Effectiveness and Safety of the TVT Exact Mid-Urethral Tape for Stress Urinary Incontinence in Low-Volume Centers: A Long-Term Follow-Up
by Michal Borowik1*, Dorota Joanna Borowik2, Marek Roslan1
1Department of Urology, Faculty of Medicine, University of Warmia and Mazury, Olsztyn, Poland
2Department of Physiotherapy, Faculty of Health Sciences, VISTULA University in Olsztyn, Poland
*Corresponding Author: Michal Borowik, Department of Urology, Faculty of Medicine, University of Warmia and Mazury, ul. Oczapowskiego 2, 10-719 Olsztyn, Poland
Received Date: 19 August 2025
Accepted Date: 22 August 2025
Published Date: 26 August 2025
Citation: Borowik M, Joanna DB, Marek Roslan M (2025) Effectiveness and Safety of the TVT Exact Mid-Urethral Tape for Stress Urinary Incontinence in Low-Volume Centers: A Long-Term Follow-Up. Ann Case Report. 10: 2385. https://doi.org/10.29011/2574-7754.102385
Abstract
Introduction: Mid-urethral sling surgery is the standard treatment for stress urinary incontinence (SUI), but outcomes from lowvolume centers are underreported. We evaluated the efficacy and safety of the Gynecare TVT-Exact mid-urethral sling in women with SUI treated at three low-volume urological centers. Methods: Between October 2012 and August 2020, 58 women (mean age 60.6, range 41–83 years) with SUI underwent TVT-Exact placement at three centers (19, 31, and 9 cases respectively). Preoperative evaluation included SUI type (I–III) and grade (majority grade III), a 24-hour pad test, and the ICIQ-UI SF questionnaire. All patients received a standardized retropubic TVT-Exact polypropylene sling (Gynecare, Ethicon Inc.). Outcomes included operative time, hospital stay, blood loss, objective cure (completely dry), overall improvement, and complications. Results: Mean preoperative 24-hour pad loss was 87 mL (range 8–870). At a mean follow-up of 47.8 months (range 12–103), the objective cure rate was 81%, and overall cure or improvement was 94.8%. Mean operative time was 26 minutes (22–35) and mean hospitalization was 12.1 hours (5–96). Blood loss was minimal; only two cases (at one center) exceeded 200 mL, with one transfusion required. Complications were infrequent: one bladder perforation, one late bladder tape erosion, one vaginal tape erosion, one urinary retention, one hemorrhage requiring reoperation, and four urinary tract infections (managed conservatively). Conclusion: In low-volume centers, TVT-Exact sling surgery achieved high cure rates and low complication rates comparable to high-volume institutions. The procedure is safe and effective in low-volume settings when performed by experienced surgeons with standardized kits.
Keywords: Stress Urinary Incontinence; Treatment; Suburethral Sling; Urinary Retention; Low Volume Centers.
Abbreviations: SUI - stress urinary incontinence; MUS - mid-urethral sling; TVT - tension-free vaginal tape; ICIQ-UI - International Consultation on Incontinence Questionnaire-Urinary Incontinence, OAB - overactive bladder; SD - standard deviation; IQR - interquartile range; BMI - body mass index; UTI - urinary tract infection.
Introduction
Stress urinary incontinence (SUI) is a common condition in women, defined by involuntary urine leakage during exertion or activities such as exercise, coughing or sneezing [1]. Epidemiological studies estimate a prevalence of approximately 15–35% among adult women [2, 3]. According to the integral theory of female urinary incontinence, the pathophysiology frequently involves urethral hypermobility and/or intrinsic sphincter deficiency due to pelvic floor laxity [4]. Although SUI is not life-threatening, it can markedly impair quality of life and is associated with social withdrawal, sexual dysfunction, depression and anxiety, particularly in more severe cases [5-7].
Conservative measures lifestyle modification, weight loss, pelvic floor muscle training (PFMT) and bladder training are recommended as first-line therapy. When these fail to provide adequate relief, surgical treatment is considered the gold standard [8-10]. Despite the burden of disease, only a small proportion of women undergo surgery (≈5%), and even fewer seek specialist care, suggesting under-treatment [11]. Over the past century numerous surgical approaches have been developed, but a major advance occurred in the mid-1990s with the introduction of the tension-free vaginal tape (TVT) by Ulmsten and Petros [12]. The retropubic mid-urethral sling (MUS) uses a polypropylene tape placed beneath the mid-urethra to provide support during rises in intra-abdominal pressure and achieved rapid global adoption because of high effectiveness and relatively low morbidity [1315]. TVT-Exact is a refinement of the original retropubic TVT, designed to facilitate tape delivery while preserving the proven mid-urethral sling concept.
Some studies have suggested that high-volume centres (>50 anti-incontinence procedures per year) achieve better outcomes, potentially reflecting surgeon experience and institutional processes [13-15]. Conversely, the standardised nature of TVT may allow comparable results in smaller hospitals provided surgeons are appropriately trained. Whether low-volume centres (performing only a few sling procedures annually) can achieve outcomes similar to those of high-volume units remains a relevant service-delivery question.
This study aimed to assess the efficacy and safety of TVT-Exact performed in low-volume centres (<20 cases per year per centre). We conducted a retrospective analysis across three regional hospitals, evaluating objective cure/improvement and peri- and postoperative complications to determine whether outcomes are maintained despite lower surgical volume.
Materials and methods
Study design and patients
We performed a retrospective, multicentre cohort study of 58 women who underwent TVT-Exact for SUI between October 2012 and August 2020 at three neighbouring regional hospitals, each performing fewer than 20 anti-incontinence operations annually. Case numbers per centre were 19, 30 and 9, respectively. All patients had predominant SUI (Stamey grade II or III). Detailed baseline demographics and clinical characteristics for the whole cohort are summarised in (Table 1), and key characteristics by centre in (Table 2). There were no significant baseline differences between centres with respect to age, body mass index (BMI), SUI severity or major comorbidities (all p > 0.05).
|
Variable |
Value |
|
Number of patients (female) |
58 |
|
Age (years), mean ± SD (range) |
60.6 ± 11.4 (41–83) |
|
Body Mass Index (kg/m²), mean ± SD (range) |
27.6 ± 3.9 (19.0–39.0) |
|
Pads used per day, mean ± SD (range) |
4.2 ± 2.0 (2–10) |
|
24-h pad test (g), mean ± SD (range) |
86.7 ± 143.0 (6–870) |
|
ICIQ-UI SF score, median (IQR) |
17 (13–21) |
|
Mean follow-up duration (months), range |
47.8 (12–103) |
|
Prior hysterectomy, n (%) |
7 (12%) |
|
Previous anti-incontinence surgery, n (%) |
9 (16%) |
|
History of urinary tract infection, n (%) |
4 (7%) |
Table 1: Baseline demographic and clinical characteristics of the study cohort (N = 58)
|
Center 1 (n = 19) |
Center 2 (n = 30) |
Center 3 (n = 9) |
|
|
Age (years), mean ± SD |
59.6 ± 13.0 |
62.2 ± 10.4 |
56.0 ± 11.2 |
|
BMI (kg/m²), mean ± SD |
26.3 ± 2.99 |
27.6 ± 3.81 |
29.6 ± 5.10 |
|
24-h pad test (g), mean ± SD |
137.6 ± 240.7 |
61.0 ± 36.7 |
64.9 ± 39.9 |
|
Pre-operative ICIQ-UI SF score, mean ± SD |
16.7 ± 2.5 |
18.4 ± 1.7 |
18.1 ± 2.3 |
|
Mean follow-up (months) [range] |
63.9 [12–103] |
47.3 [32–64] |
14.8 [12–25] |
|
Previous anti-incontinence surgery, n |
4 |
2 |
3 |
|
History of UTI, n |
1 |
3 |
0 |
Table 2: Key patient characteristics by center
Surgical technique
All procedures were performed by consultant urologists who had completed formal training and certification in anti-incontinence surgery at the same academic institution. A uniform technique was followed according to the manufacturer’s instructions for the Gynecare TVT-Exact kit (Figure 1a) Under regional or general anaesthesia, patients were placed in lithotomy. After insertion of an 18F Foley catheter to empty the bladder, a 1-cm midline incision was made in the anterior vaginal wall approximately 1 cm from the external urethral meatus. Bilateral para-urethral dissection was carried out to the mid-urethra. The TVT-Exact tape, mounted on plastic introducer trocars, was advanced via the vaginal incision in a retropubic trajectory and externalised through two small (~4 mm) suprapubic skin incisions ~4 cm apart. The bladder was refilled (~150 mL saline) and inspected by rigid cystoscopy (19F, 70° lens) to exclude injury. Once the absence of perforation was confirmed, trocars were brought out through the suprapubic incisions, pulling the polypropylene mesh into position beneath the mid-urethra. The tape was adjusted to lie tension-free (without compressing the urethra), plastic sheaths were removed and excess mesh trimmed at the skin exit sites. The bladder was emptied and urethral mobility assessed using a female metal catheter. The vaginal incision was closed with absorbable sutures and a vaginal pack placed for haemostasis (removed after a few hours). In uncomplicated cases no indwelling catheter was left postoperatively.

Figure 1a: TVT Extract Operation Set
Perioperative care
All patients received antibiotic prophylaxis (cephalosporin or trimethoprim) perioperatively. A fast-track protocol was used: patients were mobilised within hours of anaesthesia and discharged the same day or the following morning provided they voided spontaneously. Duration of hospitalisation, anaesthetic type and perioperative events were recorded. Follow-up and outcome measures
Institutional review board approvals were obtained at all centres, and all patients provided informed consent. Data were collected from hospital charts and outpatient records and supplemented by standardised interviews (telephone or in-person). Preoperative variables included SUI type/grade (Stamey classification), 24-hour pad test (grams), and patient-reported symptom severity using the International Consultation on Incontinence Questionnaire–Urinary Incontinence Short Form (ICIQ-UI SF) [16].
Postoperative follow-up visits were scheduled at approximately 1, 3 and 12 months, and annually thereafter when feasible. Outcomes were assessed at the last available follow-up. Objective cure (dryness) was defined as no leakage on stress manoeuvres and no pad use. Improvement was defined as ≥50% reduction in leakage episodes and pad use. Patients also completed the ICIQ-UI SF at final follow-up. Complications and subsequent interventions were recorded. All 58 women had at least one documented postoperative assessment (≥6 months); 51/58 (87.9%) had evaluable follow-up of ≥12 months. Among those with ≥12 months’ follow-up, the mean duration was 47.8 months (range 12–103).
Statistical analysis
Analyses were performed in Statistica 13 PL (StatSoft, Poland). Normality was assessed by Shapiro–Wilk and homogeneity of variance by Levene’s test. For between-centre comparisons, one-way analysis of variance (ANOVA) was used for approximately normally distributed variables; otherwise the Kruskal–Wallis test was applied. Where overall differences existed, appropriate post-hoc multiple comparisons were undertaken. Categorical variables were compared using the chi-square or Fisher’s exact test. Results are presented as mean ± standard deviation (SD) or median (interquartile range, IQR). Two-tailed α = 0.05 was used; p < 0.05 was considered statistically significant.
Statistical distributions are illustrated with box-and-whisker plots; all relevant statistical diagrams are available from the corresponding author upon reasonable request.
Statistical analysis of the materials is illustrated with box-andwhisker plots (Figure 1b-5).
It showed no significant difference in the mean age of patients across the study centres (p = 0.340). Post-hoc multiple-comparison testing likewise detected no pair-wise age differences between individual centres (p > 0.05). (Figure 1b)
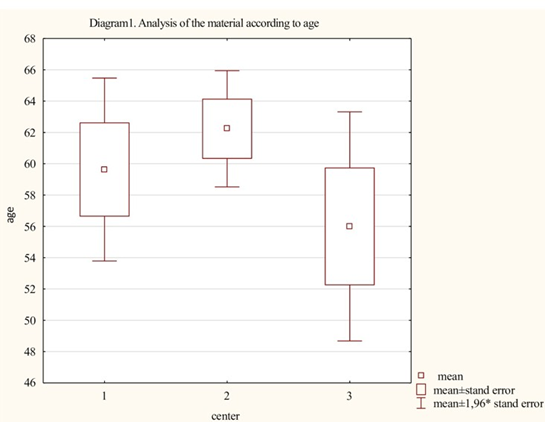
Figure 1b: Age
Statistical analysis found no significant differences in patients’ mean BMI across the study centres (p = 0.094). Post-hoc multiple-comparison testing likewise identified no pair-wise BMI differences between individual centres (p > 0.05) (Figure 2)
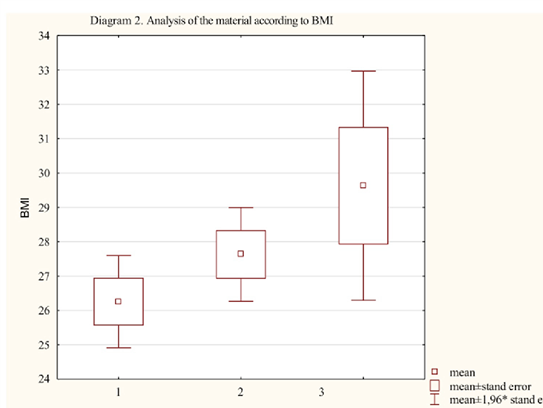
Figure 2: BMI
Statistical analysis revealed no significant differences in the mean PAD values among patients across the study centres (p = 0.259). Post-hoc multiple-comparison testing likewise detected no pairwise differences in PAD between individual centres (p > 0.05) (Figure 3)
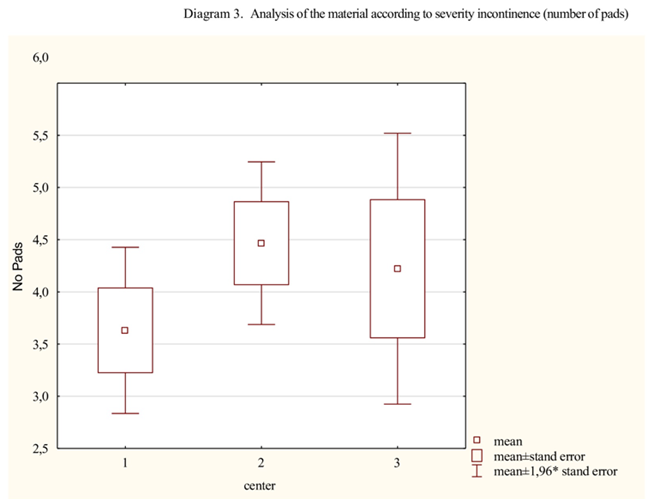
Figure 3: Pads
Statistical analysis showed no significant difference in the mean 24-hour pad-test results among patients across the participating centres (p = 0.871). Post-hoc multiple-comparison analysis likewise revealed no pairwise differences in 24-hour pad-test outcomes between individual centres (p > 0.05) (Figure 4).
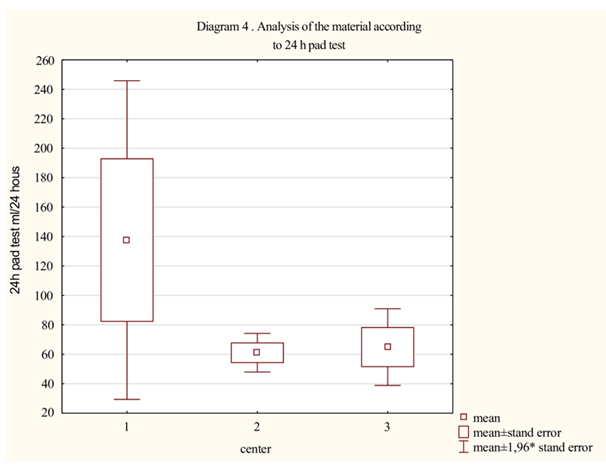
Figure 4: 24h pad test
Statistical analysis revealed no significant differences in preoperative mean ICIQ-SF questionnaire scores among the participating centres (p = 0.059). Post-hoc multiple-comparison testing likewise showed no pair-wise differences in pre-operative ICIQ-SF scores between individual centres (p > 0.05) (Figure 5)
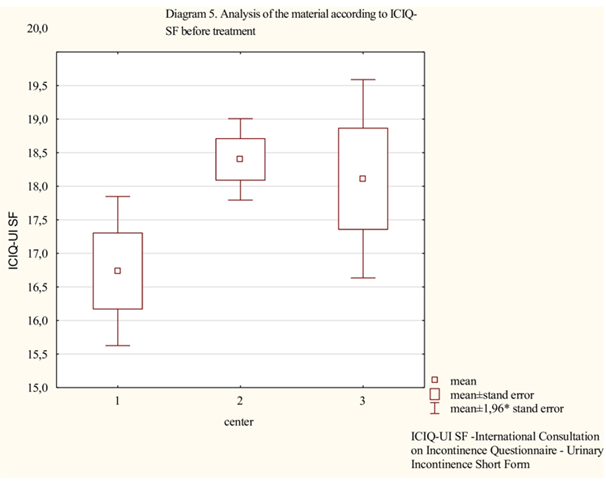
Figure 5: iciqsf pre
Results
Statistical Analysis
Statistical analysis showed a significant difference in mean operative time across the study centres (p < 0.001). Post-hoc multiple-comparison testing confirmed significant pair-wise differences between Centre 1 and Centre 2 (p < 0.001) and between Centre 2 and Centre 3 (p = 0.024), whereas no significant difference was observed between Centre 1 and Centre 3 (p > 0.05) (Figure 6).
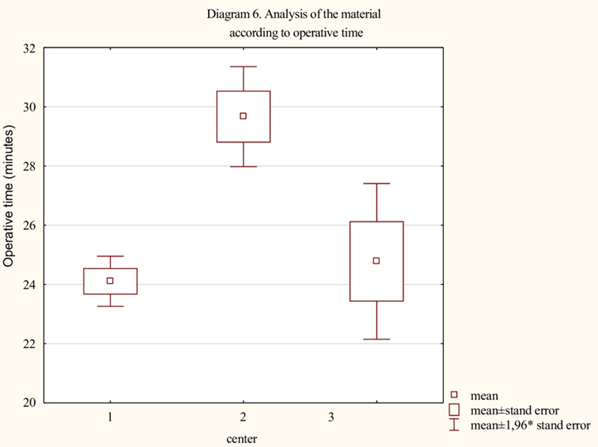
Figure 6: Operative time
Statistical analysis demonstrated a significant difference in mean postoperative length of stay (hours) among the study centers (p < 0.001). Post-hoc multiple-comparison testing identified a significant pair-wise difference only between Centre 1 and Centre 2 (p < 0.001); no other inter-center differences reached statistical significance (p > 0.05) (Figure 7).
Figure 7: Operative time
Statistical analysis revealed a significant difference in the mean ICIQ-SF questionnaire scores across the study centres (p = 0.024). Post-hoc multiple-comparison testing demonstrated a significant pair-wise difference only between Centre 2 and Centre 3 (p = 0.022); no other inter-centre differences reached statistical significance (p > 0.05) (Figure 8).
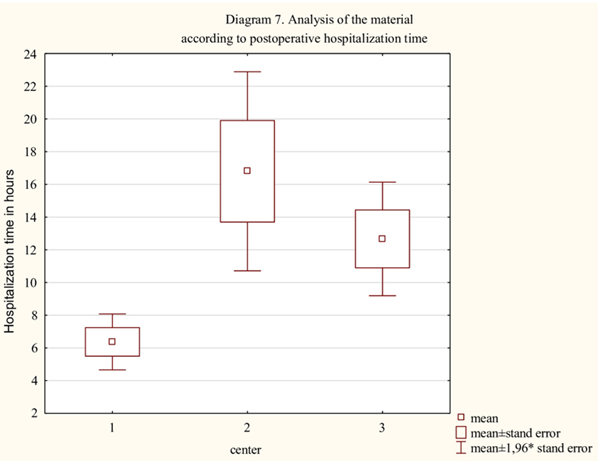
Figure 8: iciqsf after
Operative outcomes and complications
All 58 procedures were completed without major intraoperative complications. Mean operative time was 26.2 ± 2.5 min (range 22–35). Blood loss was minimal in most cases; estimated blood loss was typically <50 mL, and no patient had intraoperative haemorrhage >500 mL. Two patients (3.4%) experienced bleeding >200 mL; one required postoperative transfusion and one underwent haematoma evacuation. There were no bowel or major vascular injuries. Bladder perforation occurred in 2/58 (3.4%); both were recognised intraoperatively on cystoscopy, the trocars were repositioned and a Foley catheter was left for three days. Neither patient experienced sequelae. No urethral injuries were recorded.
Early postoperative complications were infrequent: four patients (6.9%) developed lower urinary tract infections within one month, all treated successfully with oral antibiotics. One patient (1.7%) had acute urinary retention managed with a one-week indwelling catheter; normal voiding resumed thereafter. Transient voiding hesitancy in the immediate postoperative period occurred in ~15% but resolved spontaneously and was not counted as a complication.
During longer-term follow-up, two patients (3.4%) developed mesh-related erosions. One had a 1-cm segment of tape exposed in the vaginal wall at six months and underwent outpatient excision with local tissue coverage. The second presented two years postoperatively with recurrent urinary tract infections; imaging demonstrated an intravesical calculus and cystoscopy revealed tape erosion into the bladder. A transvesical laparoendoscopic single-site (T-LESS) procedure was used to remove the eroded mesh with good recovery and no recurrence. No cases of chronic pelvic pain or dyspareunia attributable to the mesh were reported.
Efficacy
At last available follow-up (mean among those with ≥12 months 47.8 months), 47/58 (81.0%) were objectively dry. A further 8/58 (13.8%) reported marked improvement (reduced leakage and pad use but not completely dry). Overall success (cure + improvement) was 94.8%; 3/58 (5.2%) were classified as failures. The median postoperative ICIQ-UI SF score for the cohort was 4 (IQR 0–7), a substantial reduction from the preoperative median of 17, indicating a large improvement in patient-reported symptom severity. Among patients with ≥12 months’ follow-up, 8/51 (15.5%) reported de novo urgency/overactive bladder symptoms, all mild and managed conservatively (lifestyle measures ± anticholinergic or β3-agonist therapy).
Hospital stay and recovery
Postoperative recovery was rapid. Mean duration of hospitalisation was 12.7 ± 13.3 hours (range 4–96); 59% were managed as true day-case procedures (<24 h), with nearly all others discharged by the next morning (Table 3). All 19 patients (100%) in the smallest centre were treated on an outpatient basis (<24 h), compared with 40% in the largest centre. Discharge policies reflected institutional practice and patient preference; importantly, the shorter stays in Centre 1 were not associated with higher complication or readmission rates. All patients were required to void spontaneously before discharge.
Crucially, objective cure rates, overall success and complication rates did not differ significantly between centres (all p > 0.1), indicating comparable clinical performance despite volume differences.
All key perioperative and outcome measures for each center are summarized in (Table 3).
Center 1(n = 19) | Center 2<(n = 30) | Center 3(n = 9) | Total (N = 58) | |
Objective efficacy (at last follow-up) | ||||
• Cure (dry), n (%) | 15 (78.9%) | 24 (80.0%) | 8 (88.9%) | 47 (81.0%) |
• Improved, n (%) | 3 (15.8%) | 4 (13.3%) | 1 (11.1%) | 8 (13.8%) |
• Failure, n (%) | 1 (5.3%) | 2 (6.7%) | 0 (0%) | 3 (5.2%) |
Operating time (minutes), mean ± SD | 24.0 ± 1.8 | 29.7 ± 4.7 | 24.8 ± 4.0 | 26.2 ± 2.5 |
Postoperative hospital stay (hours), mean [range] | 6 [5–10] | 16.8 [4–96] | 13.5 [5–18] | 12.1 [4–96] |
One-day procedures, n (%) | 19 (100%) | 12 (40.0%) | 3 (33.3%) | 34 (58.6%) |
Type of anesthesia: spinal/epidural, n (%) | 5 (26.3%) | 9 (30.0%) | 1 (11.1%) | 15 (25.9%) |
Type of anesthesia: general, n (%) | 14 (73.7%) | 21 (70.0%) | 8 (88.9%) | 43 (74.1%) |
ICIQ-UI SF score at final follow-up, mean ± SD | 4.1 ± 3.7 | 5.5 ± 4.8 | 2.6 ± 3.1 | 4.1 ± 4.0 |
Clavien–Dindo grade > II complications, n (%) | 2 (10.5%) | 1 (3.3%) | 1 (11.1%) | 4 (6.9%) |
Blood loss > 200 mL, n | 1 (5.3%) | 0 | 1 (11.1%) | 2 (3.4%) |
Bladder perforation, n | 0 | 2 (6.7%) | 0 | 2 (3.4%) |
Bladder erosion (intravesical), n | 0 | 1 (3.3%) | 0 | 1 (1.7%) |
Vaginal tape erosion, n | 1 (5.3%) | 0 | 0 | 1 (1.7%) |
Re-operation for bleeding, n | 1 (5.3%) | 1 (3.3%) | 0 | 2 (3.4%) |
Bowel injury, n | 0 | 0 | 0 | 0 |
Follow-up duration (months), mean [range] | 63.9 [12–103] | 47.3 [32–64] | 14.8 [12–25] | 47.8 [12–103] |
Table 3: Operative outcomes and complications by center
Discussion
To our knowledge, this is the first study evaluating the outcomes of TVT-Exact mid-urethral sling procedures performed in lowvolume centers. We found that even with fewer than 20 cases per year at each hospital, the standardized technique and thorough training of surgeons yielded outcomes on par with those reported from high-volume institutions. All three participating urology departments followed uniform surgical and perioperative protocols, and importantly, all procedures were performed by experienced urologists who had been formally trained and certified in the TVT technique. As a result, we observed no significant differences in success rates or major complications between the three centers aside from a shorter average hospitalization in one center, which reflected a difference in postoperative management strategy rather than surgical quality.
Our findings indicate that low surgical volume does not necessarily adversely affect treatment efficacy or safety, provided the surgical team is well-trained and adheres to best practices. This observation is echoed by other authors. For example, in a nationwide analysis of 1,455 TVT procedures in Finland, Kuuva and Nilsson reported similar complication rates in local community hospitals as in academic referral centers [15]. This suggests that a surgeon’s experience and adherence to standardized protocols may be more important determinants of outcome than the sheer number of surgeries performed at a facility. In our series, despite the smaller scale of operations at each center, the cure rates and safety profile were comparable to those from high-volume reference centers published in the literature.
Efficacy in Context: The therapeutic efficacy of the TVT-Exact procedure in our cohort was very high and consistent with global data. At a mean follow-up of about 4 years, the objective cure rate (complete dryness) was 81%, and including those with significant improvement it reached 94.8%. These outcomes align with previously reported values. For example, Porena et al. (in a multicenter randomized trial) observed a 71–77% objective cure rate at ~2.5 years for retropubic vs transobturator slings, which rose to ~90% when improved cases were included [17]. Aniulienė et al. reported a 94–95% cure rate at 12 months specifically for TVT-Exact, in line with our short-term results [13]. Numerous other studies also document cure rates exceeding 80–90% at 1–2 years post-surgery [19].
The durability of the TVT outcomes has been confirmed in long-term follow-ups. Broś-Konopielko et al. found that 85% of women had a negative cough stress test ~12 years after a TVT procedure, with 72.5% still satisfied with their results [14] Nilsson et al. reported that after 17 years, over 90% of patients remained objectively continent, and 87% considered themselves cured or significantly improved [18]. Our follow-up (mean ~4 years) lies between typical short-term studies (6–24 months) and those rare long-term reports (≥10 years), which may explain why our observed cure rate (~81%) is slightly lower than 1-year rates (~90%) but remains within the expected range when accounting for some recurrence of symptoms over time. It is known that SUI outcomes can decline in the long run (e.g., objective cure rates of 72–85% at 10–12 years vs ~90% at 1 year), owing to factors like aging, tissue changes, or onset of new pelvic floor issues. In our study, the 5% failure rate is consistent with the literature (reported failure rates ~2–20% in various series), which largely reflect differences in patient selection and outcome definitions across studies [15, 18 -20]. Notably, our cohort included a high proportion of severe SUI cases (most were grade III, many with intrinsic sphincter deficiency as indicated by low Valsalva leak point pressures). Such patients inherently have a higher risk of incomplete cure, which could influence success rates. This trend was also observed by Abdelwahab and Sherif, who reported that all their TVT failures occurred in women with the most severe SUI and VLPP < 60 cm H₂O [19]. Adjusting for the complexity of our patient population, our success rates are very much in line with those of high-volume centers managing similar cases.
Safety Profile and Complications: The retropubic TVT approach is known for minimal invasiveness and a low overall complication rate, a fact reaffirmed by our results and numerous published studies. In our entire series, there were no life-threatening complications and no injuries to major organs (bowel, major blood vessels, etc.). We observed zero cases of intra-abdominal (peritoneal) tape placement, bowel injury, or severe vascular injury, complications which have been reported in under 1% of cases in large Finnish registry by Kuuva and Nilsson [15]. The most common intraoperative complication of the retropubic sling procedure bladder perforation occurred in 2 patients (3.4%). This incidence is within the typical range (approximately 1–10% reported in the literature) and both cases were recognized during surgery via cystoscopy [18-21]. They were immediately managed by repositioning the tape and leaving a catheter in place for a few days. Neither of these patients suffered any lasting harm, and this management approach is standard and has been widely reported as effective in preventing long-term issues from bladder perforation.
Excessive bleeding was rare. Only one patient (1.7%) required a blood transfusion due to perioperative hemorrhage, and two patients (3.4%) had an estimated blood loss > 200 mL. These figures align well with published data; for example, Kuuva and Nilsson noted significant hemorrhage (> 200 mL) in about 1.9% of cases, and Teo et al. reported major bleeding in 1.6% [15,20]. Our findings are on par with those results, suggesting that hemorrhagic complications of TVT are infrequent and can be effectively managed when they do occur.
The most frequent complication in our cohort was urinary tract infection. Four patients (6.9%) developed a postoperative UTI, nearly identical to the 6.6% rate reported by Abdelwahab et al. in a study comparing retropubic and transobturator tapes [19]. Systematic reviews of mid-urethral slings indicate UTI rates on the order of 7–13% [21], placing our result roughly in the middle of this range. All UTIs in our patients were managed conservatively with antibiotics and resolved without further issues, indicating that routine postoperative monitoring and early treatment of UTIs is appropriate in these patients.
We paid special attention to late complications, particularly those related to the implanted mesh tape. Two patients (3.4%) experienced tape erosions: one vaginal exposure and one tape migration into the bladder with calculus formation. This incidence is low and comparable to other reported series for retropubic slings (generally 2-6%) [21]. Importantly, both complications were successfully addressed with minimally invasive methods. The intravesical tape was removed via a single-port transvesical endoscopic surgery, as described by Ingber et al. and by Przudzik et al., avoiding the need for a large open surgery [22,23]. Neither patient had recurrence of the erosion during subsequent followup. Long-term studies suggest that the risk of new erosions does not continue to increase indefinitely; for instance, Nilsson et al. reported only one minor mesh extrusion over 17 years among TVT patients [18]. This confirms the good biocompatibility and stability of modern polypropylene sling materials over time.
Another important aspect of the sling procedure’s safety profile is the development of new lower urinary tract symptoms (LUTS) such as urgency or urge incontinence after surgery. In our study, 8 out of 51 followed patients (15.5%) experienced de novo overactive bladder (OAB) symptoms postoperatively (new onset urgency with or without urge incontinence that was not present before surgery). This rate is consistent with some reports. For example, in a meta-analysis by Huang et al., roughly 20% of women developed urgency symptoms after a mid-urethral sling [24]. On the other hand, some studies have reported lower incidences of post-sling OAB, around 8–10% [25]. The disparity likely stems from differences in how OAB is defined and the length of followup: some urgency symptoms appear transiently in the early postoperative period (related to initial irritation or inflammation) and then subside, while in other cases they may emerge or persist later. Our incidence of 15% falls within the broad range (0– 30%) reported in the literature for de novo urgency [15, 18]. It is noteworthy that the presence of postoperative OAB symptoms can affect patient satisfaction a woman might be objectively dry but still bothered by urgency, thus perceiving the outcome as less successful. In our cohort, all cases of urge de novo were mild and were effectively managed with conservative measures (lifestyle advice and, in some cases, anticholinergic or beta-3 agonist medications). These interventions mitigated the impact of OAB on overall patient satisfaction, and by last follow-up none of the patients with initial de novo OAB described their outcome as a failure of the surgery.
Voiding dysfunction (difficulty emptying the bladder) after TVT is another potential concern. In our series, significant voiding problems were uncommon. Only one patient (1.7%) had true urinary retention requiring prolonged catheterization, and that case resolved within a week. This rate is lower than some reports; for instance, Aniulienė et al. noted that approximately 20% of their TVT patients required temporary recatheterization post-op [13]. However, their definition was very broad, including even a single post-void residual check with a catheter. Other studies distinguish transient voiding difficulty (which often requires just one intermittent catheterization or an overnight catheter) from persistent retention that necessitates intervention (e.g. indwelling catheter for > 48 h or surgical tape loosening). In the Finnish national registry, complete urinary retention occurred in about 2.3% of cases, while transient voiding difficulty was reported in 7.6% [15]. If we apply similar criteria, our results are comparable: roughly 1–2% of patients had meaningful retention requiring intervention, whereas a handful had mild voiding hesitancy that resolved spontaneously. We attribute our low retention rate in part to our postoperative management protocol, patients were not discharged until they had successfully voided. This allowed us to detect any voiding issue early and address it (as with the one patient who stayed an extra week with a catheter). Ensuring normal voiding before discharge likely helped avoid missed cases of retention and contributed to the safety of early discharge.
Hospital Stay and Fast-Track Surgery: The length of hospital stay following mid-urethral sling surgery has shortened dramatically over the past two decades. Initially, when TVT was introduced, patients often stayed several days for monitoring [14]. In the late 1990s and early 2000s, typical hospital stays of 2–4 days were reported even for uncomplicated cases [15]. For example, in the years 2009–2011 Aniulienė et al. reported an average post-TVT hospitalization of about 3.5 [13]. With growing experience and evidence, there has been a shift toward outpatient management. Many centers now perform mid-urethral sling operations as daycase surgeries, and studies have shown that most patients can be safely discharged the next day or even the same day as surgery [12, 13, 15, 18]. Our findings strongly support this trend. The average hospitalization time in our cohort was only 12.7 ± 13.3 hours, meaning that the majority of patients went home the day of surgery or the morning after. In fact, 59% of our cases were true outpatient procedures with <24 h stay. This is a significantly shorter stay than that reported in historical series, and it reflects both medical and institutional factors. First, using primarily general anesthesia (in 74% of patients, (Table 3) facilitated quicker post-anesthesia recovery and earlier ambulation compared to spinal anesthesia, though both anesthesia types are viable for this procedure. Second, the minimally invasive nature of the operation (small incisions, minimal blood loss, low pain levels) allows rapid recovery without need for prolonged observation. Third, we implemented early mobilization, encouragement of oral intake, and prompt voiding trials, which expedited readiness for discharge. Early discharge has potential benefits such as lower risk of hospital-acquired infections, greater patient comfort at home, and reduced healthcare costs, without compromising the success of the surgery. Our experience shows that with proper protocols, fast-track outpatient management of TVT is feasible even in smaller regional centers.
Study Limitations: This study has several limitations that should be acknowledged. Firstly, the sample size (58 patients across three centers) is relatively small, which limits the statistical power and the generalizability of our findings. The retrospective design is another limitation reliance on medical records and patient recall can introduce information bias, and we were unable to control variables as tightly as in a prospective trial. Additionally, while our follow-up (mean 4 years) is longer than many reports for midurethral slings, it is still moderate; we might have missed very late failures or complications that occur beyond 5-10 years. Only an ongoing longitudinal follow-up would capture those outcomes.
Despite these limitations, our results were remarkably consistent with larger studies and meta-analyses, lending credibility to our data. The multicenter nature (even though each center’s volume was low) is a strength in that it demonstrates reproducibility of outcomes across different hospital settings.
Conclusions
When performed by trained surgeons using a standardised technique and perioperative pathway, the TVT-Exact retropubic mid-urethral sling is safe and effective in low-volume centres. Objective cure of 81% (overall success 94.8%), low rates of serious complications and rapid recovery with most patients discharged within 24 hours were observed across three regional hospitals with annual volumes <20 cases. Outcomes were comparable between centres despite differences in volume and discharge policy, suggesting that standardisation and surgeon training may mitigate any putative volume effect. Further prospective, adequately powered studies with longer follow-up will help confirm these findings and guide service configuration.
Conflict of Interest: None
Funding Declaration: The authors declare that they have no relevant or material financial interests that relate to the research described in this paper.
Authors contribution
M. Borowik: Study concept and design, data analysis and
interpretation, manuscript drafting, statistical analysis
D. J. Borowik: Data acquisition, administrative, technical, and material support
M. Roslan: Critical revision of the manuscript
Data availability: The datasets supporting the findings of this study, as well as the underlying box-and-whisker plots, are available from the corresponding author upon reasonable request.
Ethics approval and consent to participate: This retrospective study was approved by the institutional review boards of all three participating centres. All patients provided informed consent for the procedure and for the use of anonymised data for research purposes.
References
- Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, et al. (2010) An International Urogynecological Association (IUGA)/ International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 29: 4-20.
- Bedretdinova D, Fritel X, Panjo H, Ringa V, et al. (2016) Prevalence of female urinary incontinence in the general population according to different definitions and study designs. Eur Urol. 69: 256-264.
- Minassian VA, Drutz HP, Al-Badr A. (2003) Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet. 82: 327-338.
- Petros PE, Ulmsten UI. (1990) An integral theory of female urinary incontinence. Experimental and clinical considerations. Acta Obstet Gynecol Scand Suppl. 153: 7-31.
- Hunskaar S, Vinsnes A. (1991) The quality of life in women with urinary incontinence as measured by the Sickness Impact Profile. J Am Geriatr Soc. 39: 378-382.
- Saarni SI, Härkänen T, Sintonen H, Suvisaari J, Koskinen S, et al. (2006) The impact of 29 chronic conditions on health-related quality of life: a general population survey in Finland using 15D and EQ-5D. Qual Life Res. 15: 1403-1414.
- Rogers RG, Villarreal A, Kammerer-Doak D, Qualls C. (2001) Sexual function in women with and without urinary incontinence and/or pelvic organ prolapse. Int Urogynecol J. 12: 361-365.
- Subak LL, Wing R, Smith West D, Franklin F, Vittinghoff E, et al. (2009) Weight loss to treat urinary incontinence in overweight and obese women. N Engl J Med. 360: 481-490.
- Shaw C. (2001) A review of the psychological predictors of helpseeking behavior and impact on quality of life in people with urinary incontinence. J Clin Nurs. 10: 15-22.
- Dumoulin C, Cacciari L, Hay-Smith EJ. (2018) Pelvic floor muscle training versus no treatment for urinary incontinence in women. Cochrane Database Syst Rev. 10: CD005654.
- Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L, et al. (2017) Urinary incontinence in women: a review. JAMA. 318: 1592-1604.
- Ulmsten U, Petros P. (1995) Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Nephrol. 29: 75-82.
- Aniulienė R, Aniulis P, Skaudickas D. (2015) TVT-Exact and midurethral sling (SLING-IUFT) operative procedures: a randomized study. Open Med (Wars). 10: 311-317.
- Broś-Konopielko M, Chmielewski L, Jodzis A, Czajkowski K. (2017) Long-term effectiveness of tension-free vaginal tape (TVT) procedure – twelve years after surgery. Fam Med Prim Care Rev. 19: 196-200.
- Kuuva N, Nilsson CG. (2002) A nationwide analysis of complications associated with the tension-free vaginal tape (TVT) procedure. Acta Obstet Gynecol Scand. 81: 72-77.
- Karmakar D, Mostafa A, Abdel-Fattah M. (2017) A new validated score for detecting patient-reported success on postoperative ICIQ-SF: a two-stage analysis from two large RCT cohorts. Int Urogynecol J. 28: 95-100.
- Porena M, Costantini E, Frea B, Giannantoni A, Ranzoni S, et al. (2007) Tension-free vaginal tape versus transobturator tape for stress urinary incontinence: results of a multicentre randomized trial. Eur Urol. 52: 1481-1490.
- Nilsson CG, Palva K, Rezapour M, Falconer C. (2013) Seventeen years’ follow-up of the tension-free vaginal tape procedure for female stress urinary incontinence. Int Urogynecol J. 24: 1265-1271.
- Abdelwahab O, Sherif H. (2010) Tension-free vaginal tape versus transobturator tape for treatment of female stress urinary incontinence: a 2-year follow-up. UroToday Int J. 3: (Available from: UroToday International Journal website)
- Teo R, Moran P, Mayne C, Tincello D. (2011) Randomized trial of tension-free vaginal tape and tension-free vaginal tape-obturator for urodynamic stress incontinence in women. J Urol. 185: 1350-1355.
- Lin YH, Lee CK, Chang SD, Chien PC, Hsu YY, et al. (2021) Long-term complications of mid-urethral slings among women with stress urinary incontinence as a patient safety issue: protocol for systematic review and meta-analysis. Medicine (Baltimore). 100: e26257.
- Ingber MS, Stein RJ, Rackley RR, Firoozi F, Irwin BH, et al. (2009) Single-port transvesical excision of a foreign body in the bladder. Urology. 74: 1347.
- Przudzik M, Borowik M, Łesiów M, Łesiów R. (2019) Transvesical laparoendoscopic single-site surgery as a valuable option to remove eroded materials from the bladder: single-center experience and a review of the literature. Int Urol Nephrol. 51: 247-252.
- Huang ZM, Xiao H, Ji ZG, Yan WG, Zhang YS. (2018) TVT versus TOT in the treatment of female stress urinary incontinence: a systematic review and meta-analysis. Ther Clin Risk Manag. 14: 2293-2303.
- Ford AA, Rogerson L, Cody JD, Ogah J. (2017) Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 7: CD006375.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.