Effect of Superior Disc-Endplate Complex Degeneration on Clinical and Radiographic Results of Posterior Fixation in Thoracolumbar Fractures
by by Sen Liu#, Ruo-Yu Zhao#, Hong-Yang Gao, Gang Ji, Chao-Hua Zhu, Jia Chen, Feng Zhao, Guo-Bin Liu*
Department of Orthopedics, The First Hospital of Hebei Medical University, NO.89 Donggang Road, Shijiazhuang, 050031, China
#These authors contributed equally to this study. Sen Liu and Ruo-Yu Zhao contributed equally to this work.
*Corresponding author: Guo-Bin Liu, Department of Orthopedics, The First Hospital of Hebei Medical University; NO.89 Donggang Road, Shijiazhuang, 050031, China
Received Date: 17 June 2024
Accepted Date: 21 June 2024
Published Date: 24 June 2024
Citation: Liu S, Zhao RY, Gao HY, Ji G, Zhu CH, et al. (2024) Effect of Superior Disc-Endplate Complex Degeneration on Clinical and Radiographic Results of Posterior Fixation in Thoracolumbar Fractures. J Surg 9: 11064 https://doi.org/10.29011/2575-9760.11064
Abstract
Objective: The aim of this study was to investigate the impact of superior disc-endplate complex degeneration on the clinical and radiographic outcomes of posterior fixation in thoracolumbar fractures.
Methods: A retrospective analysis was conducted on patients who underwent posterior fixation for thoracolumbar vertebral fractures. Patients were divided based on the presence or absence of superior disc-endplate complex degeneration. Clinical outcomes, including pain relief, functional improvement, and complications, were assessed. Radiographic parameters, including fracture segment height loss and kyphotic deformity angle, were measured preoperatively and postoperatively.
Results: A total of 267 patients were included in the study. Compared to the non-degeneration group, the degeneration group had a significantly higher last follow-up angle of thoracolumbar and a lower anterior injury segment height. The degeneration group also had a significantly higher incidence of internal fixation-related complications. Furthermore, patients with internal fixation-related complications had significantly higher rates of anterior column defect and anterior injury segment height change at follow-up.
Conclusion: Superior disc-endplate complex degeneration leads to a greater loss of fracture segment height and increased kyphotic deformity angle which combined with anterior column defectc may be the risk factor for the increase of internal fixation related complications in thoracolumbar fractures.
Keywords: Disc degeneration; Kyphosis deformity; Screw breakage; Screw loosening; Thoracolumbar fracture
Introduction
Traumatic Thoracolumbar (T-L) vertebral fractures account for approximately 67-80% of all traumatic spinal injuries and primarily affect young patients [1]. They typically involve spinal instability, loss of vertebral height, acute or delayed neurological dysfunction, and can even result in severe bilateral lower limb functional deficits, urinary and bowel dysfunction, paraplegia, or even death [2]. Timely surgical intervention in cases of spinal instability and neurological deficits can help minimize the risk of secondary injury. It also facilitates nerve decompression, fracture fixation, and early mobilization, thereby preventing long-term complications [3]. Treatment options for thoracolumbar fractures include anterior, posterior, or combined approaches depending on the extent of the injury, type of fracture, and presence of associated neurological and visceral damage. In recent years, there has been rapid development in the treatment of thoracolumbar fractures, with posterior pedicle screw fixation and expansion being the most commonly used method for managing unstable fractures [4]. However, along with the widespread application of this technique and the satisfactory outcomes achieved, complications have also been reported, with screw loosening and subsequent kyphotic deformity being the most severe [5,6]. This not only leads to a compromised surgical experience, increased hospitalization costs, and physical and psychological distress for patients but can also cause secondary spinal cord injury with serious consequences. Previous studies have reported that intervertebral disc degeneration is an initiating factor for various degenerative spinal diseases, including cervical spondylosis and lumbar disc herniation, and is closely related to disc degeneration [7]. However, there is no literature available on the impact of disc degeneration on the clinical efficacy of internal fixation after traumatic thoracolumbar vertebral fractures, nor is there a definitive consensus on whether additional interbody fusion is required for isolated posterior lateral screw fixation. In this study, we aim to conduct a retrospective study to investigate the effects of disc degeneration on the clinical and radiographic outcomes of patients who undergo pedicle screw fixation for thoracolumbar vertebral fractures, with the ultimate goal of providing guidance for clinical treatment strategies.
Materials and Methods
Patients and Grouping
Between January 2008 and January 2022, a total of 267 patients (153 males and 114 females) diagnosed with traumatic thoracolumbar vertebral fractures and treated with posterior pedicle screw fixation were included in this study. The exclusion criteria were as follows: abnormal sensory and motor function of both lower limbs, abnormal urinary and bowel function, multiple fractures with fusion of the affected segments, history of other spinal diseases or previous spinal surgeries, and unwillingness to participate in the study. Disc degeneration was graded according to the Pfirrmann classification system [8,9] into five grades. All patients were divided into two groups: non-degeneration group and degeneration group. The non-degeneration group included patients with disc degeneration grade I or II, indicating no or mild disc degeneration, who only underwent posterior pedicle screw fixation without disc degeneration before or within one year after surgery. The degeneration group included patients with disc degeneration grade III, IV, or V, indicating obvious adjacent disc degeneration observed during preoperative or postoperative follow-up.
Relevant Factors
Relevant data were recorded for all patients, including demographic data, surgical factors, and postoperative complications. Demographic factors: age, gender, Body Mass Index (BMI), smoking status, drinking, history of heart disease, hypertension, diabetes, injury vertebral body, type of fracture, superior fixed segment. Surgical factors: operation time, blood loss, incision length, weight-bearing time. Radiology results: preoperative and postoperative thoracolumbar lordosis, vertebral wedge angle, Anterior Injury Segment Height (AISH). Postoperative complications: screw loosening, rod breakage, kyphosis deformity, deep vein thrombosis in the lower limbs, secondary nerve injury, revision surgery. Clinical outcomes were assessed using various validated scoring systems such as the Visual Analog Scale (VAS) and the Japanese Orthopaedic Association Scores (JOA).
Open Reduction and Internal Fixation Surgery
Open reduction and internal fixation surgery is the most commonly used surgical procedure for treating traumatic thoracolumbar fractures. The surgical steps are as follows: 1. Under fluoroscopic guidance, locate the fractured vertebra and determine the skin incision for the surgical segment. Make an incision through the skin and subcutaneous tissue, dissect the para-spinal muscles, and expose the injured vertebra and its posterior elements, such as spinous processes, laminae, and facet joints. 2. Use bone forceps to remove the bony part of the facet joint of the surgical segment vertebra, exposing the cancellous bone. Insert pedicle screws into the vertebral pedicles for stabilization, ensuring proper positioning of the injured vertebra and screws. 3. Remove the positioning pins and select pedicle screws with appropriate diameter and length. Insert the pedicle screws based on the positioning pins, ensuring that the screws penetrate the vertebral body at a depth exceeding 2/3 of the vertebral body on the lateral X-ray image and stay within the pedicle. 4. Select a connecting rod of appropriate length. Use a distractor to gently open the intervertebral space, correct the kyphotic deformity of the affected segment, tighten the nuts to secure the correction. Under fluoroscopic guidance, confirm the correction of the kyphotic deformity and achieve maximal distraction of the fractured vertebra. 5. Irrigate the wound, achieve hemostasis thoroughly, place a drainage tube, suture the wound, and cover it with sterile dressings. 6. Observe the healing of the wound and allow the patient to bear weight with a brace three days after surgery. Take measures to prevent and manage relevant complications.
Measurement of thoracolumbar kyphosis angle (Cobb angle)
All patients underwent a neutral lateral X-ray of the thoracolumbar spine. On the anterior-posterior X-ray images of the thoracolumbar spine, a tangent line is drawn on the superior endplate of the T10 vertebrae, and another tangent line is drawn on the inferior endplate of the L2 vertebrae. The acute angle between the extension lines of the two tangent lines is defined as the thoracolumbar kyphosis angle or Cobb angle. If the extension lines intersect on the ventral side of the spine, it is recorded as a positive value; if they intersect on the dorsal side of the spine, it is recorded as a negative value (as shown in Figure 1).
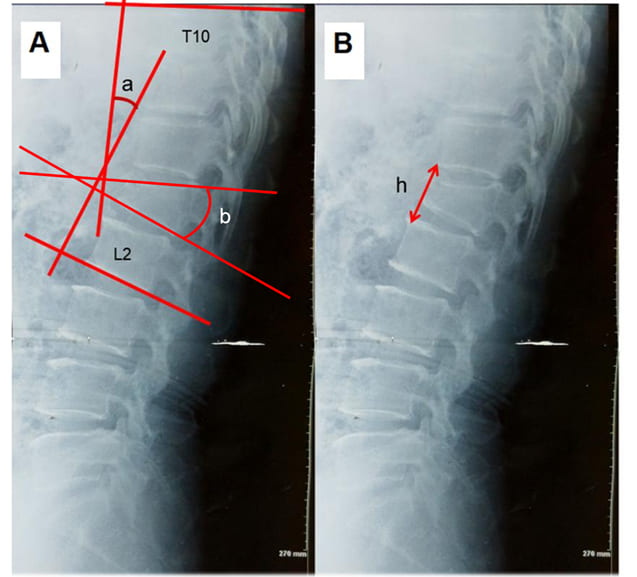
Figure 1: Measurement of thoracolumbar curvature and intervertebral height. ∠a:Thoracolumbar Cobb`s Angle. ∠b:Vertebral wedge angle. h: Anterior Column Height.
Assessment of anterior injury segment height (AISH)
All patients underwent a neutral lateral X-ray of the thoracolumbar spine. A line was drawn from the inferior anterior edge of the upper vertebrae to the superior anterior edge of the lower vertebrae at the level of the injured vertebrae. The distance between these lines was measured and recorded as the Anterior Injury Segment Height (AISH). The AISH-Index refered to the ratio of the AISH immediately after surgery to the AISH at the last follow-up. A larger AISH-Index indicated a larger anterior injury segment height change (as shown in Figure 1).
Statistical Analysis
Pairwise t-test, independent samples t-test and chi-square test were used to perform statistical analysis on the relevant influencing factors. Independent samples t-test was conducted on the metric data between the two groups; paired samples t-test was performed on pre- and post-operative metric data; chi-square test was used for analyzing count data. A significance level of P < 0.05 was defined as statistically significant. All statistical analyses were conducted using SPSS software version 13.0 (SPSS Inc, Chicago, Illinois).
Results
A total of 267 patients (129 males, 138 females) entered the final evaluation stage. According to the MRI grading of superior disc-endplate complex degeneration, there were 73 cases classified as Grade I, 105 cases as Grade II, 58 cases as Grade III, 19 cases as Grade IV, and 12 cases as Grade V. The non-degenerative group included patients with Grade I and Grade II, totaling 178 cases, while the degenerative group included patients with Grade III, Grade IV, and Grade V, totaling 89 cases. There were no significant differences in demographic factors between the two groups, including age, gender, body mass index, smoking, drinking, heart disease, hypertension, diabetes, injury vertebral body, and fracture type (Table 1).
|
No degeneration group (n=178) |
Disc degeneration group (n=89) |
P value |
||
|
Age (years) |
47.01±4.87 |
47.97±4.86 |
0.13 |
|
|
Sex ratio (M/F) |
82/96 |
47/42 |
0.299 |
|
|
BMI (kg/m2 |
24.6±2.7 |
24.1±2. |
0.108 |
|
|
Smoking (Yes/No) |
60/118 |
33/56 |
0.586 |
|
|
Drinking (Yes/No) |
45/133 |
31/58 |
0.103 |
|
|
Heart Disease (Yes/No) |
26/150 |
14/75 |
0.837 |
|
|
Hypertension (Yes/No) |
14/75 |
13/76 |
0.62 |
|
|
Diabetes (Yes/No) |
11/167 |
May-84 |
0.175 |
|
|
Injury vertebral body (T10-L2) |
0.603 |
|||
|
T10 |
15 |
5 |
||
|
T11 |
32 |
32 |
||
|
T12 |
53 |
27 |
||
|
L1 |
50 |
32 |
||
|
L2 |
28 |
10 |
||
|
Type of fracture |
0.126 |
|||
|
Burst fracture |
55 |
30 |
||
|
Compression fracture |
109 |
55 |
||
|
Others |
14 |
3 |
||
|
* P<0.05 indicates that difference has statistically significant in two groups. |
||||
Table 1: The Main Demographic Variables of Patients Before the Surgery.
Regarding surgery-related factors, including disease duration, superior fixed segment, operation time, blood loss, incision length, and postoperative weight-bearing time, there were no significant differences between the two groups (Table 2).
|
No degeneration group (n=178) |
Disc degeneration group (n=89) |
P value |
||
|
Course of disease (day) |
5.20±2.64 |
5.56±4.07 |
0.378 |
|
|
Operation time (min) |
56.5±9.7 |
56.3±9.1 |
0.873 |
|
|
Incision length (cm) |
12.5±2.9 |
12.7±2.0 |
0.311 |
|
|
Blood loss (ml) |
12.7±2.0 |
140.8±24.4 |
0.148 |
|
|
Time of weight-bearing (day) |
4.48±1.46 |
4.58±1.53 |
0.6 |
|
|
Superior fixed segment |
0.285 |
|||
|
3 |
132 |
61 |
||
|
4 |
16 |
6 |
||
|
5 |
30 |
22 |
||
|
Internal fixation complications (Yes/No) |
7/170 |
Dec-77 |
0.004* |
|
|
Screw breakage |
4 |
5 |
||
|
Screw loosening |
3 |
7 |
||
|
Lower Extremity DVT (Yes/No) |
6/172 |
Feb-87 |
0.612 |
|
|
Nerve injury (Yes/No) |
3/175 |
Feb-87 |
0.75 |
|
|
Wound infection (Yes/No) |
5/173 |
Mar-86 |
0.8 |
|
|
Fat liquefaction (Yes/No) |
8/168 |
May-84 |
0.703 |
|
|
Delayed Wound Healing (Yes/No) |
11/167 |
Sep-80 |
0.25 |
* P<0.05 indicates that difference has statistically significant in two groups.
Table 2: The Surgery-Related Variables of Patients.
Clinical Outcomes
Clinical outcome assessed using JOA scores showed no significant differences between the two groups. However, compared to the non-degenerative group, the degenerative group showed significantly poorer low back pain assessed using VAS scores at the last follow-up (Table 3).
|
No degeneration group (n=178) |
Disc degeneration Group (n=89) |
P value |
||
|
JOA score |
||||
|
Preoperative |
15.97±2.06 |
15.81±2.03 |
0.54 |
|
|
Final follow-up |
25.68±3.04 |
25.09±2.74 |
0.124 |
|
|
VAS score-low back pain |
||||
|
Preoperative |
7.05±1.03 |
6.89±1.23 |
0.256 |
|
|
Final follow-up |
1.42±0.50 |
1.80±0.40 |
<0.001* |
|
|
* P<0.05 indicates that difference has statistically significant in two groups. |
||||
Table 3: Clinical outcomes of patients between the two groups.
Radiographic Results
Compared to the non-degenerative group, the degenerative group showed significantly smaller Cobb angles at the thoracolumbar junction at the last follow-up and significantly smaller Anterior Injury Segment Height (AISH) which changed exceeding 8% at the last follow-up. Other factors showed no significant statistical differences between the two groups (Table 4).
|
No degeneration group (n=178) |
Disc degeneration Group (n=89) |
P-value |
||
|
Thoracolumbar kyphosis angle (°) |
||||
|
Preoperative |
15.64±5.04 |
14.63±5.63 |
0.132 |
|
|
Postoperative |
9.52±3.36 |
9.06 ±2.89 |
0.264 |
|
|
Final follow-up |
9.98±3.16 |
10.86±2.79 |
0.027* |
|
|
Vertebral wedge angle (°) |
||||
|
Preoperative |
8.04±2.38 |
8.14±2.29 |
0.667 |
|
|
Postoperative |
5.92±1.03 |
5.98±1.03 |
0.626 |
|
|
Final follow-up |
5.90±1.02 |
6.10±1.02 |
0.132 |
|
|
ISH-A (mm) |
||||
|
Preoperative |
1.82±0.46 |
1.76±0.57 |
0.333 |
|
|
Postoperative |
3.78±0.46 |
3.72±0.53 |
0.278 |
|
|
Final follow-up |
3.58±0.46 |
3.41±0.53 |
0.006* |
|
|
ISH-Index (%) |
5.33±0.95 |
8.45±1.69 |
<0.001* |
|
|
* P<0.05 indicates that difference has statistically significant in two groups. |
||||
Table 4: Radiographic results of patients between the two groups.
Complication
Compared to the non-degenerative group, the degenerative group exhibited significantly higher incidence of internal fixation-related complications, indicating a statistically significant difference. No significant statistical differences were observed for other complications between the two groups (Table 2). Furthermore, in the degeneration group, patients who experienced internal fixation-related complications had a significantly higher rate of vertebral body endplate defects (Figure 2) and larger AISH index exceeding 10% at the last follow-up (Table 5). There were no differences in posterior vertebral body injuries.
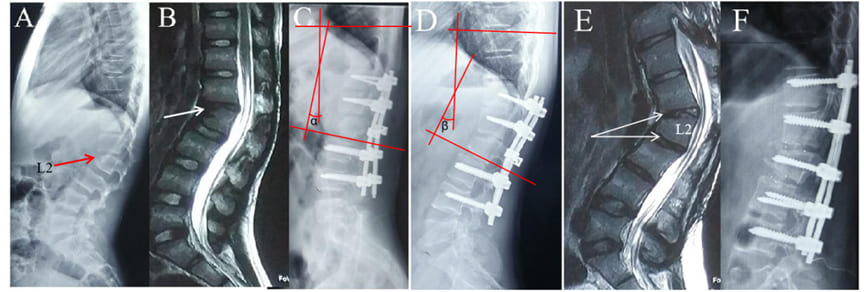
Figure 2: Loosening of screws and kyphosis deformity. A-C: Pedicle screw system were performed in the treatment of L2 fracture(∠α=10°). MRI showed anterior column defect of L2 vertebral body and degeneration of L1/2 intervertebral disc with Pfirrmann grade IV. D-F: After 1 year of follow-up, X-ray revealed loosening of the T12 screw and kyphotic deformity of the spine(∠β=21°). After removal of the screw, the MRI showed degeneration of the L2/3 intervertebral disc graded as Pfirrmann grade IV. The patient underwent intervertebral fusion surgery eventually and obtained healing effect.
|
Complications of internal fixation |
P Value |
||
|
Yes (n=12) |
No (n=77) |
||
|
Anterior column defect (Yes/No) |
7-May |
May-72 |
<0.001* |
|
Posterior column injures (Yes/No) |
11-Jan |
Mar-74 |
0.49 |
|
Other (Yes/No) |
9-Feb |
May-74 |
0.169 |
|
ISH-Index (%) |
10.17±1.34 |
8.19±1.59 |
<0.001* |
|
* P<0.05 indicates that difference has statistically significant in two groups. |
|||
Table 5: Complications associated with internal fixation of patients.
Discussion
Currently, more than 60% of traumatic spinal fractures occur in the thoracolumbar region [1]. The posterior pedicle screw fixation technique is a popular treatment method, which involves fixing the injured vertebrae and 1-2 adjacent vertebrae with pedicle screws, and achieving greater initial spinal stability through compression fixation. It also corrects spinal kyphotic deformity, relieves early back pain, and indirectly decompresses the spinal canal [10-12]. In recent years, diseases caused by intervertebral disc degeneration have attracted increasing attention. This not only causes physical discomfort such as cervical and lumbar degenerative diseases, but also brings psychological distress such as fear and anxiety about the disease, resulting in long-term negative effects on social therapy, healthcare, and economic development. It has been reported that in the general population, as high as 70-80% of healthy adults have varying degrees of intervertebral disc degeneration [13]. Intervertebral disc degeneration has been widely recognized as a prerequisite and basis for various diseases of the cervical and lumbar spine in previous literature. However, there is no literature reporting the impact of intervertebral disc degeneration on the clinical efficacy of postoperative reduction and fixation of traumatic thoracolumbar vertebral fractures. It is also inconclusive whether isolated posterior lateral screw fixation requires additional interbody fusion. In the long-term follow-up of intervertebral disc degeneration after thoracolumbar vertebral fractures, early intervertebral disc injury often plays an important role. Su et al.[14] analyzed 56 patients with single-segment thoracolumbar vertebral fractures, and all patients underwent MRI examination. They found that more than 82.1% (46) of patients had intervertebral disc injury, and at the same time, they pointed out that the incidence of intervertebral disc injury in the adjacent disc above the injured vertebra was 82.1%, and 30.2% in the adjacent disc below. Yeol et al. [15] analyzed the MRI results of stable thoracolumbar burst fractures and found that more than 54.1% had intervertebral disc injury. It can be seen that intervertebral disc injury is not uncommon in thoracolumbar vertebral fractures, and the intervertebral disc above the fracture is more susceptible to injury. The causes of intervertebral disc injury in thoracolumbar vertebral fractures are varied and currently lack a unified mechanism. They are often caused by activities, traffic accidents, falls from heights, etc. [16,17]. Stable thoracolumbar burst fractures are mainly caused by axial compression forces, which often result in damage to the anterior and middle columns of the spine. The posterior column often leads to pedicle fractures or no visible fracture. Lin et al. [18] found that vertebral body, superior adjacent intervertebral disc, and inferior adjacent intervertebral disc accounted for 38%, 35%, and 27%, respectively, of all unstable factors after thoracolumbar burst fractures, and 60% of vertebral body fractures showed high mobility around the intervertebral disc. Similarly, this study found similar conclusions, with more than 60% of patients with intervertebral disc degeneration in the long-term follow-up of thoracolumbar vertebral fractures having initial disc injuries. The anatomical components of the intervertebral disc include cartilaginous endplates, fibrous rings, and nucleus pulposus, which together form a cartilaginous complex that absorbs and cushions vertical pressure [19,20]. However, large compressive or tensile forces, especially shear forces during fractures, can easily cause disc injuries [21].
In most fractures, the posterior column of the vertebral body remains intact and provides additional fixation points. Literature reports, including those by Yurac et al. [22], have shown that pedicle screw fixation, including the injured vertebra, can provide sufficient stability to correct and maintain kyphotic deformity. In cases of fracture healing with concurrent disc degeneration, vertebral body fracture healing is often easier. However, these studies suggest that secondary deformity loss and disc degeneration are major contributing factors. The results of this study indicate that compared to patients without disc degeneration, disc degeneration can decrease the height of the fractured vertebral body and increase thoracolumbar kyphosis angle at the last follow-up. These differences were not significantly observed in the early postoperative period. Therefore, vertebral fractures with disc degeneration may experience varying degrees of loss in imaging features. This phenomenon may be attributed to the ongoing degeneration of the intervertebral disc during the fracture healing process, which causes further narrowing of the disc space. In addition, the burst fracture results in anterior column damage, and fragmented bone fragments may be absorbed by osteoclasts during the fracture repair process, leading to insufficient bone mass in the anterior vertebral body to maintain its height. Consequently, it becomes challenging to maintain anterior column height, resulting in height loss, while the posterior column remains stable. This disrupts the biomechanical equilibrium and stability of the spine, further concentrating pressure on the anterior column, exacerbating thoracolumbar kyphosis. Therefore, it is crucial to reconstruct and maintain stability in the anterior column. During the fracture healing process, the vertebral body usually recovers quickly and fully heals, restoring normal strength. However, due to the avascular nature of intervertebral disc tissue, it cannot self-repair after injury, resulting in loss of disc components, manifested by reduced elasticity and height [23,24].
Meanwhile, this study found that complications related to internal fixation were significantly higher in the group with disc degeneration, including screw fracture and loosening. Bo Zhang et al. [25], when discussing the reasons for pedicle screw fracture after posterior vertebral pedicle screw fixation, pointed out that inappropriate surgical techniques and indications were among the causes of complications related to internal fixation. Among them, screw fracture is most common in burst fractures, and he believed that this type of fracture should not be treated with posterior fixation alone. However, in this study, we found that not all burst fractures are prone to complications related to internal fixation. When disc degeneration is accompanied by anterior column defect or endplate injury, the incidence of screw loosening and fracture increases significantly. Untreated thoracic burst fractures can easily progress to spinal kyphosis deformity. However, there is no evidence in the literature to strongly support a specific surgical approach, and there is still controversy regarding the surgical treatment of these common injuries in young individuals [26,27]. If the indications are not properly selected, the postoperative loss rate of internal fixation exceeds 40% [28,29]. Dengwei et al. [30] adopted laminectomy, fracture reduction, and removal of intervertebral discs followed by bone graft fusion to treat thoracolumbar fractures with severe intervertebral disc injury, reconstructing the stability of the anterior and middle columns. The postoperative fracture region obtained good orthopedic results, which were maintained in the long term. Therefore, we believe that when disc degeneration occurs with anterior column defects or endplate injuries, posterior fixation alone is not enough, and intervertebral disc removal with interbody fusion should be performed to prevent excessive loss of kyphotic curvature, leading to failure of internal fixation or even revision surgery.
This study has certain limitations. Firstly, due to its retrospective design, we were unable to further differentiate between degeneration caused by intervertebral disc injury and non-traumatic degeneration. Therefore, further research is needed to explore the specific reasons for postoperative imaging results of intervertebral disc degeneration. Secondly, the loss of anterior column height was not clearly distinguished as either loss of intervertebral space height or loss of vertebral body height, which should be further investigated in future studies. Lastly, the small sample size can lead to selection bias, and thus it is necessary to expand the study sample further.
Conclusion
Superior Disc-Endplate Complex Injury leads to a greater loss of fracture segment height and increased kyphotic deformity angle which combined with anterior column defectc may be the risk factor for the increase of internal fixation related complications in thoracolumbar fractures.
Funding
This study was supported by the Bureau of Science and Technology of Hebei Province (NO. 21377770D) and the Department of Hebei Health Commission (NO. 20221384).
References
- Leucht P, Fischer K, Muhr G, Mueller EJ (2009) Epidemiology of traumatic spine fractures. Injury 40: 166-172.
- Wang F, Tong T, Miao DC, Wang LF, Shen Y (2022) Clinical correlation between osteoporotic thoracolumbar vertebral compression fractures and lumbar spondylolisthesis. Int Orthop 46: 1095-1100.
- Spiegl UJ (2022) Effect of subsequent vertebral body fractures on the outcome after posterior stabilization of unstable geriatric fractures of the thoracolumbar spine. BMC Musculoskelet Disord 22: 1064.
- Song X (2023) Percutaneous versus open posterior stabilization and decompression in AOSpine-type A3 thoracolumbar fractures with neurological deficit. BMC Musculoskelet Disord 24: 385.
- Hirahata M (2022) Vacuum phenomenon as a predictor of kyphosis after implant removal following posterior pedicle screw fixation without fusion for thoracolumbar burst fracture: a single-center retrospective study. BMC Musculoskelet Disord 23: 94.
- Reinhold M (2010) Operative treatment of 733 patients with acute thoracolumbar spinal injuries: comprehensive results from the second, prospective, Internet-based multicenter study of the Spine Study Group of the German Association of Trauma Surgery. Eur Spine J 19: 1657-1676.
- Millecamps M, Stone LS (2018) Delayed onset of persistent discogenic axial and radiating pain after a single-level lumbar intervertebral disc injury in mice. Pain 159: 1843-1855.
- Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26: 1873-1878.
- Moser M (2023) The association between vertebral endplate defects, subchondral bone marrow changes, and lumbar intervertebral disc degeneration: a retrospective, 3-year longitudinal study. Eur Spine J 32: 2350-2357.
- Tanasansomboon T (2022) Thoracolumbar Burst Fracture without Neurological Deficit: Review of Controversies and Current Evidence of Treatment. World Neurosurg 162: 29-35.
- El Behairy HF (2020) Short-Segment Fixation of Thoracolumbar Fractures with Incorporated Screws at the Level of Fracture. Orthop Surg 12: 170-176.
- Cirillo JI (2023) Surgical timing prevails as the main factor over morphologic characteristics in the reduction by ligamentotaxis of thoracolumbar burst fractures. BMC Surg 23: 166.
- Madigan L, Vaccaro AR, Spector LR, Milam RA (2009) Management of symptomatic lumbar degenerative disk disease. J Am Acad Orthop Surg 17: 102-111.
- Su Y, Ren D, Zou Y, Lu J, Wang P (2016) A retrospective study evaluating the correlation between the severity of intervertebral disc injury and the anteroposterior type of thoracolumbar vertebral fractures. Clinics 71: 297-301.
- Lee KY, Kim MW, Seok SY, Kim DR, Im CS (2017) The Relationship between Superior Disc-Endplate Complex Injury and Correction Loss in Young Adult Patients with Thoracolumbar Stable Burst Fracture. Clin Orthop Surg 9: 465-471.
- Doud AN (2015) Has the incidence of thoracolumbar spine injuries increased in the United States from 1998 to 2011? Clin Orthop Relat Res 473: 297-304.
- Yang M (2019) Comparison of clinical results between novel percutaneous pedicle screw and traditional open pedicle screw fixation for thoracolumbar fractures without neurological deficit. Int Orthop 43: 1749-1754.
- Lin RM, Panjabi MM, Oxland TR (1993) Functional radiographs of acute thoracolumbar burst fractures. A biomechanical study. Spine 18: 2431-2437.
- Ozdemir B (2017) Restoration of Anterior Vertebral Height by Short-Segment Pedicle Screw Fixation with Screwing of Fractured Vertebra for the Treatment of Unstable Thoracolumbar Fractures. World Neurosurg 99: 409-417.
- Mahar A (2007) Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine 32: 1503-1507.
- Baaj AA (2011) Biomechanical advantage of the index-level pedicle screw in unstable thoracolumbar junction fractures. J Neurosurg Spine 14: 192-197.
- Yurac R, Marré B, Urzua A, Munjin M, Lecaros MA (2006) Residual mobility of instrumented and non-fused segments in thoracolumbar spine fractures. Eur Spine J 15: 864-875.
- Oner FC (1999) Correlation of MR images of disc injuries with anatomic sections in experimental thoracolumbar spine fractures. Eur Spine J 8: 194-198.
- Theodorou DJ, Theodorou SJ, Kakitsubata S, Nabeshima K, Kakitsubata Y (2020) Abnormal Conditions of the Diskovertebral Segment: MRI With Anatomic-Pathologic Correlation. AJR Am J Roentgenol 214: 853-861.
- Zhang B, Wang JC, Jiang YZ, Song QP, An Y (2022) Effectiveness and postoperative rehabilitation of one-stage combined anterior-posterior surgery for severe thoracolumbar fractures with spinal cord injury. World J Clin Cases 10: 6001-6008.
- Suer O, Aydemir S, Kilicli B, Akcali O, Ozturk AM (2024) Should the level of the posterior instrumentation combined with the intermediate screw be a short segment or a long segment in thoracolumbar fractures with fusion to the fractured segment? Eur J Trauma Emerg Surg 2024.
- Xu GJ (2013) Anterior versus posterior approach for treatment of thoracolumbar burst fractures: a meta-analysis. Eur Spine J 22: 2176-2183.
- Butt MF (2007) Management of unstable thoracolumbar spinal injuries by posterior short segment spinal fixation. Int Orthop 31: 259-264.
- Moura DL (2024) The role of kyphoplasty and expandable intravertebral implants in the acute treatment of traumatic thoracolumbar vertebral compression fractures: a systematic review. axOpen Rev 9: 309-322.
- He D, Wu L, Chi Y, Zhong S (2011) Facet joint plus interspinous process graft fusion to prevent postoperative late correction loss in thoracolumbar fractures with disc damage: finite element analysis and small clinical trials. Clin Biomech 26: 229-237.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.