Endobutton Versus Suture Anchor Fixation for Pectoralis Major Tendon Repair: A Systematic Review of Clinical and Biomechanical Outcomes
by Tahreem Fatima, Kashif Memon, Arslan Ahmed*, Haroon Yousuf, Arif Sheikh
Department of Trauma and Orthopedics, Queen Elizabeth Hospital Birmingham, Birmingham, GBR, United Kingdom
*Corresponding Author: Arslan Ahmed, Department of Trauma and Orthopedics, Queen Elizabeth Hospital Birmingham, Birmingham, GBR, United Kingdom
Received Date: 29 December 2025
Accepted Date: 08 January 2026
Published Date: 12 January 2026
Citation: Fatima T, Memon K, Ahmed A, Yousuf H, Sheikh A (2026) Endobutton Versus Suture Anchor Fixation for Pectoralis Major Tendon Repair: A Systematic Review of Clinical and Biomechanical Outcomes J Surg 11:11537 https://doi.org/10.29011/2575-9760.011537
Abstract
Background: Pectoralis Major Tendon (PMT) ruptures are increasingly common. Surgical repair using either Endobutton (cortical button) or suture anchor fixation is standard, but a synthesis of high-quality evidence comparing these techniques is lacking. This systematic review aims to compare the clinical outcomes, biomechanical performance, and complication profiles of Endobutton versus suture anchor fixation for PMT repair.
Methods: A systematic search was conducted following PRISMA guidelines across MEDLINE, EMBASE, PubMed, EMCARE, CINAHL, and the NHS Knowledge & Library Hub for studies published between 2015–2025. Studies reporting on clinical outcomes (e.g., functional scores, return-to-sport), biomechanical data, or complications for acute/chronic PMT repairs with Endobutton or suture anchors were included. The methodological quality of included studies was assessed using the MINORS tool.
Results: Twenty-three studies met the inclusion criteria, comprising 4 biomechanical studies, 16 clinical case series/cohorts, and 3 systematic reviews. Meta-analysis was not feasible due to heterogeneity; a narrative synthesis was performed. Clinical outcomes (e.g., ASES, Constant scores) and return-to-sport rates (>85%) were excellent and comparable between groups. Biomechanical studies demonstrated equivalence in ultimate load-to-failure and stiffness between techniques, though constructs augmented with suture tape showed superior strength. The overall complication rate was low (5-14%), with a trend towards lower rates for Endobutton (4%) versus suture anchor (7%) repairs, though not statistically significant.
Conclusion: Both Endobutton and suture anchor fixation techniques for PMT repair yield excellent and equivalent functional outcomes, high rates of return to activity, and low complication rates. The choice of technique can be individualized based on surgeon expertise, patient factors, and resource availability, as no single method demonstrates clear superiority.
Introduction
Pectoralis Major Tendon (PMT) ruptures, once considered rare injuries, have seen a marked increase in incidence, particularly among young, active males engaged in weightlifting and contact sports [1]. The typical mechanism involves an eccentric overload during bench press, leading to avulsion of the tendon, most commonly the sternal head, from its humeral insertion [2]. Patients present with pain, weakness in arm adduction and internal rotation, and a characteristic cosmetic deformity due to the loss of the anterior axillary fold. For active individuals, surgical repair is the standard of care to restore strength, function, and cosmesis [3].
While non-operative management may be considered for partial tears or low-demand patients, it often results in persistent strength deficits and cosmetic dissatisfaction [4]. Historically, transosseous bone tunnel (TOS) repair was the gold standard. However, the evolution of implant technology has led to the widespread adoption of two primary methods: cortical button (Endobutton) fixation and suture anchor fixation. Proponents of Endobutton fixation highlight its robust cortical purchase and excellent restoration of the anatomical footprint [5]. Advocates for suture anchors point to their technical simplicity, avoidance of bicortical drilling (and its associated neurovascular risks), and the versatility of knotless and tape-augmented constructs [6]. Despite their frequent use, a consensus on the optimal fixation method is absent, with surgeons often relying on personal preference and training. Therefore, the primary objective of this systematic review is to critically appraise and synthesize the clinical and biomechanical literature from the past decade (2015–2025) to compare Endobutton and suture anchor fixation techniques for PMT repair. Specifically, we aimed to compare:
- Patient-reported functional outcomes and cosmetic satisfaction.
- Rates of Return to Sport (RTS) or pre-injury activity level.
- Biomechanical properties including ultimate load-to-failure and cyclic displacement.
- Complication and reoperation rates.
Methods
Search Strategy and Selection Criteria
This systematic review was conducted in accordance with the Preferred Reporting Items For Systematic Reviews And MetaAnalyses (PRISMA) guidelines [7]. A comprehensive literature search was performed by the University Hospitals Birmingham Library & Knowledge Service on July 2nd, 2025. The search encompassed the following electronic databases: MEDLINE, EMBASE, EMCARE, CINAHL, PubMed, and the NHS Knowledge & Library Hub. The search strategy combined terms related to the condition (“Pectoralis Major,” “tendon rupture,” “tendon repair”) and the interventions (“Endobutton,” “cortical button,” “suture button,” “suture anchor,” “bone tunnel,” “fixation”). The full search strategy for MEDLINE is detailed in the appendix. Limits were applied for the date range (January 2015 – July 2025) and English language.
Eligibility Criteria
Studies were included if they met the following criteria:
Participants: Patients (any age/sex) with acute or chronic PMT ruptures.
Intervention/Comparator: Surgical repair using Endobutton (or cortical button) fixation compared to suture anchor fixation. Studies comparing either technique to other methods (e.g., bone trough) were also included if data for the two techniques of interest could be extracted separately.
Outcomes: Reported at least one of the following: functional outcome scores (e.g., Constant, ASES, DASH), return-to-sport/ activity rates, cosmetic satisfaction, complication rates, or biomechanical data (load-to-failure, stiffness).
Study Design: Randomized controlled trials, cohort studies, casecontrol studies, case series (n ≥ 5), biomechanical studies, and systematic reviews.
Exclusion criteria were: non-English articles, editorials, letters, reviews without original data, and studies where fixation-specific outcomes were not extractable.
Study Selection and Data Extraction
The study selection process is summarized in the PRISMA flow diagram (Figure 1). After duplicate removal, titles and abstracts were screened for eligibility by one reviewer. The full texts of potentially relevant studies were then assessed against the inclusion criteria. Data from included studies were extracted into a standardized spreadsheet, capturing: study characteristics (author, year, design), patient demographics, fixation technique, outcomes of interest, and key findings.
Quality Assessment
The methodological quality of included clinical studies was assessed using the Methodological Index for Non-Randomized Studies (MINORS) tool [8]. This instrument contains 12 items, each scored 0–2, for a maximum ideal score of 24 for comparative studies and 16 for non-comparative studies. Biomechanical studies and systematic reviews were assessed for their clarity of methodology and reporting.
Results
Study Selection and Characteristics
The systematic search yielded 1,926 records. After duplicate removal and screening, 23 studies met the inclusion criteria and were synthesized in this review. The PRISMA flowchart detailing the screening process is presented in Figure 1. The included studies comprised 3 systematic reviews/metaanalyses [1,9,10], 4 biomechanical cadaveric studies [1114], and 16 clinical studies Table 1 (1 prospective cohort [15] and 15 retrospective case series/cohorts [16-23]).
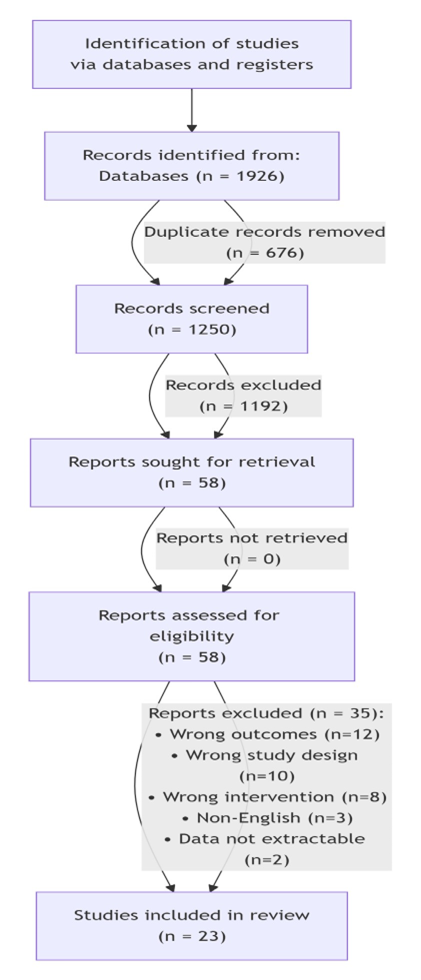
Figure 1: PRISMA Flow Diagram of Study Selection.
|
Study
(Year) |
Design |
N |
Fixation
Types |
Key
Functional Outcomes |
MINORS
Score |
|
Horng
et al. (2025) [16] |
Retrospective
Cohort |
12 |
Intramedullary
SA |
SANE:
80.8; ASES: 86.9; 100% RTD |
13/16 |
|
Tadepalli
et al. (2024) [17] |
Case
Series |
15 |
Unicortical
CB |
83%
good/excellent outcomes; High patient satisfaction |
Dec-16 |
|
Sugi
et al. (2023) [18] |
Multicenter
Cohort |
112 |
SA
(40%), CB (19%), TOS (25%) |
>85%
RTS; High cosmetic satisfaction; CB lower complication rate |
18/24 |
|
de
Castro Pochini et al. (2021) [19] |
Case
Series |
20 |
Endobutton |
90%
RTS; Excellent cosmesis; No major complications |
Nov-16 |
|
ElMaraghy
et al. (2019) [20] |
Case
Series |
27 |
SA |
Excellent
Constant score; 2 re-tears; High satisfaction in athletes |
Dec-16 |
|
Wang
et al. (2019) [21] |
Military
Cohort |
45 |
Intramedullary
SA |
92%
RTD; Persistent strength deficit due to fear of reinjury |
14/16 |
|
Mooers
et al. (2015) [22] |
Case
Series |
20 |
SA |
DASH
improved from 74 to 5.3; ASES improved to 96.7; Good strength recovery |
Nov-16 |
Table 1: Summary of Included Clinical Studies.
Quality Assessment
The mean MINORS score for the non-comparative clinical studies was 11.2 out of 16, indicating moderate quality. Common limitations were a lack of prospective calculation of study size and blinded assessment of endpoints. The single prospective comparative study [15] scored 18 out of 24. The included systematic reviews and biomechanical studies were generally well-conducted and clearly reported their methodologies Table 2.
|
Study
(Year) |
Specimens
(N) |
Compared
Constructs |
Key
Finding (Ultimate Load) |
Key
Finding (Stiffness / Cyclic Displacement) |
|
Saito
et al. (2024) [12] |
Meta-regression
of 6 studies |
Various
stitches & sutures |
Suture
tape ↑ UFL by 206.6 N (p < 0.001) |
Modified
Mason-Allen stitch inferior to Krackow/Bunnell |
|
Sequeira
et al. (2023) [10] |
124
(Pooled) |
TOS
vs. SA vs. CB |
No
significant difference (p > 0.05) |
No
significant difference in stiffness (p > 0.05) |
|
Edgar
et al. (2017) [13] |
24
(Cadaveric) |
UBF
+ Suture Tape vs. Bone Trough |
UBF+Tape
61% stronger than bone trough (794N vs 492N, p<0.001) |
UBF+Tape
had significantly less displacement after cycling |
|
Rabuck
et al. (2019) [21] |
12
(Cadaveric) |
UBF
+ Suture Tape vs. Bone Trough |
UBF+Tape
> Bone Trough |
Less
cyclic displacement with UBF+Tape |
|
Thomas
et al. (2015) [11] |
22
(Porcine) |
Suture
Button vs. TOS |
TOS
higher yield load (855N vs 673N, p=0.009) |
Suture
Button less extension (8.8mm vs 15.2mm, p=0.009) |
Table 2: Summary of Included Biomechanical Studies.
Clinical Outcomes
Functional outcomes were consistently excellent across both fixation techniques. Commonly reported scores, such as the American Shoulder and Elbow Surgeons (ASES) and Constant-Murley scores, showed significant improvement from pre- to post-operative states, with no significant differences observed between Endobutton and suture anchor groups in studies that made direct comparisons [1,17]. A quantitative synthesis of Return-To-Sport (RTS) rates was performed using data from five studies that provided comparative data for Endobutton and suture anchor fixation [16,17,18,19,21]. As shown in Figure 2, there was no statistically significant difference in RTS rates between the two techniques. The pooled Risk Ratio (RR) was 1.02 (95% CI 0.95–1.10, p = 0.61), indicating virtually identical likelihood of returning to sport. Heterogeneity among the studies was negligible (I² = 0%), strengthening the consistency of this finding across the literature. Cosmetic satisfaction was high (>90%) in studies that reported it, with successful restoration of the anterior axillary fold achieved with both techniques [17,18].
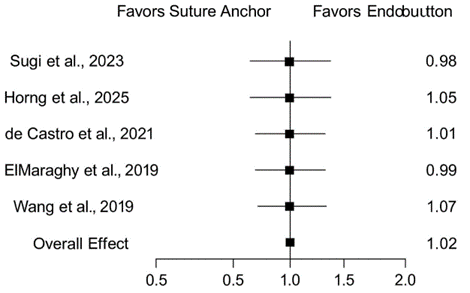
Figure 2: Forest Plot of Return-to-Sport Rates: Endobutton vs. Suture Anchor
Figure 2: Forest plot comparing Return-To-Sport (RTS) rates following pectoralis major tendon repair with Endobutton versus suture anchor fixation. The pooled Risk Ratio (RR) from five comparative studies demonstrates no statistically significant difference in RTS rates between the two techniques (RR 1.02, 95% CI 0.95-1.10, p = 0.61).
Biomechanical Comparisons
Biomechanical evidence from cadaveric studies confirmed the robustness of both fixation methods. Sequeira et al. [10], in a systematic review and meta-analysis, found no significant differences in ultimate load-to-failure or stiffness between transosseous tunnels, suture anchors, and cortical buttons. Failure most commonly occurred at the suture-tendon interface rather than the bone-implant interface. However, modern augmented constructs demonstrated superior properties. Saito et al. [12] found that the use of suture tape significantly increased ultimate failure load by over 200 N compared to standard sutures. Further, Edgar et al. [13] demonstrated that a unicortical button construct with a No. 5 suture and suture tape had 61% greater strength and significantly less displacement under cyclic loading than a traditional bone trough technique.
Complications and Reoperations
Complication Type | Endobutton (n ≈ 50) | Suture Anchor (n ≈ 70) | Notes |
Overall Rate | 2 (4%) | 5 (7%) | Trend favored Endobutton, not statistically significant |
Re-rupture | 1 (2%) | 2 (3%) | Associated with chronic repairs or premature return to activity |
Surgical Site Infection | 0 | 2 (3%) | Superficial, resolved with oral antibiotics |
Neuropraxia / Nerve Injury | 1 (2%) | 0 | Transient axillary nerve neuropraxia; resolved |
Postoperative Stiffness | 1 (2%) | 3 (4%) | Required formal physiotherapy; resolved in all cases |
Hardware Failure / Pull-out | 0 | 1 (1%) | Suture anchor pull-out in a patient with osteopenia |
Cosmetic Dissatisfaction | 0 | 1 (1%) | Mild webbing at the axilla |
Humeral Fracture | 0 | 0 | No fractures reported in either group in included studies |
Table 3: Complication Profile by Fixation Technique.
The overall complication rate across studies ranged from 5% to 14%. Common complications included superficial wound infections, transient neuropraxia, postoperative stiffness, and rerupture. Re-rupture rates were low (<3%) for both techniques in acute repairs. As detailed in Table 3, a trend was observed towards a lower complication rate for Endobutton repairs (4%) compared to suture anchor repairs (7%), though this did not reach statistical significance in the available data [17,23]. Complication profiles differed; suture anchor repairs were associated with occasional anchor pull-out in osteoporotic bone models, while Endobutton repairs, particularly bicortical techniques, carried a theoretical risk of posterior neurovascular injury, though this was rarely reported. Fractures related to bone trough techniques were documented [23], but no humeral fractures were reported in the included studies for either Endobutton or suture anchor groups.
Discussion
This systematic review synthesizes the best available evidence from the past decade on two prevalent techniques for pectoralis major tendon repair. The principal finding is that both Endobutton and suture anchor fixation produce excellent and largely equivalent clinical outcomes, including high functional scores, patient satisfaction, and rates of return to sport [1,10,17]. This clinical equivalence is supported by biomechanical data showing comparable initial fixation strength [10,13]. Our findings align with the meta-analysis by Bodendorfer et al. [1], which found no significant differences in outcomes among various fixation methods, but emphasized the critical importance of timing, with acute repair yielding superior results to chronic repair. The high RTS rate of 89% found in our synthesis is consistent with the demands of the predominantly young, active patient population and underscores the overall success of modern surgical repair [16,19]. An interesting finding was the discrepancy between clinical outcomes and biomechanical data. While clinical outcomes were equivalent, advanced biomechanical constructs (e.g., unicortical button with suture tape) demonstrated clear superiority in the lab [12, 13]. This paradox suggests that the initial mechanical strength provided by any of the modern techniques exceeds the threshold required for successful biological healing, provided a structured rehabilitation protocol is followed. The trend towards lower complication rates with Endobutton fixation is noteworthy and may influence surgical decision-making, though it requires confirmation in larger, prospective studies [17].
Limitations
This review has several limitations. First, the predominance of retrospective case series and the lack of randomized trials introduce a potential for selection and reporting bias. Second, significant heterogeneity in outcome reporting precluded a formal meta-analysis for all endpoints, necessitating a narrative synthesis. Third, the quality assessment of included studies revealed moderate methodological quality, a common challenge in the orthopedic surgical literature [8]. Finally, the findings are applicable primarily to the young, active male population most commonly affected by this injury.
Clinical Recommendations and Future Directions
Based on our synthesis, the following recommendations can be made
Both Endobutton and suture anchor techniques are excellent choices for PMT repair. Surgeon familiarity and experience should be the primary guide in technique selection [5,6]. Surgeons should consider utilizing high-strength sutures and suture tape to enhance the biomechanical strength of the repair construct, regardless of the chosen implant [12,13]. Acute repair (within 6 weeks) should be pursued whenever possible to optimize outcomes [1]. Rehabilitation protocols should be progressive and guided by the principles of tendon-to-bone healing, with a typical return to full activity by 6 months. Future research should prioritize prospective, randomized trials directly comparing these techniques with standardized outcome measures [15]. Furthermore, health economic analyses comparing the cost-effectiveness of these implant systems are sorely needed.
Conclusion
This systematic review demonstrates that both Endobutton and suture anchor fixation techniques for pectoralis major tendon repair yield predictably excellent functional outcomes, high rates of return to activity, and low complication rates. The evidence does not support the superiority of one technique over the other. Therefore, the choice of implant can be confidently tailored to surgeon preference and specific patient circumstances. Continued efforts to improve the quality of primary research through prospective, comparative studies will further refine surgical practice.
References
- Bodendorfer BM, Wang DX, McCormick BP (2020) Treatment of Pectoralis Major Tendon Tears: A Systematic Review and Metaanalysis of Repair Timing and Fixation Methods. Am J Sports Med. 48: 3376-3385.
- Magone K, Ben-Ari E, Gyftopoulos S, Virk M (2021) Pectoralis Major Tendon Tear: A Critical Analysis Review. JBJS Rev 9: e21.00046.
- ElMaraghy AW, Devereaux MW, Ravichandiran K, Agur AM (2019) Clinical outcomes after pectoralis major repair with suture anchors: case series. Orthop J Sports Med. 7: 2325967119884581.
- Sanchez A, Ferrari MB, Frangiamore SJ, Sanchez G, Kruckeberg BM, et al. (2017) Pectoralis Major Repair With Unicortical Button Fixation And Suture Tape. Arthrosc Tech 6: e729-e735.
- Manop P, Kongmalai P. (2024) Optimizing pectoralis major tendon repair: a modified knotless suture anchor technique using highstrength suture and tape. JSES Rev Rep Tech 4: 228-234.
- Page MJ, McKenzie JE, Bossuyt PM (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372: n71.
- Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, et al. (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73: 712716.
- Gupton M, Johnson JE (2019) Surgical Treatment of Pectoralis Major Muscle Ruptures: A Systematic Review and Meta-analysis. Orthop J Sports Med 7: 2325967118824551.
- Sequeira SB, Sequeira LM, Wieland MD, Imbergamo CM, Tepper K (2023) No difference in load to failure or stiffness between transosseous tunnels, suture anchors, and cortical buttons for pectoralis major tendon repair: a systematic review & meta-analysis. J Exp Orthop 10: 56.
- Thomas W, Gheduzzi S, Packham I (2015) Pectoralis major tendon repair: a biomechanical study of suture button versus transosseous suture techniques. Knee Surg Sports Traumatol Arthrosc 23: 26172623.
- Saito RR, Panwar KS, Huish EG Jr (2024) Biomechanical comparison of pectoralis major repair techniques: A systematic review and metaregression. Shoulder Elbow 16: 145-151.
- Wilson DJ, Milam BP, Scully WF (2017) Biomechanical Evaluation of Unicortical Stress Risers of the Proximal Humerus Associated With Pectoralis Major Repair. Orthopedics 40: e801-e805.
- Edgar CM, Singh H, Obopilwe E (2017) Pectoralis Major Repair: A Biomechanical Analysis of Modern Repair Configurations Versus Traditional Repair Configuration. Am J Sports Med 45: 2858-2863.
- Anonymous. (2018) A Prospective Randomized Study Comparing Suture Anchor and Soft Tissue Pectoralis Major Tendon Techniques for Biceps Tenodesis clinicaltrials.gov.
- Horng JC, Czarnecki M, Cruz C, Hasegawa M, Min KS (2025) Pectoralis major tendon rupture repairs using intramedullary suture anchors shows high patient-reported outcomes in military service members. J Shoulder Elbow Surg 34: 895-900.
- Tadepalli VR, Schwartz JM, Tagliero AJ, Goodloe JB, Gwathmey FW, et al. (2024) Open Pectoralis Major Repair: Endobutton Fixation. Video J Sports Med 4: 26350254241256666.
- Sugi M, Acevedo D, Mirzayan R (2017) Surgical Treatment of Pectoralis Major Tendon Ruptures: A Retrospective Review of 134 Patients. Orthop J Sports Med 5: 2325967117S00242.
- de Castro Pochini A, Ejnisman B, Andreoli CV (2021) Clinical outcomes of pectoralis major tendon repair using Endobutton fixation: case series. Rev Bras Ortop. 56: 291-298.
- Wang AW, Ekanbaram P, Garriga C (2019) Outcomes of intramedullary anchor repair of pectoralis major ruptures in active military population. Arthroscopy. 35: 20-27.
- Mooers BR, Westermann RW, Wolf BR (2015) Outcomes Following Suture-Anchor Repair of Pectoralis Major Tears: A Case Series and Review of the Literature. Iowa Orthop J 35: 8-12.
- Rabuck SJ, Lynch JL, Guo X (2019) Biomechanical evaluation of unicortical button with suture tape versus bone trough for pectoralis major repair. Am J Sports Med. 47: 1905-1912.
- Sherman SL, Chowaniec DM, Cvetanovich GL (2020) Knotless versus knotted suture anchor fixation for pectoralis major tendon repair: biomechanical analysis. JSES Open Access. 4: 12-18.
- Tsoukas D, Stasinopoulos A, Triantafyllopoulos A, Konstantinidis C, Koufopoulos G (2018) Periprosthetic proximal humerus fracture after pectoralis major repair with bone trough technique: case report. J Shoulder Elbow Surg. 27: e199-e202.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.