Echoes of Gulf War Illness: A Case Study of Chronic Symptoms from Toxic Exposure in East Palestine, Ohio
by Alexander Lishuen Chen1,2, Jun Hee Han2,3, Beatrice Alexandra Golomb2*
1University of Southern California, USA
2University of California, San Diego, USA
3California State University, Fullerton, California, USA
*Corresponding author: Beatrice Alexandra Golomb, Professor of Medicine, UC San Diego School of Medicine, 9500 Gilman Dr. #0995, La Jolla, California, USA
Received Date: 28 November 2024
Accepted Date: 02 December 2024
Published Date: 04 December 2024
Citation: Chen AL, Han JH, Golomb BA (2024) Echoes of Gulf War Illness: A Case Study of Chronic Symptoms from Toxic Exposure in East Palestine, Ohio. Ann Case Report. 9: 2100. https://doi.org/10.29011/2574-7754.102100
Abstract
Mixed toxic chemical exposures are a common problem, but challenging because different chemical mixtures for each may forestall progress of relevant science. Here, we evaluate a woman exposed to multiple toxic chemicals following the February 2023 East Palestine, Ohio train derailment and toxicant release/burn, to evaluate for concordance of ensuing health problems with diagnostic criteria for Gulf War illness (GWI) – i.e. for chronic multisymptom illness following a wholly distinct mixed toxic exposure. This woman in her 30s fully met criteria for all six “Kansas criteria” symptom domains required for diagnosing mixed toxicant illness in Gulf War veterans: fatigue/sleep, neurological/cognitive/mood, pain, respiratory, gastrointestinal, and dermatologic. (Kansas symptom criteria require qualifying symptoms, of at least moderate severity and/or multiple, in at least three domains; she met criteria for all six.) She additionally had a highly distinctive problem new post-derailment breakage and loss of teeth (culminating in removal of all teeth within the year) that was previously reported by a number of Gulf War veterans. We propose that since most chemicals’ toxicity includes mitochondrial mechanisms (severity of which relates to GWI severity), this toxic mechanism may add/synergize across chemicals for many chemical mixes, producing a shared chronic health profile. Conformity of persistent health problems in this woman to the signature illness affecting Gulf War veterans suggests that knowledge from one mixed chemical exposure may be ported to others, allowing science to advance – and enabling prophylaxis and treatment measures to be developed.
Keywords: Mixed chemical exposure; East Palestine, Ohio; Gulf War illness; Chronic multisymptom illness.
Abbreviations: EP: East Palestine, Ohio; GWI: Gulf War illness; MTE: mixed toxicant exposure; OSA: obstructive sleep apnea.
Introduction
Mixed toxicant exposures (MTEs) have historically posed problems, engendering chronic health problems in settings ranging from the Gulf War to the World Trade Center, now to the residents of East Palestine, Ohio (EP) who experienced a mixed toxic chemical release following the February 3, 2023 train derailment and toxicant release, followed by the February 6, 2023 “controlled-burn.” Each event involved a different mix of chemicals, so that those exposed are left without lessons from prior events. However, in the Gulf War, it was found that a similar health complex arose despite differing chemical mixtures experienced by different servicepersons. The finding that illness severity was tied to mitochondrial impairment [1] provides a rationale for why lessons from one event might have relevance to other events since mitochondrial toxicity transcends specifics of the chemical, and provides a mechanism that can add and synergize across mixed chemicals, leading to prospects for impacts that may be applicable for MTE events with distinct chemical composition perhaps particularly when individual component chemicals are thought to be within safe limits. Here we present a case of a young woman exposed following the EP derailment, to show that her symptom profile appears to accord with the profile previously reported for Gulf War illness following that very different chemical mixture. If similar health challenges arise following distinct MTE, this could provide prospects for lessons from one event to accelerate understanding and help for others.
Case Presentation
X, a 36-year-old female who resided ~0.5 miles from the derailment, was in her usual state of health (with a history of rhabdomyolysis) on no medications at time of the February 3, 2023 train derailment and toxicant release in EP. She welcomed a case report describing her experience. Among toxicants reportedly released/produced in the derailment/controlled-burn were vinyl chloride, phosgene, benzene, and butyl acrylate [2]. She developed a range of new symptoms and conditions in the ensuing days and weeks. X remained in EP for two months following the derailment, relocating in April 2023 due to health problems she attributed to the exposure.
When assessed 1.5 years after the derailment, she continued to manifest an array of symptoms that were evaluated according to the symptoms and symptom domains of the Kansas criteria for Gulf War illness (GWI), the persistent symptoms that classically followed a prior mixed toxicant exposure setting [3]. Regarding the sleep/fatigue domain, she cited alternating sleep disturbances, characterized by periods of insomnia and hypersomnolence. Even during phases of extended sleep, she reported persistent fatigue, with unrefreshing sleep. Regarding neurological/cognitive/mood symptoms, in addition to current (post-derailment) problems with memory and concentration, she reported developing (postderailment) material retrograde memory loss spanning from the time of derailment back to approximately 2020. She reported leg and generalized muscle weakness. She initially experienced severe headaches, which largely resolved following her move from EP. Regarding the Kansas pain domain, she noted persistent muscle pain in her left leg (the Kansas pain domain focuses on muscle/body pain). Regarding the respiratory domain, she reported shortness of breath on ascending a flight of stairs (also noting an irregular heart rhythm, with a heart rate rising up to 150 beats per minute when climbing stairs). Cited gastrointestinal symptoms include severe diarrhea as well as midline epigastric pain. Skin domain symptoms encompassed an acneiform eruption on her face that was not present pre-derailment, but (like the other symptoms noted) had persisted to the time of assessment. She also developed severe pervasive tooth decay, manifesting as tooth softening and breakage, culminating in extraction of all teeth, necessitating dentures in this woman without pre-derailment dental problems. Each time she returned to the area, she experienced sudden recurrence of headaches, shortness of breath, and nausea. Regarding laboratory tests, there was mild microcytic anemia, potentially consistent with her status as a menstruating female: hemoglobin 10.4 g/dL (11.7-15.5 g/dL), hematocrit 34.9% (35.0-45.0%), MCV 74.9 fL (80.0-100.0 fL), RDW 19.3% (11.0-15.0%). hsCRP was normal. A post-derailment EKG showed Long QT Syndrome.
Results
A past MTE setting, the 1990-1991 Persian Gulf War theater, led to multiple chronic symptoms in a subset of those exposed, i.e. GWI which has been quantitatively tied to mitochondrial impairment [1]. Most toxicants released in EP also produce mitochondrial toxicity [4], and such mechanisms are expected to be especially important in settings of MTEs. Mitochondrial and associated oxidative toxicity may add across exposures, even if toxicants are individually within safe limits. Because of these factors, we evaluated whether X’s symptoms met proxy “Kansas criteria” for GWI – criteria that are the most specific, and are recommended by the US National Academy of Medicine (then the Institute of Medicine) [5]. Under the proposed mitochondrial mechanism, individuals with conditions tied to less favourable pre-existing cell energy might show elevated vulnerability. X’s situation conforms to this: Her prior rhabdomyolysis (2016) and presence of reported lactic acidosis (and the addition of anemia, which, though mild, could compound cell energy shortfall by impeding oxygen delivery) may augment the prospect for mitochondrial compromise, if produced, to surpass the clinical threshold for symptom induction.
Table 1 demonstrates concordance of X’s symptoms with the Kansas symptom domains used for diagnosing GWI. It includes a column for new medications (post-derailment) added by her providers to alleviate associated symptoms. We include selfratings (scaled 0-10) for each domain-relevant symptom at its peak severity and current status. (Those criteria also require the exposure setting in that case, deployment to the Gulf theater at any time between the dates of August 1, 1990 and July 31, 1991, inclusive.) Obviously, there is a different exposure setting and timeframe for the EP event. For GWI, symptoms which have led to chronic illness (affecting an estimated third of those deployed) remain present in most affected veterans more than 30 years postexposure. While not part of Kansas criteria for GWI, similar descriptions of dental deterioration were documented in public comment sessions by multiple Gulf War veterans in the years following the Gulf War.
The finding that EP post-derailment symptoms can match GWI symptoms is important because it demonstrates that shared consequences may follow on MTE incidents that involve widely disparate toxicants. For GWI, many objective markers have been shown to be altered, including the aforementioned mitochondrial impairment, as well as expected consequences of said impairment: inflammation (tied to mitochondrial apoptosis [1], but mostly within normal limits, and with elevations inversely tied to GWI severity [1]); elevated autoantibodies [6,7], evidence of gray and white matter injury on brain imaging, autonomic impairment, immune impairment including depressed natural killer cells, and others. These markers may merit evaluation in EP toxicant-affected individuals. Figure 1 contains a proposed pathway for how MTEs cause health complications through mitochondrial mechanisms.
|
Kansas GWI Domain |
Example Qualifying Symptoms in EP toxicantaffected person |
Domain Qualifies? |
Symptom Rating at Worst |
Symptom Rating Currently‡ |
Current ‡ Medications |
|
Fatigue/sleep |
Severe fatigue, non-restful sleep, alternating insomnia and hypersomnolence |
√ |
6 |
6 |
Prazosin† and occasional hydroxyzine |
|
Neurological/ cognitive /mood |
Severe headache, muscle weakness, cognitive/ memory problems, severe irritability and short fuse, mood fluctuations, anxiety and depressed mood |
√ |
8 |
7 |
Risperidone and Lamictal |
|
Pain |
Muscle pain |
√ |
5 |
5 |
None |
|
Respiratory |
Shortness of breath causing her to present for medical care |
√ |
4 |
4 |
None |
|
GI |
Severe diarrhea, abdominal pain, weight loss |
√ |
7 |
4 |
Omeprazole |
|
Skin |
Rash on face, rash on perineum, thin skin, brittle hair and nails |
√ |
9 |
6 |
None |
|
*Proxy Kansas criteria 3, see text †Alpha-blocker used for nightmares and sleep disorders in PTSD ‡At time of assessment |
|||||
Table 1: GWI-relevant symptoms, by domain, in EP-exposed case.
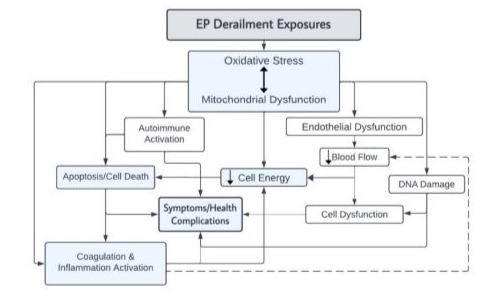
Figure 1: Pathway diagram illustrating the proposed mechanism by which MTE, including in EP, leads to the onset of symptoms’ Adapted from Golomb et al (2014), ©2014 Massachusetts Institute of Technology. All rights reserved.
Discussion
Increased rates of comorbid conditions (each also tied to mitochondrial impairment) have been reported in veterans with GWI, manifesting as hypertension, cardiovascular disease, sleep apnea, and, particularly in the earlier years, neurodegenerative disorders. Surveillance for these conditions should occur in those exposed following the EP derailment. X has not been evaluated for obstructive sleep apnea (OSA), but unrestful sleep with periods of hypersomnolence, and fatigue that may be worse following sleep, suggests OSA should be assessed. OSA, if present, is one potential post-derailment contributor to Long QT Syndrome [8]. Postderailment heavy metals and solvents have also been tied to Long QT. Muscle weakness, which can affect the upper airway dilator muscles, can compound any underlying energetic impairment. In Gulf War veterans, treating pulmonary sleep disorders – more common in GWI as in others with muscle weakness – significantly reduced many symptoms [9].
Factors favouring a causal relation of derailment-associated chemicals to this individual’s new symptoms and conditions include the ~rapid onset of multiple symptoms following the derailment, modest symptom mitigation after leaving EP, and recurrence or worsening of multiple symptoms upon return to EP, as well as concordance of her GWI-like symptom profile with that of another MTE exposed both in EP and following the Gulf War. (X also reported symptom exacerbation after encountering someone who has been in EP.) Not everyone is equally affected, as is true with any chemical exposure; X’s proximity to the derailment as well as prior history of rhabdomyolysis, with its tie to cell energy impairment [10], may also have influenced her symptom severity. The conformity of the symptom profile with GWI as further vital information compatible with a causal relationship: GWI, which is documented to relate to environmental exposures in individuals with notably variable multiple toxicant exposures in the Gulf theater, shows that this profile arises in a vulnerable subset following MTEs. Moreover, the tie between GWI severity and the severity of mitochondrial impairment provides a foundation for understanding the condition in the EP context, since most EP chemicals also produce toxicity through mitochondrial mechanisms. Dental breakage and loss were a reported Gulf War sequela that is also a match.
Conclusion
To conclude, literature showing that compatible symptoms followed a distinct MTE setting, the known presence of mitochondrial toxicity for multiple EP chemicals (together with GW agents), and documentation in GWI of a tie between symptom severity and degree of mitochondrial impairment, all support the likelihood that X’s symptoms are related to the EP derailment. This case is noteworthy because it points to a potential opportunity to adopt lessons learned from past MTEs for future toxicant and combusted (burned) toxicant events, underscoring the importance of learning from each event to draw lessons for future ones. Such lessons may enable better targeting of early testing, enhanced surveillance for health problems of potential interest, and possibly implementation of protective measures against some associated conditions, in a fashion that could offer prospects to reduce symptoms, suffering, morbidity, disability, and conceivably mortality following future MTE events.
Addendum
The individual died after this case report was written (with her full involvement), taking her life citing EP derailment issues and the concern she would be a burden to others. Beyond derailmentassociated health challenges, she had faced financial hardships leaving her home near “ground-zero,” with her home being foreclosed. She had faced anguishing personal decisions e.g. whether to abort a fetus given the chemical exposure that affected her health and might affect that of her unborn child. Some other details are perhaps relevant but withheld out of deference to the family. She had repeatedly made clear that she wanted her experience to be shared, in hopes of helping others. X was not just a “case” for this report but a person – who will be missed dearly by her family, friends, and her community.
Acknowledgements: We acknowledge the kind help of Jami Wallace, in communications with the family. This case report was part of an effort funded by NIEHS R21ES036163-02. The funding source had no role in the study design, data collection, data analysis, data interpretation, or the decision to submit the manuscript for publication.
Conflict of Interest: All authors declare they have no competing interests.
References
- Golomb BA, Sanchez Baez R, Schilling JM, Dhanani M, Fannon MJ, et al. (2023) Mitochondrial impairment but not peripheral inflammation predicts greater Gulf War illness severity. Sci Rep. 13:10739.
- Isaacs-Thomas B. (2023) What we know about the chemicals aboard the train that derailed in Ohio.
- Steele L. (2000) Prevalence and patterns of Gulf War illness in Kansas veterans: association of symptoms with characteristics of person, place, and time of military service. American Journal of Epidemiology. 152:992-1002.
- Miller ML, Radike MJ, Andringa A, Bingham E. (1982) Mitochondrial changes in hepatocytes of rats chronically exposed to vinyl chloride and ethanol. Environ Res. 29:272-9.
- Committee on the Development of a Consensus Case Definition for Chronic Multisymptom Illness in Gulf War Veterans, Board on the Health of Select Populations, Institute of Medicine. Chronic Multisymptom Illness in Gulf War Veterans: Case Definitions Reexamined. Washington (DC): National Academies Press (US) Copyright 2014 by the National Academy of Sciences. All rights reserved.; 2014.
- Vojdani A, Thrasher JD. (2004) Cellular and humoral immune abnormalities in Gulf War veterans. Environ Health Perspect. 112:8406.
- Abou-Donia MB, Conboy LA, Kokkotou E, Jacobson E, Elmasry EM, et al. (2017) Screening for novel central nervous system biomarkers in veterans with Gulf War Illness. Neurotoxicol Teratol. 61:36-46.
- Patel SI, Zareba W, Wendel C, Perez K, Patel I, et al. (2023) A QTc risk score in patients with obstructive sleep apnea. Sleep Med. 103:15964.
- Amin MM, Gold MS, Broderick JE, Gold AR. (2010) The effect of nasal continuous positive airway pressure on the symptoms of Gulf War illness. Sleep Breath.
- Preger A, Wei R, Berg B, Golomb BA. (2023) COVID-19-associated rhabdomyolysis: A scoping review. International Journal of Infectious Diseases. 136:115-26.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.