Efficacy of Anti-Hypertensive Monotherapy in Primary Open-Angle Glaucoma (POAG) Patients at the Centre of Application of the Diploma of Specialized Studies in Ophtalmology at Donka National Hospital of Conakry
by Thierno Madjou BAH*, Fadima Tamim Hann, Alpha Ibrahima Baldé, Abdoul Karim Baldé
University of Gamal Abdel Nasser of Conakry, Guinea
*Corresponding author: Thierno Madjou BAH, University of Gamal Abdel Nasser of Conakry, Guinea.
Received Date: 12 August 2025
Accepted Date: 18 September 2025
Published Date: 22 September 2025
Citation: BAH TM, Hann FT, Baldé AI, Baldé AK (2025) Efficacy of Anti-Hypertensive Monotherapy in Primary Open-Angle Glaucoma (POAG) Patients at the Centre of Application of the Diploma of Specialized Studies in Ophtalmology at Donka National Hospital of Conakry. Ophthalmol Res Rep 9: 171. https://doi.org/10.29011/2689-7407.100171
Abstract
Purpose: The aim of this study was to determine the efficacy of different antihypertensive therapeutic classes in monotherapy for the treatment of primary open-angle glaucoma at the Centre d’Application du Diplôme d’Etudes Spécialisées en Ophtalmologie de Donka. Methods: The study was observational-analytical, including patients with naive eyes at baseline. An eye was considered naive when it had never received a drop of antihypertensive medication. The study variables were socio-epidemiological (age, sex), intraocular pressure, therapeutic classes and molecules used. Intraocular pressure (IOP) was measured with a Goldmann applanation tonometer and was not correlated with central corneal thickness. The percentage of pressure reduction was calculated for each therapeutic class. Statistical analysis was performed using Epi info v7.2.2.16 and SPSS v21. Pearson correlation was applied for a p-value of less than 5% considered significant. Results: The mean age of patients was 46.9 ± 22.3 years, with extremes of 12 and 89 years; the sex ratio was 1. The therapeutic classes were beta-blockers (53.7%), prostaglandin analogues (43.9%) and carbonic anhydrase inhibitors (2.4%). Prostaglandin analogues proved superior in efficacy, but very close to betablockers (Pearson coefficient = 0.79).Conclusion: prostaglandin analogues and bet-blockers are the best classes for the initial treatment of open-angle glaucoma as monotherapy.
Keywords: Efficacy; Anti-hypertensive; monotherapy; POAG treatment; CADES/O.
Introduction
Open-angle glaucoma, whether primary or secondary, is the most common cause of irreversible blindness worldwide, and second only to cataracts [1]. The prevalence of primary open-angle glaucoma (POAG) varies according to ethnic origin. In their study of the epidemiology of glaucoma in sub-Saharan Africans in 2023, Kyari F et al. [2] reported that GPAO was more frequent in subjects of African and Afro-Caribbean origin (4.2%), intermediate in Caucasians and Hispanics (2.1%), and less frequent in Asian subjects (1.4%). In 2022, TM Bah et al. [3] found a hospital prevalence of POAG of 3.1% in Conakry. Blindness due to POAG can be prevented or at least delayed if the diagnosis is made early and treatment instituted. Currently available treatment options for glaucoma include eye drops, laser treatment or surgery. Eyedrops, with their easy access and proven efficacy in lowering IOP, represent the first-line treatment for glaucoma in Africa [3]. Betablockers, prostaglandin analogues, carbonic anhydrase inhibitors, alpha-2 adrenergic agonists and parasympathomimetic myotics are the main therapeutic classes available, with greater access for the first three classes in Guinea. In monotherapy, meta-analyses have demonstrated the superior efficacy of prostaglandin analogues over other therapeutic classes in reducing blood pressure [4,5]. These studies have particularly analyzed Western or Asian studies, which raises the question of their applicability to melanoderm subjects. It is therefore necessary to initiate such studies to understand the case of the black subject and in particular the Guinean. The aim of this study was to determine the efficacy of different antihypertensive therapeutic classes in monotherapy for the treatment of primary open-angle glaucoma at the Centre of Application of the Diploma of Specialized studies in Ophtalmology at Donka National Hospital of Conakry.
Patients and Methods Patients
These were patients diagnosed with open-angle glaucoma treated with anti-hypertensive monotherapy and followed up at the center for application of the diploma of specialized studies in ophthalmology. The study only included patients with naive eyes at baseline. An eye was considered naive when it had never received a drop of anti-hypertensive medication. Patients already treated with a combination of anti-hypertensive agents, patients treated by laser or surgery, and patients who had not enrolled in the study were excluded. Recruitment was exhaustive, and the size of the study population was based on the number of patients responding to the inclusion criteria. The study followed strict adherence to the World Medical Association’s Declaration of Helsinki on studies involving human subjects [6].
Methods
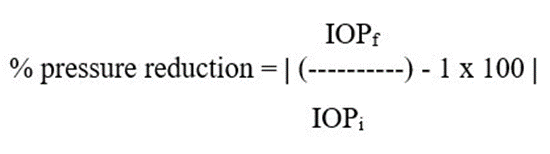
This was an observational, analytical study lasting six (6) months from January 2025 to June 2025. The diagnosis of glaucoma was made on the basis of a complete ophthalmological examination (visual acuity, slit lamp, gonioscopy, fundus) performed for each patient by a senior ophthalmologist. Gonioscopy was performed using a Goldmann three-mirror lens, looking for an open iridocorneal angle. The angle was considered open when there was no possibility of closure (grade 3 or grade 4) according to Shaffer’s classification [7]. The study variables were socio-epidemiological (age, gender), intraocular pressure, therapeutic classes and molecules used. Intraocular pressure (IOP) was measured with a Goldmann applanation tonometer after instillation of one drop of proparacaine 5% and one drop of fluorescein in blue light. It was measured at patient inclusion and at each follow-up appointment, without being correlated with central corneal thickness [8]. In this series, the values at inclusion (initial IOP, IOPi) and at the last follow-up appointment (final IOP, IOPf) were considered. The mean IOP for each therapeutic class was calculated as the sum of IOPs per patient divided by the total number of patients in each therapeutic class. The percentage pressure reduction was calculated for each therapeutic class using the absolute value formula:
The therapeutic classes were prostaglandin analogues, betablockers, carbonic anhydrase inhibitors and the molecules Latanoprost, Travoprost, Timolol, Cartéolol and Dorzolamide. Data were collected manually and analyzed using SPSS version 21. Pearson correlation was applied for a p-value of less than 5% considered significant.
Results
The study included 82 out of 148 patients with primary open-angle glaucoma. Patients ranged in age from 12 to 89 years, with a mean age of 46.9 ± 22.3 years and a median age of 46 years. There were as many men as women, with a sex ratio of 1 (Table 1).
|
n |
% |
|
|
Age (year) |
||
|
<20 |
8 |
9.8 |
|
20-39 |
25 |
30.5 |
|
40-59 |
23 |
28 |
|
60-79 |
18 |
21.9 |
|
≥ 80 |
8 |
9.8 |
|
Sex |
||
|
Homme |
41 |
50 |
|
Femme |
41 |
50 |
Table 1: Age and sex of patients (n = 82).
According to therapy, 53.7% (n = 44) were on beta-blockers, 43.9% (n = 36) on prostaglandins and 2.4% (n = 2) on carbonic anhydrase inhibitors. Mean initial IOP at inclusion was 25.0 ± 8.0 mmHg, with extremes of 10 and 50 mmHg. The percentage of patients was proportional to IOP values. In contrast, for final IOP, mean IOP was 16.5 ± 3.7 mmHg, with extremes of 10 and 27 mmHg. The percentage of patients was inversely proportional to IOP values (Figure 1).
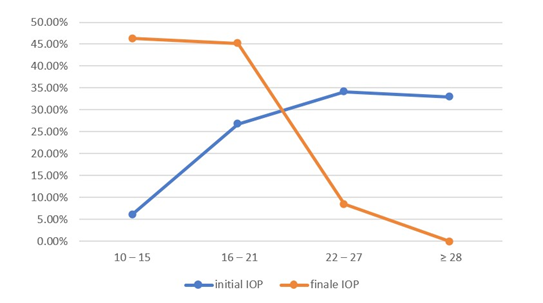
Figure 1: Intraocular pressure in millimeters of mercury (mmHg) (n = 82).
Patients were treated with different molecules, including Timolol 0.5% prescribed for 48.9% (n = 40), and Latanoprost 0.05% for 37.8% (n = 31). Figure 2 shows the number of patients with or without a reduction in IOP according to the molecule used.
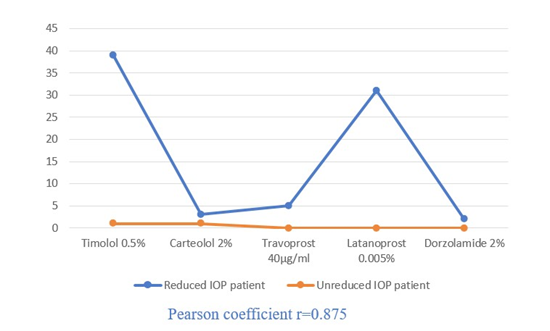
Figure 2: IOP reduction and resistance curves by molecule.
The resistance curve was flat for Latanoprost, Travoprost and Dorzolamide, in contrast to Timolol and Cartéolol, where one patient resisted each of these molecules. Nevertheless, Timolol and Latanoprost each achieved an IOP reduction of almost 35%, ahead of Cartéolol (27%) and Travoprost (25%) (Table 2).
|
Mean IOPi |
Mean IOPf |
% Reduction IOP |
|
|
Beta-blocker |
|||
|
Timolol |
24.2 |
15.8 |
34.5 |
|
Carteolol |
21 |
15.4 |
26.7 |
|
Prostaglandin Analog |
|||
|
Latanoprost |
27.1 |
17.5 |
35.4 |
|
Travoprost |
22.6 |
17 |
24.8 |
|
CAI* |
|||
|
Dorzolamid |
22 |
16.8 |
23.6 |
Table 2: Percentage of reduction in IOP by molecule; (*): Carbonic anhydrase inhibitor.
Overall, analysis of the linear trend curve showed that prostaglandin analogues had the best percentage reduction in IOP compared with the other therapeutic classes (Figure 3).
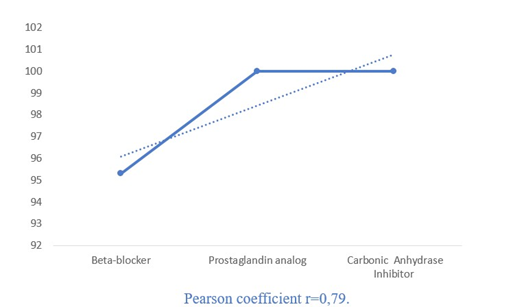
Figure 3: Percentage of reduction in IOP by therapeutic class.
Discussion
To the best of our knowledge, this monocentric observational study, which analyzed the efficacy of anti-hypertensive medical therapy as monotherapy for the treatment of primary open-angle glaucoma, is the first of its kind to be initiated in Guinea. Despite the many difficulties and limitations encountered, it provides a real insight into the efficacy and suitability of anti-glaucoma therapy for the Guinean population. These difficulties and limitations included the exclusion of a significant number of patients who dropped out of the study, and the absence of a visual field device and OCT for monitoring disease progression at the time of the study. Above all, the diagnosis had been clinical, and IOP measurements during follow-up yielded the results we discuss in this chapter, which, in our view, cannot suffer from any scientific impediment. The age of the patients was that found in the literature [2,3], but younger subjects were present in this series. The gender disparity found in studies, probably due to selection bias, always resulting in a tendency for one sex to predominate over the other, was not found in this series. POAG is therefore a pathology of both men and women. Primary open-angle glaucoma is a chronic, progressive eye disease with potential and irreversible blindness, causing visual field loss through damage to the optic nerve and the Retinal Nerve Fibre Layer (RNFL) with a normal-looking iridocorneal angle. The main risk factors are IOP level and age [8]. Reducing IOP is currently the only therapeutic approach that has been shown to be effective in reducing the risk of conversion of ocular hypertonia to glaucoma or slowing the progression of established glaucoma [9]. The aim of treatment is therefore to preserve the patient’s quality of life, and it is therefore essential to lower IOP as much as possible in order to avoid visual field deterioration [9]. Initiation of treatment most often begins with monotherapy, and the number of molecules is increased as a function of therapeutic failure in order to achieve the desired target IOP [10]. A single drug is usually prescribed from one of four therapeutic classes: beta-blockers, carbonic anhydrase inhibitors, alpha-2 adrenergic agonists and prostaglandin analogues [4]. The greater prescription of beta-blockers compared with prostaglandin analogues in this study is probably linked to their greater accessibility in terms of price in pharmacies, as the population is very poor. The inversion of the inclusion IOP curve at the end of the study can only be attributed to the overall efficacy of the therapeutic classes used (Figure 1). This could explain the flattening of the resistance curve, although there was relative resistance to betablockers (Figure 2). Vass C et al. [10] explained in 2007, without taking into account possible resistance to treatment, that treatment of ocular hypertension with any drug is more effective than placebo or no treatment in reducing IOP and the appearance of visual field defects. But taken individually, no drug showed significant protection of the visual field, although there was positive but weak evidence of a beneficial effect of beta-blockers. This hypothesis could have been verified if the study had included visual field or OCT analysis. Indeed, IOP reduction correlates with visual field preservation, but definitive or more significant outcomes such as visual field change and optic nerve damage are not easy to quantify and effects on patient-centred outcomes such as visual function and blindness require a long follow-up period to be observed [11,12]. This was not the case in this study. In several studies [4,9-12], as in this series, prostaglandin analogues have shown superior efficacy among monotherapy regimens in terms of pressure reduction (Figure 3), although differences within classes were generally very small (Latanoprost vs Timolol, Carteolol vs Travoprost) (Table 2). However, in clinical practice, Li F et al. [5] stated that when considering IOP lowering regimens, it is important to consider not only the efficacy of IOP lowering, but also the incidence of adverse events. Prostaglandins have been associated with adverse ocular side effects (ocular surface irritation, eyelash lengthening, iris colour change) that some patients may find bothersome [13]. However, they are well tolerated systemically, unlike betablockers, which have a bradycardia inducing effect. Beta-blockers are, however, very well tolerated in the eye [10]. Latanoprost has a lower risk of conjunctival hyperaemia than the other prostaglandin analogues [4]. By class, the mean reduction in IOP was greater with latanoprost, then timolol and finally dorzolamide. However, the series by Bron A [14] showed that the reduction in IOP at night was more marked with dorzolamide than with timolol. There is therefore reason to believe that CAIs provide better control of night-time IOP than beta-blockers because their mode of action does not depend on factors extrinsic to the active substance, as is the case with beta-blockers. A drop of beta-blocker in the morning is therefore physiologically the most effective, as it can prevent the effect of adrenergic hormones when they are secreted at their peak. This allows timolol to reduce aqueous humour production during the day, but has no effect at night [14]. As for prostaglandins, the increase in aqueous humour drainage is via the uveoscleral route, which frees us from the episcleral venous pressure that can hinder trabecular drainage. It is easy to understand why, when lying down at night (which increases episcleral venous pressure), prostaglandins continue to act unhindered on aqueous humour drainage [14].
Conclusion
The study enabled us to weigh up the reduction in IOP as monotherapy between the different classes in the treatment of POAG. Prostaglandin analogues and beta-blockers were all highly effective, with relative superiority for the former. In one aspect of the decision-making framework, prostaglandin analogues and beta-blockers are the best classes for the initial treatment of openangle glaucoma as monotherapy. The choice will therefore lie with the practitioner to initiate treatment with one or other therapeutic class, taking into account the patient’s purchasing power and the time of action of each therapeutic class.
Acknowledgements
The authors would like to thank Dr Amde-Michael KETEMA for his institutional and unconditional support for research in Guinea. The authors also thank Professor Jeannette TRAORE for the quality of the corrections made to this work.
Conflicts of interest
The authors declare that they have no conflicts of interest in relation to this study.
References
- Renard JP, Sellem E, Bour T, Lalanne MC (2014) Le GPAO Problème de santé publique. In : Rénard JP, Sellem E, dir. Rapport de la Société Française dOphtalmologie. Paris : Elsevier Masson 13-21.
- Kyari F, Abdull MM, Bastawrous A, Gilbert CE, Faal H (2013) Epidemiology of Glaucoma in Sub-Saharan Africa: Prevalence, Incidence and Risk Factors. Middle East Afr J Ophthalmol 20: 111-125. 3. Bah TM, Rama R, Sovogui MD, Diane S, Lama PL, et al. (2002) Aspects épidémiologiques, cliniques et thérapeutiques du glaucome à ouvert au Centre d’Application du Diplôme d’Etudes Spécialisées en Ophtalmologie (CADES/0), Hôpital National Donka. JACCR 6: 78-85. 4. Li T, Lindsley K, Rouse B, Hong H Shi Q, Friedman DS et al. (2016) Comparative effectiveness of first-line medications for primary openangle glaucoma: a systematic review and network meta-analysis. Ophthalmology 123: 129-140.
- Li F, Huang W, Zhang X (2018) Efficacy and safety of different regimens for primary open-angle glaucoma or ocular hypertension: a systematic review and network meta-analysis. Acta Ophthalmologica 96: e277-e284.
- World Medical Association. Declaration of Helsinki. Ethical Principles for medical research involving human subjects ; 2001 [on line]. [Updated 3rd April 2025 ; Consulted 07thAugust 2025]. 7. Shaffer RN (1963) Stereoscopic Manual of Gonioscopy. J Medic Education 38: 529.
- European Glaucoma Society. Terminology and Guidelines for glaucoma. 5th Edition. Savona : Publicomm ; 2021.
- Aptel F, Labbé A, Baudouin C, Brond A, Lachkare Y, et al. (2014) Glaucoma medications, preservatives and the ocular surface. JF Ophtalmol 37: 728-736.
- Bertaud S, Aragno V, Baudouin C, Labbé A (2019) Primary open-angle glaucoma. Rev Med Interne 40: 445-452.
- Weinreb RN, Brandt JD, Garway-Heath D, Medeiros FA (2007) World Glaucoma Association. Intraocular Pressure. Consensus Series 4. Amsterdam, The Netherlands : Kugler Publications.
- Weinreb RN, Kaufman PL (2011) Glaucoma research community and FDA look to the future, II : NEI/FDA Glaucoma Clinical Trial Design and Endpoints Symposium : measures of structural change and visual function. Invest Ophthalmol Vis Sci 52: 7842-7851.
- Boland MV, Ervin AM, Friedman DS, Jampel HD, Hawkins BS, et al. (2013) Comparative effectiveness of treatment for open-angle glaucoma : a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 158: 271-279.
- Topper JE, Brubaker RF (1985) Effects of timolol, epinephrine, and acetazolamide on aqueous flow during sleep. Invest Ophthalmol Vis Sci 26: 1315-1319.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.