Eco-Audit of the Da Vinci Robot in Minimally-Invasive Surgery: A Comparison with Conventional Technique for Lobectomy
by Arnaud Patoir1, Minh-Quyen Le2*, Usha Seshadri Kreaden3, Fahmida Bangert3, Jean-François Mogniotte2, Jean-Fabien Capsal2, Guilhem Rival2, Nellie Della Schiava2,4, Pierre-Jean Cottinet2*
1RAMSAY Santé, Hôpital privé de la Loire (HPL), 39 boulevard de la Palle, 42100 Saint Etienne, France
2INSA Lyon, LGEF, UR682, 69621 Villeurbanne, France
3Biostatistics and Global Access & Evidence Management, Intuitive Surgical, Sunnyvale, CA, USA
4Department of Vascular and Endovascular Surgery, Hôpital Louis Pradel, Hospices Civils de Lyon, Bron, France
*Corresponding authors: Minh-Quyen Le and Pierre-Jean Cottinet, INSA Lyon, LGEF, UR682, 69621 Villeurbanne, France
Received Date: 10 March, 2025
Accepted Date: 18 March, 2025
Published Date: 21 March, 2025
Citation: Patoir A, Le M-Q, Kreaden US, Bangert F, Mogniotte J-F, et al. (2025) Eco-Audit of the Da Vinci Robot in MinimallyInvasive Surgery: A Comparison with Conventional Technique for Lobectomy. J Community Med Public Health 9: 510. https://doi.org/10.29011/2577-2228.100510
Abstract
This study provided an important profile of the carbon footprint resulting from a lobectomy operation conducted in the HPL (a private hospital of Loire, France) using RATS (robotic-assisted surgery with da Vinci platform) and conventional VATS (video-assisted surgery with laparoscope) techniques. Our analysis aims to quantify their carbon impact and identify major sources of energy expense according to the eco-audit method. A mitigating indicator based on an estimation of the green-house emission (GHE, in kilogram carbon dioxide equivalent emissions) has been provided, which depends on materials’ quantity and emission factors computed from the life-cycle-assessment (LCA) software. For the same procedure, the RATS lead to ~ 32% higher carbon impact with respect to the conventional VATS. It has been demonstrated that, whatever the technique is chosen (either with or without robot), the majority of surgical tools consume the most energy for production and manufacture. Inversely, little electrical power is needed during use, as most of them are passive and their lifetime is relatively short (i.e., minute tools for single use like needles, scalpels, scissors, forceps, etc.). Development of sustainable surgical devices with the possibility of being reusable or recycling seems to be an interesting alternative to drop carbon emission. Nonetheless, the reusable set needs significant energy for washing and steam sterilization, which has a higher carbon impact than the disposable counterpart. Recycling plastics and metals, together with the use of bio-polymers instead of oil-based polymers might reduce the environmental burden. However, what is the price, the surface of land, as well as the water consumption needed to fabricate those bio-polymers? Also, what is the full LCA for recycling and reusing? Before going further with reflection and decision, we need to look objectively at the concrete situations to identify advantages and conveniences of each measure. These concerns, accompanied by scientific and methodological analyses, will be revealed in this study.
Keywords: Carbon footprint; Eco-audit; Life cycle assessment; Da Vinci robot; Minimally-invasive surgery; Recycled/reusable/ sustainable materials
Introduction
Robotic surgery has the features to represent the future of surgery, considering the rapid evolution of its technology and the resulting in the surgical field. In the last years, the robotic technique in thoracic surgery has progressively become widespread in the word, particularly for the treatment of the mediastinal and pulmonary lesions [1]. The development of technology in the robotic system has been associated with the improvement of intraoperative and postoperative results. Due to the satisfying results and increasing experience and confidence with the robotic technique, surgeons are consequently enlarging the surgical indication, moving to increasingly challenging cases [2]. Robotic surgery is being affirmed as a safe technique also for those complex cases, which in the past were considered a matter solely for laparoscopic surgery. In fact, robotic surgery is increasingly associated with positive surgical results and guarantees less traumatism and a fast recovery to the patients. These positive results have resulted from the evolution of the technique, which has developed in parallel with the evolution of the technology, exploiting to its best the latest features of the robotic system. The Da Vinci robotic surgical system is the focus of ongoing research to assess its clinical utility and costs. The impact of those robotic-assisted procedures on the environment, however, has not been fully assessed. Health care itself contributes to climate change. With hospitals consuming ~5% of European energy (~9% in US), and contributing 2.6 kg/ bed/day of European waste to landfills each day (~3.8 kg/bed/day in US) [3], we sought to investigate the sustainability of this new, technology-driven surgical modality.
Advanced general thoracic lobectomy can be performed safely with the da Vinci™ robot allowing precise dissection in remote and difficult-to-reach areas [4,5]. Novellis, et al. pointed out that robotic surgery for early lung cancer was associated with shorter stay and more extensive lymph node dissection than conventional open surgery [6]. Although the cost of robotic surgery is high, the hospital makes a profit. The aim of this work is not to evaluate the applicability of the da Vinci™ operation robot for general lobectomy procedures. The potential benefits and limitations of using the robotic platform for the performance of such procedures have been recently intensively explored in literatures [7,8]. Here we focus on the carbon footprint generated by lobectomy surgery, with a particular emphasis on the use of the da Vinci robot. This study, to the best of our knowledge, has not been investigated much in the healthcare research community.
The healthcare sector is a driver of economic growth, but it is also a significant source of emissions that adversely impact environmental and public health [9-12]. It has the largest carbon footprint of any service sector and is responsible for 4-5% of global carbon emissions [13]—more than aviation and shipping combined. The main contributors are medicines (including inhalers), anesthetic gases, patient and staff transport, heating and cooling facilities, electricity use, waste management, and food and catering. Climate change has become a considerable healthcare threat of the 21st century, and healthcare itself produces greenhouse gases directly, but also from indirect emissions associated with consumption of goods and services [14,15]. The Operating Room (OR) is the most resource-intensive area of a hospital, and surgery is therefore an important focal point to understand healthcarerelated emissions [16]. Life Cycle Assessment (LCA) results show that major sources of environmental emissions include the production of disposable materials and single-use surgical devices, energy used for heating, ventilation, and air conditioning, and anesthetic gases [17]. Hospitals are beginning to scientifically evaluate the source of negative environmental impacts in current medical practice, specifically in regard to energy, but there is little research on environmental impacts. With better information, healthcare innovators can strategically optimize the transition to a more sustainable system, while maintaining or improving the safety, comfort, and health outcomes of patients [18].
In order to further understanding healthcare-related carbon footprint, this study use the eco-audit method to estimate the CO2 quantity delivered by an operation [19]. Environmental impact is then compared between the RATS and the conventional VATS counterpart. A prospective LCA of most medical tools and devices used during a surgical procedure in the HPL were analyzed one-by-one to identify their essential characteristics (weight, composition of materials, country of fabrication, medical standards). These input data are then collected to convert to the energy or carbon footprint via EduPack library software. Recently, we have published several LCA topics in medical field using this library such as evaluation of routine anatomic pathology practices [20]; environmental impact of capsule endoscopy [21] or of adalimumab biosimilars in rheumatology [22]; carbon footprint analysis of an atrial fibrillation catheter ablation procedure [23], and also in the case of heart surgery procedures for mitral valve repairing [24]. However, none of these studies, as well as those found in literature, have yet been reported on the environmental impact of minimally invasive surgery (MIS) using robotic tools. It is therefore expecting that analyses explored in this research would bring a meaningful contribution to the field of MIS where the assistance of robots does not stop increasing and seems to be getting more popular these days.
Methods
Ethics and patient selection
The information and date available in this work are prospective, observational, and single-center study (Hôpitaux privé de la Loire, abbreviated as HPL). This establishment is among the 50 French centers, public or private, exercising this discipline in high volume (more than 30 procedures/year/surgeon). Neither clinical nor personal data related to the patients were collected aside from the type of surgery, which cleared us from any Institutional Review Boards’ and ethics committee’s approval requirements.
Only lung cancer surgery (so-called lobectomy) in adults were considered for the eco-audit. This procedure is well standardized in France as well as in other European countries. It consists in the removal of an anatomical part of a lung (lobe) that contains the tumor, with systematized interlobar and mediastinal lymph node dissection.
Functional units
The present study reports on two functional units for which the carbon footprints were separately evaluated and compared: (i) Video-Assisted Thoracoscopic Surgery (VATS); and (ii) RobotAssisted Thoracoscopic Surgery (RATS). No clinical data from patients were collected. As illustrated in Figure 1 (a)-(b), two workstations were identified including the anaesthesia, and the surgical workstation. The need for surgery was considered essential and, therefore, the analysis used traditional laparoscopic surgery (VAT) as the comparator. Other components of the overall carbon footprint common to surgery in general (i.e., operating theatre, electricity use, patient travel, paper products used) were considered equivalent. Only additional aspects unique to robotic tools were considered in the analysis.
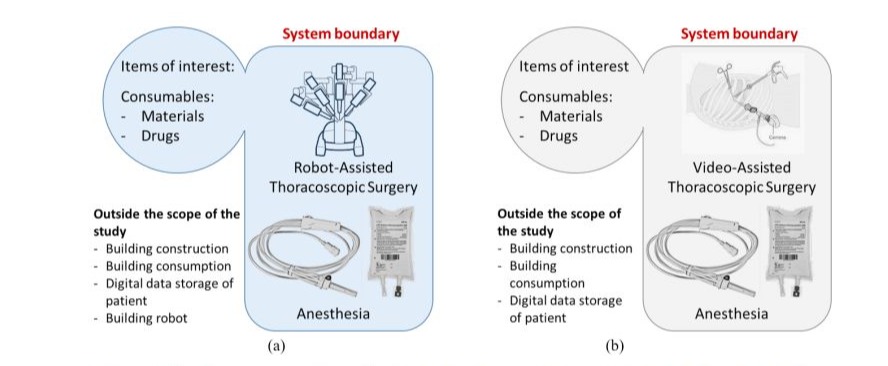
Figure 1: Workflow in the procedure of lobectomy based on two functional units: (a) RATS; and (b) VATS.
To evaluate the carbon footprint of VATS or RATS, the different steps for those procedures, from the arrival of the products to their archiving and destruction (end-of-life). The system studied was delimited (system boundary) and included all the steps of VATS and RATS. The functional units of the study were chosen as the procedure per patient that included consumables like materials and drugs. The elements not integrated in this system are considered as outside the system boundary such as the electricity consumption of building, and the carbon footprint of the transportation mode of the staff members.
Collection of emission factors for GHE assessment
For each procedure previously selected, data were prospectively collected during 2023 by medical staff (A.P. and N.D.S.) from the HPL. The emission factors determined for materials, packaging, and drugs was performed by an independent team of scientists (P-J.C. and M.-Q.L.) from the LGEF Research Laboratory. Greenhouse emission (GHE) was expressed as kg CO2 equivalent for an easier comparison with the carbon lifespan and its global warming potential. The total impact is the sum of each inventory data multiplied by its specific emission factor: total impact = Σ(inventory data × emission factor) as presented in Figure 2 (a). The emission factors, commonly found in literatures [25], were multiplied by the mean quantity of materials used per functional unit previously collected. In case of unavailable information from the literatures, each step of the reaction to produce the reagent was modeled using the chemistry research platform “SciFinder” (CAS SCIFINDER, Colombus, OH, USA).
For the carbon footprint analyses of materials and packaging, the software of library Ansys Granta EduPack® (i.e., possibly being downloaded from the website [26]) was used based on the “ecoaudit” method proposed by Ashby [19]. This software allowed for an estimation of the GHE of a product, from its raw material to final use, throughout each phase of the Life Cycle Assessment (LCA) including material production, product manufacturing, transport, and end-of-life as displayed in Figure 2 (b). The main challenge of this study is to correctly identify all original substances of each medical device with their origin, knowing where they came from. On the one hand, brief information can be found directly on the label of the products, but on the other hand, referring the CE marking to get more complete data can be an alternative solution. If both methods do not provide enough details about the main constituents of the medical tools, further engineering tests can be involved such as DSC, X-ray, and microscopy analysis. Generally, these approaches make a possibility to decompose each medical device into a subset of elementary material, allowing them to accurately determine its environmental impact based on the ecoaudit procedure. However, in some special cases, several products are not in the database, it was therefore necessary to contact the manufacturer to find the equivalent products.

Figure 2: (a) Conversion of inventory data into equivalent CO2 emission; (b) Diagram of the LCA split into different phases from raw material to final use.
Transportation is also a complex issue, and its environmental implication can be estimated based on the manufacturing location written on the label of each product. Also, some hypotheses can be taken from the logistical circuit. The last consideration relates to the electrical consumption of several active devices like scalpels, robots, etc. used throughout the procedure of lobectomy. This information can be found directly on the device’s label. On the other hand, most of the materials used in MIS procedure is passive, which does not consume any energy during use. Therefore, the largest source of electricity consumption in an Operating Room (OR) are not the medical equipment, but rather the other power usages like lighting, cooling (air conditioning, ventilation), and heating systems. Figure 3 revealed that for a typical healthcare building, cooling and the heating systems represent approximately 50% of annual demand for electric energy [27,28], and only 12% for the other equipment of which very small portion dedicated to the medical devices used in OR. Similar results are also reported in [29,30]. The data provided by the HPL, corresponding to energy expended by the hospital (with total consummation of 680 kWh/ m²/year). Considering 36 m² is a standard surface of the OR, it is possible to estimate the electric power used for one operation (~2.6 kWh). The corresponding gas emission. In France, each kWh of electricity generated over the lifetime of a nuclear plant has CO2 footprint of 0.05-0.1 kg. In US where electricity principally generated by coal, natural gas, and petroleum, the CO2 emission per kWh is much higher, about 0.4-1 kg. In the case of this study, an equivalent of 0.1 kg CO2 per kWh has been considered.
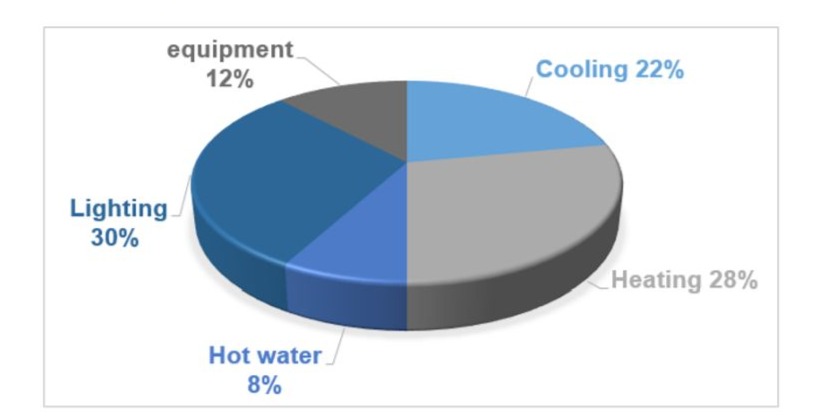
Figure 3: Electric consumption for end-users in healthcare center of the HPL: Distribution of annual energy demand by sector for a typical hospital building.
Analysis of da Vinci robot’s tools based on eco-audit study
Robotic technology allows surgeons to operate with extreme precision. Areas of the body that may difficult or even impossible to reach with the human hand are now accessible with use of the robotic system; its “arms” can rotate up to 280°. The Da Vinci robot is a laparoscopic platform in which a computer-controlled robot assists surgeons during the procedure, with an increased level of dexterity and allows them to operate in small spaces inside the body. It also allows surgeons to perform very delicate or complex surgical procedures that may have been challenging or even impossible without the aid of the robot.
Implementation of da Vinci robot in surgical field
The da Vinci system comprises three distinct subsystems: (i) the patient-side cart; (ii) the surgeon console; and (iii) the vision cart. The working principles of the robot are schematically illustrated on Figure 4. In general, surgeon is seated at a surgeon console, from which they control the motion of surgical instruments that are situated at the patient side, as well as observe video images from inside the patient. The manipulators are mounted to the patient-side cart via a setup structure [31]. Each manipulator may support either a stereo endoscopic camera or a surgical instrument, such as a grasper, a scissor, or a needle driver. Due to their contact with the patient, these instruments work within the sterile field, whereas the surgeon and the console remain outside of the sterile field. The computerized control system extends the surgeon’s “presence” their sensory awareness and control into the surgical field by transmitting video images from the endoscopic camera to the stereo viewer of the console. Similarly, the surgeon’s hand motions measured by the master interfaces is also conducted to the slave manipulators. Since this is an electronic link, the software of the control system can modify the signals, so as to filter out the surgeon’s normal physiological tremor, or to scale down their motions for enhanced precision. Figure 4 gives the typical electric power consumption for one operation, which will participate in the calculation of the carbon impact based on the ecoaudit method.
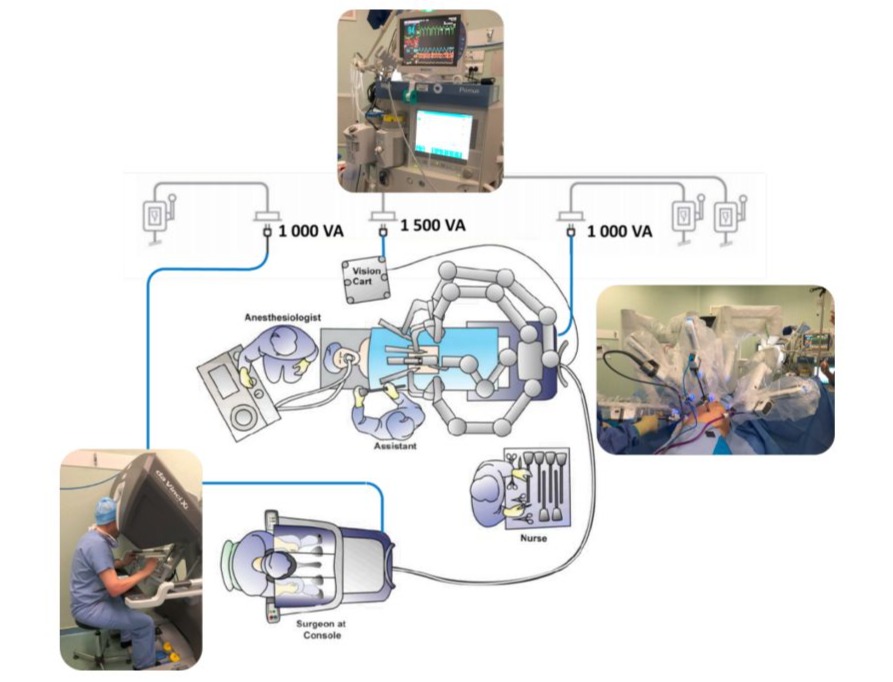
Figure 4: The configuration of the Da Vinci robot system in surgical field and power consumption.
A family of instruments has been developed for the da Vinci system in order to facilitate tissue manipulation in various types of surgical procedures. Many of these instruments have an articulated wrist mechanism to allow for dexterous and intuitive tissue interaction, following the surgeon’s wrist articulation while controlling motion from the master interfaces of the surgical console. EndoWristfi is the trade name for these articulated instruments, which include various types of scissors, forceps, needle drivers, retractors, monopolar and bipolar energy instruments, stabilizers, staplers, and vessel sealers. In the following subsection, we focus on two of the most advanced instruments used in the lobectomy intervention:
EndoWrist stapler 45 (Maryland), and Vessel Sealer instrument.
EndoWrist stapler
The EndoWrist stapler, an articulated surgical device, allows surgeons to control the positioning and firing of a reload (staple cartridge) that places multiple staggered rows of staples and transects the tissue with a knife blade. The result is a clean division of tissue with no bleeding. The stapler instrument can be reloaded multiple times with stapler reloads, these are disposable and contain both staples and a knife blade [32].
The stapler instrument as shown in Figure 5 (a) has two opposing jaws and six degree of freedom (DoFs): roll, pitch, yaw, grip, “clamp,” and “fire”. Roll, pitch, yaw, and grip are used to position the upper and lower jaws of the instrument relative to the target tissue and are controlled in the same manner as other EndoWrist instruments, via master manipulators on the surgeon console. The term “clamp” is the same motion as grip but uses a different mechanism to provide significantly higher grip force. The term “fire” describes the combined action of implantation of staples and transection (translating blade) of the target tissue. Both functions are activated and controlled by the foot pedals at the surgeon console. The lower jaw of the instrument houses the staple reload; the upper jaw contains features which “form” the staples such that they remain implanted in the tissue.
Figure 5 (b) depicts the split view of the da Vinci Xi EndoWrist stapler 45 composing of different elements like bearing spring, PCB, polymers, and so on. The weight fraction of the stapler is displayed on Figure 5 (c), indicating an important quantity of stainless steel (~80% wt.) used in the stapler. The most common “surgical steels” are austenitic SAE 316, martensitic SAE 440, SAE 420, and 17-4 stainless steels [33]. There is no formal definition on what constitutes a “surgical stainless steel”, so product manufacturers and distributors often apply the term to refer to any grade of corrosion resistant steel. To obtain the CO2 equivalent computed from the Eco-audit algorithm, a specific ASM Materials Database has been employed to identify different materials used in the stapler tool. Based on this document, it can be assumed that all the materials come from Mexico. The eco-audit bar graph of the stapler is illustrated in Figure 5 (d). Similar to most passive products, the stapler does not consume any electric power, and it can be reused 7 times (or 7 patients with ~50 clips) after sterilization. This explains why the manufacture stage has a low carbon impact, which is contrary to the cases of material production and transport.
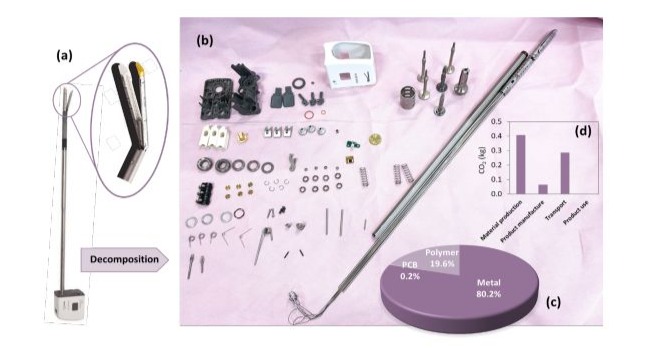
Figure 5: Da Vinci Xi EndoWrist stapler 45: (a) illustration of the whole instrument; (b) split view; (c) mass fraction (in %) of different materials; and (d) Eco-audit bar chart of CO2 emission.
Vessel sealer instrument
Another instrument currently used in robotic surgery is a sealer. The da Vinci EndoWrist One Vessel Sealer shown in Figure 6 (a) is a disposable advanced bipolar cautery instrument that seals and cuts vessels up to 7mm in diameter. By applying precise pressure and controlled energy delivery, soft tissue proteins denature within the range of 60-90°C, hence the inside wall of the vessel is melted (or fused) together. Energy delivery is controlled based on tissue impedance measurement during sealing, so as to maintain temperature within a range that results in sealing rather than charring or burning. Once sealed, the vessel can be transected by firing a mechanical knife that moves along the length of the instrument jaws, in a slot through the center of the electrodes.
Figure 6 (b)-(c) displays the split view of the device as well as the weight content (in %) of the different family of materials (i.e., polymer, metal, and PCB), confirming an important fraction of polymer used for the fabrication of the sealer. For such reusable instruments, it is well known that PPSU (PolyPhenylSulfone), PAEK (PolyArylEtherKetone), and PEEK (PolyEtherEtherKetone) are considered as the best candidates. These three high-performance medical-grade polymers offer unparalleled strength and toughness combined with high-temperature tolerance and chemical resistance to support surgical instruments that require repeat use and repeatcycle steam sterilization. Moreover, they are resiliently capable of withstanding repetitive use and sterilization methods without any significant loss of physical or mechanical properties.
Figure 6 (d) represents the carbon footprint of the da Vinci Vessel Sealer, which is of similar trend to the stapler shown in Figure 5 (d). The most important CO2 quantity of sealer has come from the material production and the transport, while being significantly lower for the product manufacture, because of its reutilization 7 times after sterilizing. Although the sealer uses electric power to measure the tissue impedance during sealing, this consumption is not continuous, and the power is ON for a very brief time (few seconds). It can be thus assumed that the product use of the sealer provokes no carbon impact as opposed to the other activities of the life cycle.
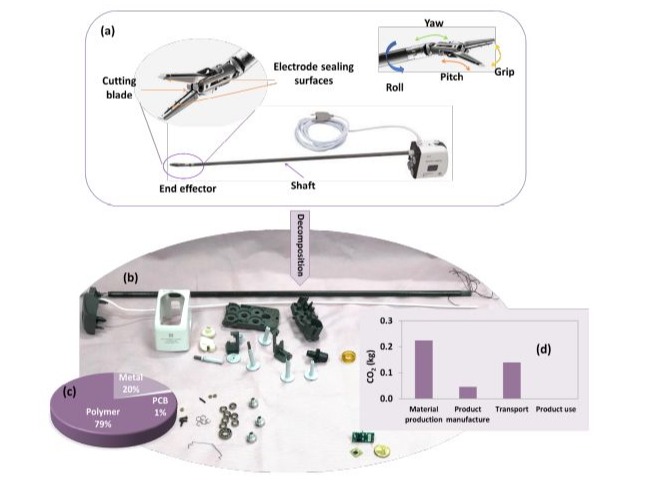
Figure 6: Da Vinci Vessel Sealer: (a) illustration of the whole instrument; (b) Split view; (c) the mass distribution of different materials; and (d) Eco-audit bar chart of CO2 emission.
Data analysis
Compared to traditional VATS, robotic surgery results in smaller incisions, which reduce pain and scarring, lead to less time spent in the hospital and quicker recovery times. Thus, the benefit of robotic surgery is evident for both surgeon and patient. However, its environmental impact is not always clear. The discussion here allows us to reveal some important points related to this issue.
RATS versus VATS: what is their carbon footprint?
Figure 7 (a)-(b) shows what eco-audits look like regarding the CO2 emission for the lobectomy lung surgery using two different interventions including RATS and VATS. Whatever the intervention, two main blocks are simultaneously performed comprising anaesthesia and surgical field. Materials used in anaesthesia procedure are assumed to be similar in both RATS and VATS, but not in the case of surgical field. The analyses clearly indicate that the total carbon emissions from the conventional VATS are less than the RATS, which is mainly caused by the energy spending and an important single use surgical instrument (except the stapler). On the one hand, robotic treatment is more expensive and polluting. On the other hand, it is associated with a shorter length of hospital stay and higher patient satisfaction, probably with better treatment outcomes and reduced complications.

Figure 7: Carbon-footprint bar chart of two types of lobectomy surgery (a) RATS; and (b) VATS.
The results in Figure 7 reveals that surgery leads to the highest consummation in energy to produce and manufacture materials, involving a high impact on the environment. Although transportation cannot be negligible, as 65% of international medical devices come from Asia and very few of them are fabricated in EU (see Figure 8), but the carbon footprint caused by this sector is notably lower than the production and manufacture phases. Accordingly, for the two blocks (surgery, anaesthesia), the material production expends far more energy than all the other phases of life. On the other hand, little energy is required during use, since most medical tools (syringe, needle, scalpel, scissors, forceps, etc. for cutting, dissecting, holding, and so on) are passive and consume practically no electric power. Furthermore, their lifetime is short because the majority are minute-tools for single use only. Thus, these materials cause the largest contribution in the embodied energies and the carbon footprint for production and manufacture.
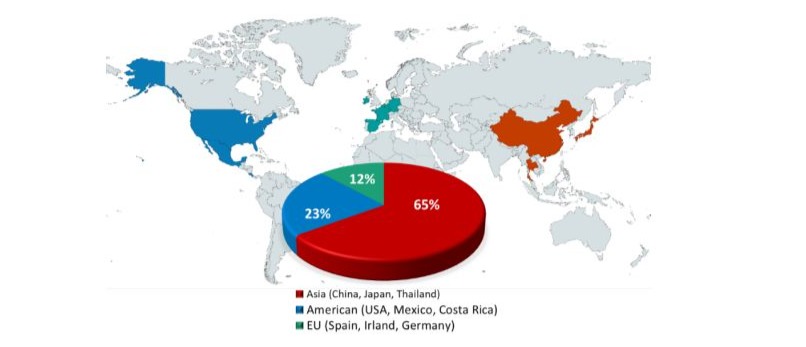
Figure 8: International medical device distributor network.
It is worth noting that the CO2 footprint in transport can be fluctuated, which is determined by the means of transportation (boat or airplane) used for delivery of medical devices. In our case, when differences are as great as those of the bars (Figure 7), high precision is not needed because it is the ranking that matters. Modest changes to the input data leave the ranking unchanged. Consequently, fluctuation of the two last phases of life (transport and use) does not affect much the total embodied energy as well as the CO2 footprint, which mainly caused by a colossal quantity of single-use disposable devices during the lobectomy surgery. Our study highlights that for one procedure in the HPL, whatever type of procedure (with or without assisted robot), more than 20 wt.% of these materials is packaging that will end up in landfill. This is considered to be not only wasteful in terms of demand for precious space in landfill sites, but represents a waste of resources that could and should be recovered and reused. Therefore, designing packaging to make it easier to recycle is hugely important. According to the P&PWD (Packaging and Packaging Waste Directive) [34], all packaging placed on the EU market must meet three essential requirements: 1) minimizing the amount of packaging to achieve the desired purpose, 2) limiting maximum specified hazardous substances, and 3) using environmentally sustainable materials.
A comparison of the total equivalent CO2 (per procedure) between the two MIS techniques (i.e., laparoscope versus robot) are summarized in Table 1, which is deduced from the eco-audit calculation of Figure 7. Obviously, the traditional VATS is more friendly environmentally, as more equipment and materials are involved in the RATS. Accordingly, robotic surgery consumes 32% more energy than the conventional procedure, resulting in a total of 105 kg equ. CO2 as opposed to 71 kg. This discrepancy seems to be acceptable by considering the high benefits of the robot to both surgeon and patient. It is possible to convert the CO2 emission to a daily action, e.g., the number of kilometers travelled by car. No official international database exists as an international reference for calculating CO2 emissions related to a specific activity or daily activities. Here we use the data proposed by the ADEM, i.e., 98.1 g of CO2/km [35]. Similar differences in carbon emissions between intervention methods are likely to be seen throughout the healthcare system laparoscopy [17].
|
Type |
Equ. CO2 (kg) |
Car travelling (equ. km) |
|
Robotic surgery (RATS) |
105 |
1070 |
|
Conventional surgery (VATS) |
71 |
723 |
|
Difference between two techniques |
34 |
347 |
Table 1: Data used for the carbon footprint calculation of two surgical techniques and the equivalent kilometers travelled by car.
Figure 9 (a)-(b) shows the reparation of the electric power consumption for the two types of surgery. Statistically, RATS has somehow longer duration, and the power consumption increases due to the presence of the patient cart and the surgeon consol. At the end, there is a difference of 0.54 kg equ. CO2 in product use, which is insignificant as opposed to the total difference mainly caused by the material production and the manufacture.
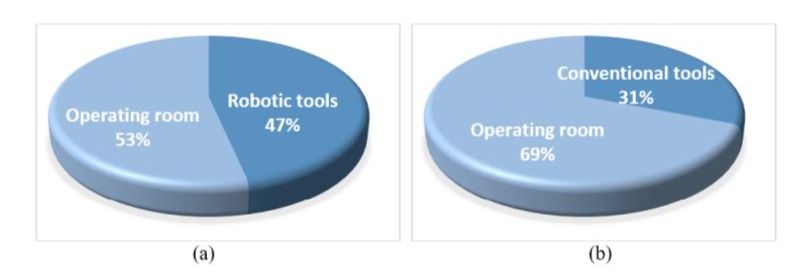
Figure 9: Power electric consumption of CO2 equivalent (in kg) for (a) RATS; and (b) VATS.
Figure 10 (a)-(b) illustrates the carbon footprint repartition in different fields (i.e., patient field dedicated to materials used for preparation, action field dedicated to materials used for operation, and anaesthesia) for the RATS and VATS. In both cases, the action field has the highest carbon impact, which is explained by the fact that the importance of medical tools are used during this procedure. The CO2 repartition is more dispersed in the case of the RATS, reflecting by the high percentage of the action field with the main involvement of the robot.

Figure 10: Carbon footprint repartition in different fields based on eco-audit analysis in two cases: (a) RATS; and (b) VATS.
The host company of the da Vinci robot, Intuitive Surgical, Inc. dominate the global surgical robotics by holding ~ 80 % of the market share in 2020 [36]. According to the annual report of the Intuitive Surgical, Inc. [37], there are ~ 6000 da Vinci Surgical Systems installed worldwide in 2020, including 3,720 in the U.S., 1,060 in Europe, 894 in Asia and 316 in the rest of the world. The total number of procedures of all types performed or assisted by the da Vinci Surgical System in hospitals is estimated to be approximately 1,243,000 throughout the world during the year ended December 31, 2020. This leads to an energy consummation difference between the robotic and conventional surgery, according to the analysis of Table 1, about 42,262,000 kg of equ. CO2, which can be estimated as 431,321,000 km of car travel. Although discrepancy is revealed to be acceptable for each procedure, as the total number of surgical procedures continues rising, the environmental impact of robotic surgery is no longer negligible. Fabrication of robotic tools with reusable options is thus of primary importance to reduce the carbon footprint. This issue, together with sterilization matter are addressed in the following subsection.
Disposable and reusable robotic surgical instruments
Various studies showed that sterilization is a critical process for the environmental footprint. Not all sterilization methods can be used for any materials. As a matter of fact, the ones used in surgical devices must fit the intended sterilization approach [38-40]. The most common methods are gamma irradiation for disposables and local steam autoclave for reusable instruments in hospitals. The energy demand for the steam sterilization of the reusable products has the highest impact on the eco-efficiency [41,42]. On the contrary, negligible environmental impact of the 60Cobalt (60Co) gamma-ray radiation process leads to significant benefits for the disposable set. A crucial issue of such a sterilization technique is high safety standards during transporting and handling the 60Co.
Among other important sources of environmental impacts from surgeries, material consumption due to required instrumentation accounts for up to 65 % of GHE. The outcome of the LCA for using the reusable and disposable set of the surgical instruments (e.g., EndoWrist stapler) in a da Vinci robot is shown in Figure 11. Transportation and disposal processes have minor impacts in both cases. As observed, the main carbon emission of the disposable set is the material production, which is revealed to be drastically higher compared to the reusable set. In other words, reusable robotic tools (e.g., 10 times) are less expensive, consume less materials, and produce less CO2 with respect to their single-use counterparts.
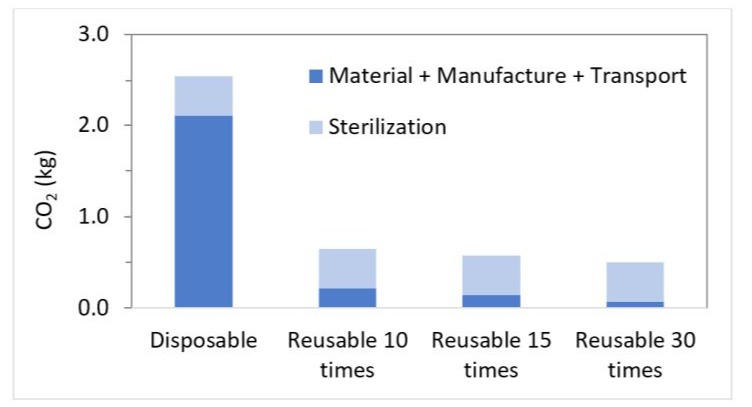
Figure 11: Carbon footprint of EndoWrist stapler (da Vinci robot) with different number of reuses.
Nonetheless, increasing the number of cycles used (from 10 to 30) only induces a moderate decrease in the GHE. Due to the high environmental impact of the cleaning, disinfection and sterilization process, the environmental impact of the reusable system still remains high. Reducing the number of instruments to be cleaned and sterilized for a surgery should be the focus for future surgery instruments development from an environmental perspective [43].
A further step is to systematically measure and reduce emissions from treatment pathways. Thiel, et al. pointed out that lowering the emissions of a laparoscopic hysterectomy without affecting clinical efficacy needed the use of low emitting anesthetic agents, reusable instruments, recycling systems, and a renewable electricity supply [44]. The main contributors to the emissions reduction were switching anesthetic gases and reducing single use materials, both of which may be cost saving. All anesthetic approaches had similar carbon footprints (desflurane and nitrous oxide were not used for general anaesthesia). Rather than spinal being a default low carbon approach, several choices determine the final carbon footprint: using low-flow anaesthesia/total intravenous anaesthesia, reducing single-use plastics, reducing oxygen flows, and collaborating with engineers to augment energy efficiency/renewable electricity. Opportunities to “green” interventions without affecting clinical outcomes are likely to exist across medicine, surgery, and throughout healthcare systems and should be driven by evidence of what works.
To sum up, the materials production and manufacture of medical products is the most energy-intensive while their use-life is extremely short and their CO2 emission during use is minor. The current solution involves great effort to improve energy efficiency in hospital building or reduce CO2 emission during transportation. Unfortunately, those measures are not sufficient to save energy and protect the environment, as the energy of materials production and manufacture largely exceed that of use and transport. Recycling medical instruments could be an alternative to reduce rawmaterial waste, which in turn lower the energy consumption and environment consequences. One relevant question is whether there is any chance of improving circularity in the biomedical sector? A deeper analysis on material constituents of most single-use disposable tools allows us to reveal this concern, to some extent. For more details, interested readers can refer to the supporting information.
Conclusion
In this study, we mainly focus on the medical field with the advanced approach of Minimally-Invasive Surgery (MIS) assisted by da Vinci robot. Robotic-assisted possesses the potential to become the standard of care for lobectomy treatment, with the benefits of Minimally Invasive Technique (MIS). Compared to the conventional method-based Video-Assisted Thoracoscopic Surgery (VATS), the technical features of the da Vinci robotic system, among which the magnification of vision, tremor filter, and a wide range of instruments, allows the lobectomy to proceed in a safer way for patients and easier manipulations for surgeons. Such advancements clearly improve patient outcomes and reduce surgical complications, justifying why the number of RATS is rising exponentially. Unfortunately, the environmental collateral effects of robotic MIS have not been much considered, to the best of our knowledge.
The aim of this research is an attempt to quantitate the carbon footprint of MIS lobectomy through Greenhouse Emissions (GHE) using the eco-audit approach, to identify its potential role in global warming. To better highlight the environmental effects of RoboticAssisted Thoracoscopic Surgery (RATS), a comparison in the GHE factor with respect to the conventional VATS technique has been carried out. The results revealed that both techniques consumed the most energy in producing and manufacturing materials, which are the two phases of life cycles involving the highest impact to the environment. Another phase relating to transport is less energyconsuming, but must be considered as a large part of medical devices come from Asia or South America. On the other hand, little energy is required during use since most medical tools (either with or without robot) are passive and consume practically no electric power. In addition, their lifetime is short because the majority are minute-tools for single use only.
Reusable seems to be an interesting option to reduce the financial and environmental cost of the single-use tools. The reusable devices, however, need steam sterilization that has extremely high carbon impact compared to other techniques. It has been demonstrated in this study that the selected cleaning and sterilization process for the EndoWrist staple 45 (reused 7 times) of the da Vinci robot is responsible for up to 90% of the GHE. Reusable certainly allows to reduce the cost of production and manufacturing materials, but sterilization for reusable (steam in autoclave) needs much more power than the single-use counterpart (i.e., usually sterilized with 60Co gamma-ray radiation). Up to now, no ideal solution could drastically decrease the carbon footprint in the medical field where too many constraints are imposed. Each case should be thoroughly investigated in detail to find out the best compromise for patients and practicians, while achieving sustainable development and environmentally-friendly practices.
It is vital to consider this important time in healthcare, as we make decisions about cost, reform, access, and the impact on future generations. As climate change has become an environmental emergency, medical systems need to investigate ways in which high-quality health care can be delivered while minimizing the environmental impact. Therefore, thanks to advanced robotic technology and to the standardization of surgical procedures, robotic surgery may be able to offer the patients a minimally invasive approach, while respecting the environment based on the development of sustainable, reusable, and recycling devices.
Author Contributions
All authors have read and agreed to the published version of the manuscript.
A.P.: Contextualization, Validation, Data collection and curation.
N.D.S: Material and Data collections.
M.-Q.L.: Writing – Original draft, Data Analyses, Methodology.
P.-J.C.: Software, Editing/writing, Resources and conceptualization, Scientific support.
G.R., J.-F.C. and J.-F.M.: Visualization and Reviewing.
U.S.K. and F.B.: Reviewing, Advice, and Language help
Funding
This work is mainly supported by the scientific team of LGEF laboratory.
Acknowledgments
The authors would like to thank the ANR (French National Research Agency, number ANR-22-CE09-0032-04, IMINEN project) for having partially financed the research.
Conflicts of Interest: The authors declare no conflicts of interest.
References
- Zirafa CC, Romano G, Key TH, Davini F, Melfi F (2019) The Evolution of Robotic Thoracic Surgery. Ann Cardiothorac Surg 8: 210-217.
- Bodner J, Wykypiel H, Wetscher G, Schmid T (2004) First Experiences with the Da VinciTM Operating Robot in Thoracic Surgery. Eur J Cardiothorac Surg 25: 844-851.
- Kaposi A, Nagy A, Gomori G, Kocsis D (2024) Analysis of Healthcare Waste and Factors Affecting the Amount of Hazardous Healthcare Waste in a University Hospital. J Mater Cycles Waste Manag 26: 11691180.
- Egberts JH, Möller T, Becker T (2019) Robotic-Assisted Sleeve Lobectomy Using the Four-Arm Technique in the DaVinci Si® and Xi® Systems. Thorac Cardiovasc Surg 67: 603-605.
- Yang Y, Song L, Huang J, Cheng X, Luo Q (2021) A uniportal right upper lobectomy by three-arm robotic-assisted thoracoscopic surgery using the da Vinci (Xi) Surgical System in the treatment of early-stage lung cancer. Transl Lung Cancer Res 10: 1571-1575.
- Novellis P, Bottoni E, Voulaz E, Cariboni U, Testori A, et al. (2018) Robotic surgery, video-assisted thoracic surgery, and open surgery for early stage lung cancer: comparison of costs and outcomes at a single institute. J Thorac Dis 10: 790-798.
- Kumar A, Asaf BB (2015) Robotic Thoracic Surgery: The State of the Art. J Minim Access Surg 11: 60-67.
- Guo F, Ma D, Li S (2019) Compare the prognosis of Da Vinci robotassisted thoracic surgery (RATS) with video-assisted thoracic surgery (VATS) for non-small cell lung cancer: A Meta-analysis. Medicine (Baltimore) 98: e17089.
- Prasad PA, Joshi D, Lighter J, Agins J, Allen R, et al. (2022) Environmental Footprint of Regular and Intensive Inpatient Care in a Large US Hospital. Int J Life Cycle Assess 27: 38-49.
- Gaetani M, Uleryk E, Halgren C, Maratta C (2024) The Carbon Footprint of Critical Care: A Systematic Review. Intensive Care Med 50: 731-745.
- McGain F, Burnham JP, Lau R, Aye L, Kollef MH, et al. (2018) The Carbon Footprint of Treating Patients with Septic Shock in the Intensive Care Unit. Crit Care Resusc 20: 304-312.
- Tomson C (2015) Reducing the Carbon Footprint of Hospital-Based Care. Future Hosp J 2: 57-62.
- Pichler PP, Jaccard IS, Weisz U, Weisz H (2019) International Comparison of Health Care Carbon Footprints. Environ Res Lett 14: 064004.
- Watts N, Amann M, Ayeb-Karlsson S, Belesova K, Bouley T, et al. (2018) The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet 391: 581-630.
- Eckelman MJ, Sherman J (2016) Environmental Impacts of the U.S. Health Care System and Effects on Public Health. PLoS One 11: e0157014.
- McGain F, Sheridan N, Wickramarachchi K, Yates S, Chan B, et al. (2021) Carbon Footprint of General, Regional, and Combined Anesthesia for Total Knee Replacements. Anesthesiology 135: 976991.
- Thiel CL, Eckelman M, Guido R, Huddleston M, Landis AE, et al. (2015) Environmental Impacts of Surgical Procedures: Life Cycle Assessment of Hysterectomy in the United States. Environ Sci Technol 49: 1779-1786.
- Dettenkofer M, Kümmerer K, Schuster A, Mühlich M, Scherrer M, et al. (1997) Environmental auditing in hospitals: approach and implementation in an university hospital. J Hosp Infect 36: 17-22.
- Ashby MF (2013) Materials and the Environment. Eco-informed Material Choice, 2nd Edition.; Butterworth Heinemann, Oxford.
- Trecourt A, Cottinet PJ, Donzel M, Favretto M, Bancel B, et al. (2023) Carbon Footprint Evaluation of Routine Anatomic Pathology Practices Using Eco-Audit: Current Status and Mitigation Strategies. Ann Diagn Pathol 67: 152210.
- Pioche M, Neves JAC, Pohl H, Lê MQ, Grau R, et al. (2024) The Environmental Impact of Small-Bowel Capsule Endoscopy. Endoscopy 56: 737-746.
- Moninot I, Fontana A, Feurer E, Le MQ, Cottinet PJ, et al. (2024) Ab1331 the Carbon Footprint of Adalimumab Biosimilars Through Their Life Cycle. Annals of the Rheumatic Diseases 83: 2015-2016.
- Ditac G, Cottinet PJ, Quyen Le M, Grinberg D, Duchateau J, et al. (2022) Carbon Footprint of Atrial Fibrillation Catheter Ablation. Europace 25: 331-340.
- Grinberg D, Buzzi R, Pozzi M, Schweizer R, Capsal JF, et al. (2021) Eco-audit of conventional heart surgery procedures. Eur J Cardiothorac Surg 60: 1325-1331.
- McGinnis S, Johnson-Privitera C, Nunziato JD, Wohlford S (2021) Environmental Life Cycle Assessment in Medical Practice: A User’s Guide. Obstet Gynecol Surv 76: 417-428.
- Ansys Granta: Materials Information Management.
- Sartori I, Hestnes AG (2007) Energy Use in the Life Cycle of Conventional and Low-Energy Buildings: A Review Article. Energy and Buildings 39: 249-257.
- García-Sanz-Calcedo J (2014) Analysis on energy efficiency in healthcare buildings. J Healthc Eng 5: 361-373.
- Villani JD, Steiner L Energy Efficiency Opportunities in the OR.
- González González A, García-Sanz-Calcedo J, Rodríguez Salgado D (2018) Evaluation of Energy Consumption in German Hospitals: Benchmarking in the Public Sector. Energies 11: 2279.
- Da Vinci Surgery | Thoracic Robotic Assisted Surgery.
- Azizian M, Liu M, Khalaji I, DiMaio S (2018) The Da Vinci Surgical System. In: The Encyclopedia of Medical Robotics; World Scientific, pp. 3-28.
- (2015) Stainless Surgical Instruments.
- Vaughan A (2009) Environmental Legislation in the EU – What Medical Device Manufacturers Need to Know.
- Car Labelling Ademe: Comparateur des véhicules neufs (énergie, CO2, polluants ...).
- ltd, R. and M. Global Surgical Robotics Market 2021-2031: Focus on Vendor Analysis, Key Enabling Technologies, Emerging Platforms in Pipeline, 26 Company Profiles, and 45 Countries Data & Cross Segmentation.
- Intuitive Surgical, Inc. - AnnualReports.Com.
- Harrell CR, Djonov V, Fellabaum C, Volarevic V (2018) Risks of Using Sterilization by Gamma Radiation: The Other Side of the Coin. Int J Med Sci 15: 274-279.
- Peterson HB (2008) Sterilization. Obstet Gynecol 111: 189-203.
- Massey LK (2004) The Effect of Sterilization Methods on Plastics and Elastomers.
- Rizan C, Lillywhite R, Reed M, Bhutta MF (2022) Minimising Carbon and Financial Costs of Steam Sterilisation and Packaging of Reusable Surgical Instruments. Br J Surg 109: 200-210.
- McGain F, Story D, Lim T, McAlister S (2017) Financial and Environmental Costs of Reusable and Single-Use Anaesthetic Equipment. Br J Anaesth 118: 862-869.
- Leiden A, Cerdas F, Noriega D, Beyerlein J, Herrmann C (2020) Life cycle assessment of a disposable and a reusable surgery instrument set for spinal fusion surgeries. Resources, Conservation and Recycling 156: 104704.
- Bhopal A, Norheim OF (2021) Priority setting and net zero healthcare: how much health can a tonne of carbon buy? BMJ 375: e067199.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.