DCRS) in these cases:
- In cases where Epiphora is caused by anatomical obstruction of the sac or nasolacrimal duct: as in cases of chronic dacryocystitis with leakage of purulent secretions, inflammation of the skin over the lacrimal sac, in cases of the medial canthus region, traumatic injuries of the nasolacrimal duct, in dacryolithiasis as well as in cases of dacryocele with benign mass of the lacrimal sac.
- Even in cases of dry eye syndrome, we have not performed surgical interventions for chronic Epiphora that are the cause of obstruction of the sac above the level and have also created facial nerve paralysis with lagophthalmos and ectropion of the lower eyelid in some of our elderly patients examined with malignant tumors of the lacrimal system.
Endoscopic Dacryocystorhinostomy (DCRS) has its advantages and disadvantages compared to external Dacryocystorhinostomy (DCRS).
Among the most obvious and highly effective advantages of endoscopic dacryocystorhinostomy we can mention:
- provides a better aesthetic effect and no cicatrices;
- provides a single operation while simultaneously
correcting nasal pathologies such as DSN or
- chronic sinusitis, which may be the cause of obstruction;
- avoids damage to the medial canthus and preserves the pump mechanism of the orbicularis oculi muscle;
- Active infection of the lacrimal system is not a contraindication for surgery and there is less bleeding during the intervention.
One of the most common disadvantages of Endoscopic Dacryocystorhinostomy (DCRS) surgery is listed below:
# requires specialized training in endonasal endoscopic surgery, and the endoscopic tools needed for the surgery are more expensive.
This type of surgical procedure is performed in this way: Initially, we place 2% lidocaine-soaked tampons in the nose one hour before the operation. Then, we pretreat the patient with Diazepam 5 mg/ ml for 30 minutes before the procedure. A rigid endoscope (0-30 degrees) is usually used to perform endoscopic surgery. Initially, the concha media and the maxillary line opposite it are identified. The surface opposite the maxillary line is the area of the lacrimal sac. The lacrimal sac is covered by the lacrimal bone, which is removed during Endoscopic Dacryocystorhinostomy (DCRS) surgery. In the following steps, infiltration with 2% lidocaine is performed by adding adrenaline (1:100.000) to the mucosa of the surface of the lacrimal bone, and also the concha media, since it is a very sensitive part when touched. Cauterization of the nasal mucosa is performed at the level of the lacrimal sac. We expose the lacrimal bone by removing the cauterized mucosa to expose the entire surface of the lacrimal bone. We remove the lacrimal bone with Carrison forceps, and begin its removal at the maxillary line of the lacrimal bone. After making a small opening, we press the lacrimal sac from the outside and endoscopically observe the movement of the medial wall of the lacrimal sac. We expand the newly created stoma as much as possible. Then we carefully moisten and rinse the lacrimal passages with physiological solution.
A vertical incision is made in the lacrimal sac, and the newly created stoma of the sac is expanded. The cannula is inserted through the canaliculus system to exit into the nasal cavity, checking the patency of the stoma. Finally, the sac is carefully washed, allowing the saline solution to freely drain, which indicates a successful surgery [4]. Then, a light unilateral tamponade of the nasal cavity on the side where the surgery was performed is performed. As a rule, the patient leaves the surgical clinic approximately one hour after the end of the intervention. The tampon is removed after 24 hours. In the postoperative period, the patient is given oral therapy with antibiotics for one week, analgesics, and saline spray for 1 week to 3 months, nasal decongestants for one week, and antibiotic eye drops for 10-15 days. Canalicular testing is performed on the day the nasal packing is removed, and then 1-4 weeks later, and also 3 months after surgery. In cases where the patient has had a silicone tube inserted, it should be kept for several weeks, and various authors recommend keeping it for 2-12 weeks for adults and 10-12 weeks for children [5, 6].
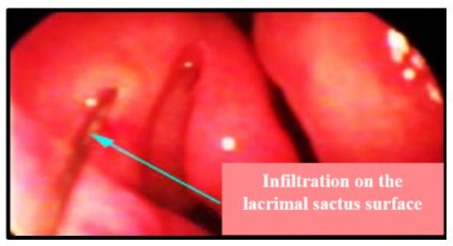
Figure 3: Infiltration at the mucose of the lacrimal sactus in the surface and media concha.
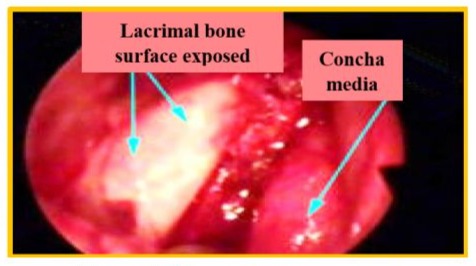
Figure 4: Whole lacrimal bone surface exposed.
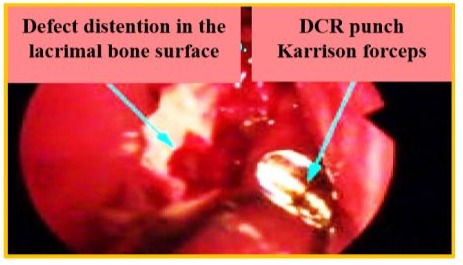
Figure 5: Lacrimal Osteotamia.
Materials and Methods
Our reported study on Endoscopic Dacryorhinostomy (DCRS) was conducted during a period of 2019-2024, at the “Albanian Eye Center” Clinic, where 174 patients with nasolacrimal duct obstruction were examined and treated.
Our reported study aimed to implement endoscopic surgical treatment protocols for chronic dacryocystitis, as a result of nasolacrimal duct obstruction, which was the main goal of this study.
The study included two groups of patients: the first group included 174 patients, those who would be treated at the “Albanian Eye Center” Clinic, Tirana, and the second control group consisted of 157 patients with chronic dacryocystitis who underwent external DCR at the University Hospital Center “Mother Theresa”, Tirana during the same period.
The patients were distributed a questionnaire specially prepared for the study and which contained the following specific requirements:
a) Demographic profile (Name, surname, age, gender, residence, place of work); b) Socio-economic status; c) Main complaints which included eye examination, regurgitation test (emptying from the back) and canalicular test.
The collected data were systematized and analyzed for each of the patients of both groups prospectively, concluding for each of them, according to the observations made. The collected data were analyzed with the statistical program SPSS version 19.0. Categorical variables are presented in percentage (%) and number of cases. In the tables and graphs presented, the data are visualized, considering that the value of P ≤ 0.05 is statistically significant.
Results
The study included 174 patients with nasolacrimal duct obstruction who were currently being treated at the “Albanian Eye Center” Clinic, Tirana.
|
Patients of treatment group |
Age (year) |
|
Study cases number |
174 |
|
Position |
66 |
|
Minimum |
16 |
|
Maximum |
82 |
|
Average |
49,17 |
|
Standard deviation |
15,791 |
|
Variance |
249,365 |
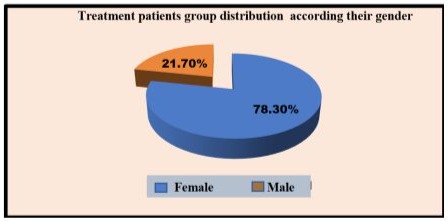
Graph 1: Treatment patients group distribution according to their gender.
These patients who presented with nasolacrimal duct obstruction underwent surgical intervention using the Endoscopic Dacryorhinostomy (DCRS) method.
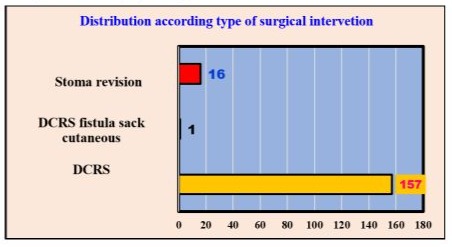
Graph 2: Patients distribution according to their type surgical intervention.
According to the Graph 2, we observe that out of the total number of patients (174) in the first treated group, approximately 157 (90.2%) case-patients underwent surgical intervention with the Endoscopic Dacryorhinostomy (DCRS) method, in 1 patient the Endoscopic Dacryorhinostomy (DCRS) method with cutaneous fistula of the scrotum was applied, and in 16 patients the Endoscopic Dacryorhinostomy (DCRS) method with stoma revision was applied.
The distribution by type of intervention, surgery, and operated eyes is presented in Graph 3.
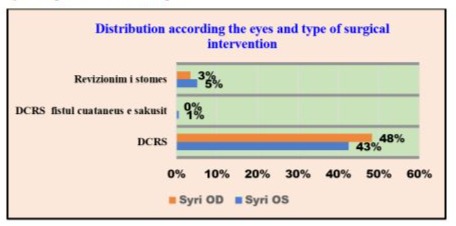
Graph 3: Distribution according to the type of surgical intervention and operated eyes in %.
According to the data in Graph 3, we observe the Endoscopic Dacryorhinostomy (DCRS) method predominates in 48% of patient-cases. In our treated patients, stoma revision was also performed in 5% of patient-cases. From the analysis of the above data, no significant correlation was found between the operated eye and the type of operation.
Graph 4 shows the tear duct damage that occurred in both the left and right eyes.
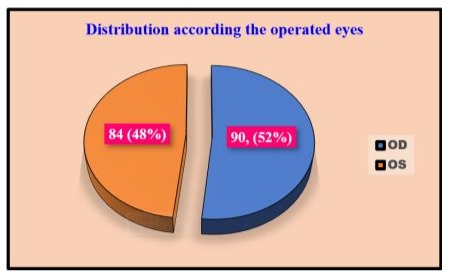
Graph 4: Distribution according to the operated eyes.
According to Graph 4, it is shown that in 90.52% of the patient cases, surgical interventions were performed on the right eye, while in the left eye, the surgical interventions were performed in 84.48% of the patient-cases. The differences between surgical interventions according to the respective eyes do not result to be significant.
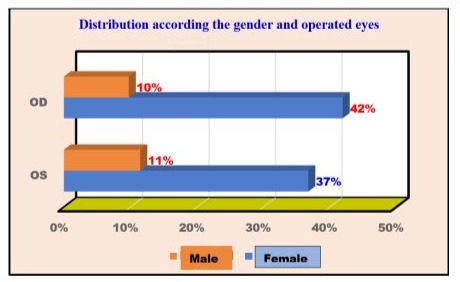
Graph 5: Surgical intervention in both eyes according to the gender of the patients.
Surgical interventions on the eyes of patients were performed on both men and women; the data are given in Graph 5. According to the graph 5, we observe about 52% of women and men were operated on in the right eye, and 48% of women and men in the left eye. From the statistical analysis according to the collected and reported data, no meaningful relationship or odds ratio was observed, which appeared between these two variables.
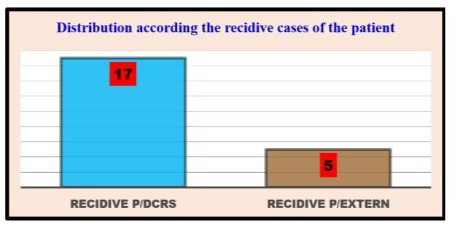
Graph 6: Recidivistic cases of the lacrimal duct blocked according to the Endoscopic DCRS.
After surgical interventions, recurrence of lacrimal duct obstruction was observed in some patients, which was observed only in 5 cases after external Endoscopic Dacryorhinostomy (DCRS) and in 17 cases of recurrence after Endoscopic Dacryorhinostomy (DCRS), data which are reported in Graph 6.
In the surgical interventions for stoma revision, silicone tube placement was performed, and from the cases of interventions, it resulted only in 23 (13%) of the patient-cases, silicone tube placement was used, a fact that indicates its rare use, at the same time, the positive and advantageous benefits from its non-use, data which are reported in Graph 7.
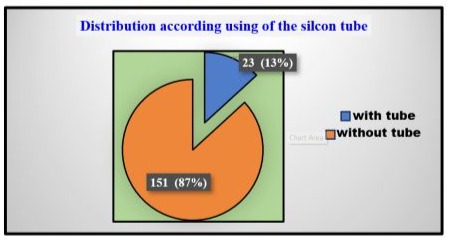
Graph 7: Using of silicon tube for secretions discharge.
With the highest number of surgical interventions according to diagnosis, patients in the first group were treated with the Endoscopic Dacryorhinostomy (DCRS) method in 142 of all cases. This distribution according to diagnosis and type of surgery is presented with the data in Graph 8.
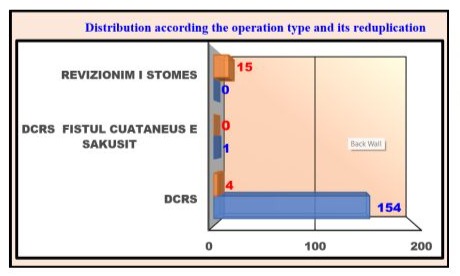
Graph 8: Type of surgical intervention and its duplication
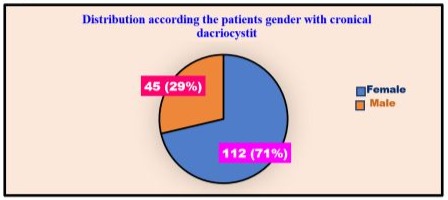
Graph 9: Distribution according to the gender of the control group of patients.
Patients from the second control group underwent surgical intervention in both the left and right eyes, data which are presented in Graph 10.
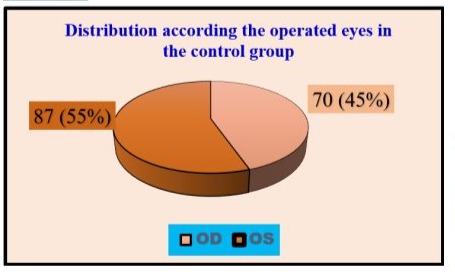
Graph 10: Distribution of the operated eye cases in the control group.
This graph shows, about 87 (55%) of the patient-cases underwent surgery on the left eye and 70 (45%) of the patient-cases underwent surgery on the right eye compared to the control group patients.
After surgery, approximately 130 (83%) of the patients in the control group had a silicone tube placed for operation, data which are presented in Graph 11.
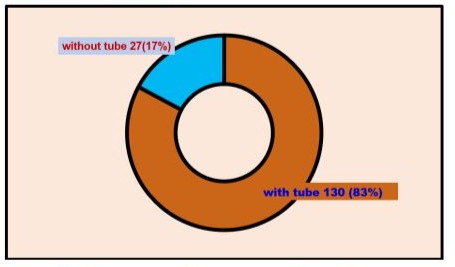
Graph 11: Distribution of the cases according to the use of the silicon tube in the control group.
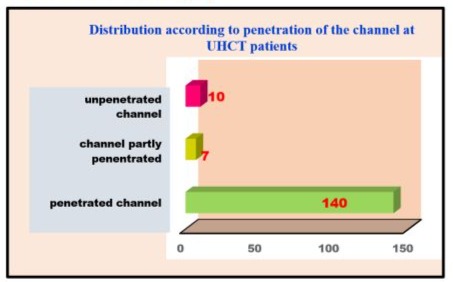
Graph 12: Distribution of the patients according to the practicability of the channel.
The permeability through the canal was found in approximately 140 patient-cases, values that are similar to the cases of the first group of treatment using the Endoscopic Dacryorhinostomy (DCRS) method, the data are presented in Graph 12.
Table 2 presents the odds ratios of patency through the canal depending on the type of surgical intervention, the data of which cases are expressed in %, and where values of P < 0.001 are significant.
|
Opportunity of the permeability through channel |
DCR externe |
DCRS |
Percentage differences |
P-values |
|
Penetrated channel |
89.2% |
92.5% |
3.4% |
0.001 |
|
Partly penetrated channel |
4.5% |
6.3% |
1.9% |
0.001 |
|
Unpenetrated channel |
6.4% |
1.1% |
5.2% |
0.001 |
Table 2: The rate of permeability through the channel according to the logistical decrease.
Discussion
During our 4-year study, 174 patients aged 16-82 years were randomly selected from the first study group, of which 78.3% of the cases were female patients, compared to 21.7% who were male patients. While from the second control group, approximately 112 (71.3%) of the case-patients were female and 4 (28.7%) of the case-patients were male.
According to the literature studied by us on the occurrence of primary acquired nasolacrimal duct, it is most often observed in women. Other previous studies report that the bony canal of the nasolacrimal duct in the minimum acceptable (normal) norm is encountered in women. This anatomical and natural characteristic in patients is considered responsible for the development of PANDO [5]. Our study is consistent with the data of authors Codere, Denton, and Corona, who refer to the same percentages regarding the dominance of the female gender in this pathology [7-9] This phenomenon is explained by the fact that women have a narrower anatomical structure of the nasolacrimal duct compared to men.
The presentation of patients in our clinic has been uniform and alternating in the first 7-12 months from the onset of tear flow in 27% of patient-cases, and continuing for 1-3 years in 24% of patient-cases, but at the same time we have had over 10 years of tear flow in 3.4% of all patient cases.
All patients treated by us have had nasolacrimal duct obstruction and of these 157 patients have undergone surgical intervention with the Endoscopic Dacryorhinostomy (DCRS) method, and only in 1 case there was nasolacrimal duct obstruction and fistulacutaneous and in this case the patient has undergone Endoscopic Dacryorhinostomy (DCRS) and fistulectomy and 16 patient cases have undergone stoma revision. Of the 174 patients operated on by the staff of the “Albanian Eye Center” Clinic, Tirana, about 157 (90%) patients underwent surgical intervention for the first time, of which, 4 patients who underwent the intervention using the Endoscopic Dactylinostomy (DCRS) method did not have recurrences, while 10 (10%) patients had recurrences and of these 5 patients with recurrences, they were post-external Dactylinostomy.
We performed the placement of the silicone tube in 23 (13%) patients, while in 151 (87%) patients, the silicone tube was not placed. As for surgical interventions in the second control group, 130 (83%) patients had the silicone tube placed, and in 27 (17%) patients, the silicone tube was not placed. Significant differences were observed between the first treatment group and the second control group regarding the placement of the silicone tube, as the values of P < 0.002. Not placing the silicone tube has two positive sides: firstly, it reduces the cost of the operation, and secondly, it reduces the duration of the surgical intervention.
Of the 174 patients examined endoscopically, 21 patients were found to have nasal pathology, which is sometimes associated with chronic dacryocystitis, 17 patients with Dactylocystostomy, 1 patient with hypertrophy of the nasal concha, 1 patient with bullous inferior concha, 1 patient with allergic rhinitis and only 1 patient with synechiae from previous nasal surgeries.
Referring to studies conducted by other authors such as Rice, Umer. et al. they have shown approximately the same values for nasal pathology in patients treated with the Endoscopic Dactylocystostomy (DCRS) method [10].
From our study, approximately 143 (82%) patients from the first treatment group resulted with the diagnosis of chronic dacryocystitis, 17 (10%) patients with the diagnosis of recurrent dacryocystitis, 8 (5%) patients with the diagnosis of sac phlegmon and 4 (2%) patients with the diagnosis of sac hydrops. During the check-up periods of 1 week, 1 month to 1 year, it was found that: about 161 of the patient-cases presented with complete patency of the canal, while in 11 patient-cases partial patency was found, and in only 2 cases the canal was blocked.
The treatment of our patients with the Endoscopic Dacryocystectomy (DCRS) method resulted in a very effective success rate of up to 92.5% of the patients, which is consistent with the results achieved by the author Umer, et al. a value of approximately 75-95% [9,6]. Meanwhile, the success rate for the cases of the second control group with the external dacrocyte method resulted in 89.2%, a comparable result achieved by the author Kanski Jack J., who reports a success rate of 87.5%, while another author Andre Aroni., reports success rates of 98% [11,12]. The above methods, also referred to as studies by other foreign authors, as well as the results achieved by us, significantly improve the symptoms of lacrimal obstruction, such as Epiphora and local inflammation. The positive results achieved by us are both achievements and advantages of the development of methods and the use of coherent surgical instruments, the use of endoscopic devices during surgical interventions, as well as the professional surgical experiences of the specialist surgeon doctor [13,14].
Conclusions
The results achieved by our study, with the data collected, processed, and analyzed with the statistical program SPSS version
19.0, according to categorical variables presented in percentage (%) and number of cases-patients, lead us to the following conclusions:
Surgical interventions with the Endoscopic Dactrinoscopy (DCRS) method reported by us and foreign authors is a new contemporary and valid method, since according to the results achieved by this study it shows and demonstrates a high degree of success for the management of cases presented in patients with nasolacrimal duct obstruction.
Endoscopic Dactrinoscopy (DCRS) as a contemporary method is less invasive, preserves the anatomical structures of the nasal cavity, shortens the time of surgical intervention and at the same time achieves rapid recovery of the patient, which makes this method the most selected in the daily practices of clinical surgical interventions.
The results achieved by surgical interventions to patients operated by two groups: the first group, the treatment group, and the second group, the control group, by means of this method and realized by us, are in considerable percentages and almost the same as those achieved by other foreign researchers referred to in contemporary literature, and undoubtedly constitute a successful achievement in this scientific-practical study.
Plagiarism: The study reported was designed and written by the authors, presenting a significant contribution with an effort to ensure that the accuracy of the published parts of the cited literature sources is in line with the approved norms and rules of the journal. We declare that for the drafting and revision of the paper, we have strictly respected the rules of acceptance, and in terms of references and citations of the literature used in our scientific research, ethical and academic norms have been taken into account and respected.
Institution & Department: The data in which our study is reported were collected in “Albanian Eye Center”, Tirana, Albania, managed by Associated Prof. Ali TONUZI, in cooperation with the University Hospital Center, “Mother Theresa”, Tirana (UHCT), for all the data of the control group.
Acknowledgments: The authors of the manuscript have great gratitude to the staff of private/public institutions and hospitals in Albania, as well as especially gratitude to Mr. Luan Qafmolla for the obligation and adjustment of our manuscript according to the guidelines of the journal, as manager of this project and research article Also, thanks and gratitude to Prof. Dr. Ruzhdie Qafmolla who professionally supported this reported study.
Consent on information: Written consent was obtained on the disclosure and use of personal data, and illustration photos in the scientific article for all patient, who became a participant in this study report and agreed to publish the data and measurements performed.
Conflict of interest: No conflict of interest has been declared by the three authors.
Financial disclosure: The authors declare, this study case received no financial support because it was a unique case for the data collected and reported.
Corresponding person: Luan Qafmolla, managing of the project for this research article.
References
- Burns JA (1978) “Atlas of Eye Surgery and Related Anatomy”. 7: 234237.
- Dutton JJ, et al. (1994) “The lacrimal systems. Atlas of Clinical and Surgical Orbital Anatomy”. Philadelphia. W.B Saunders 140–142.
- Vikas Sinhala (1998) Shah Medical Collage Jamnagar Hospital, Gujarat, India “Dacryocystorhynostomia endoscopic”. 2: 12-14, 21-32.
- Weber AL, Rodriguez-De Velasquez A, Lucarelli MJ, Cheng HM (1996) “Normal anatomy and lesions of the lacrimal sac and duct: evaluated by dacryocystography, computed tomography, and MR imaging”. Neuroimaging Clin N Am 6: 199-217
- Malik SR, Gupta AK, Chaterjee S, et al. (1969) “Dacryocystography of normal and pathological passages”. British Journal Ophtalmolology 53: 174-179.
- Wormald PJ (1984) “Powered Endonasal dacryocystorhinostomy Laryngoscope”; “Digital subtraction macroda-cryocystography. A new method of lachrymal system imaging. Ophthalmology” 91: 956-962.
- Ashenhurst M, Jaffer N, Hurwitz J, et al. (1991) “Combined computed tomography and dacryorhynography for complex lacrimal system imaging”. Can J Ophthalmol 26: 27-31.
- Freitag SK, Woog JJ, Kousoubris PD, et al. (2002) “Helical computed tomographic dacryocystography with three-dimensional reconstruction”. A new view of lacrimal drainage system”. Ophthalmology Plastic Reconstruction Surgery 18: 121-132.
- Rice DH, et al. (1998) “Endoscopic dacryocystorhinostomy: A cadaver study”. American Journal of Rhinology 2: 127-128.
- Kanski Jack J. “A Systematic Approach”. King Edward VII Hospital, Windsornson. United Kingdom, Clinical Ophthalmology Journal 44-53.
- Aron Andrea (1957) “Një metodë e modifikuar nga ana jonë për dakriocistorinostominë eksterne”. A study of the University Hospital Center “Mother Theresa”, Tirana. 11-23; 26-32.
- Hartikainen J, Antila J, Varpula M (1998) “Prospective randomized comparison of endonasal endoscopic dacryocystorhinostomy”. Laryngoscope 108: 1861-1864.
- G,B, Hanafee W, N. (1968) “Distension dacryocystography”; Radiology 90: 1020-1022.
- George Spaeth, Helen Danesh-Meyer, Ivan Goldberg, Anselm Kampik (2013) “Ophthalmic Surgery: Principles and Practice” 1: 13-17; 35-38.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.