Early-Age Orthodontic Treatment: An Approach with “Prefabricated Aligners” Combined with Myofunctional Therapy - Two Case Reports
by Andrea Freudenberg1, Daniel Fuchs1, Maximilian Bleilöb2, Christina Erbe2, Julia Camilla Bulski2*
1Private practice, Fachzentrum für Kieferorthopädie Dr. Andrea Freudenberg & Kollegen, Weinheim, Germany
2Department of Orthodontics, University Medical Center of the Johannes Gutenberg, University of Mainz, Augustusplatz 2, 55131 Mainz, Germany.
*Corresponding author: Contributed equally; Julia Camilla Bulski, Department of Orthodontics, University Medical Center of the Johannes Gutenberg, University of Mainz, Augustusplatz 2, 55131 Mainz, Germany.
Received Date: 24 March 2024
Accepted Date: 28 March 2024
Published Date: 01 April 2024
Citation: Freudenberg A, Fuchs D, Bleilöb M, Erbe C, Bulski JC (2024) Early-Age Orthodontic Treatment: An Approach with “Prefabricated Aligners” Combined with Myofunctional Therapy - Two Case Reports. Ann Case Report 9: 1727. https://doi.org/10.29011/2574-7754.101727
Abstract
Early-childhood orthodontic treatment should be preventive, sustainable, and cost-efficient. Two cases treated with mykie®, an early-age orthodontic approach in combination with myofunctional therapy, will be presented. The use of eruption guidance appliances (EGAs) as “prefabricated aligners” is integrated in this interdisciplinary concept. Advantages and limitations of this approach will be discussed and the possibility of combining EGAs with other appliances, e.g. aligners, will be discussed.
Keywords: Aligner; Early-Age Orthodontic Treatment; Economic Evaluation; Eruption Guidance Appliances; Growing Patients; Myofunctional Therapy
Introduction
Early-childhood orthodontic treatment is very controversially discussed in literature. Opponents criticize frequently observed instability, often failing to avoid a second orthodontic treatment and thus resulting in extended treatment durations as well as a total cost increase [1]. Therefore, many practitioners favor a later start, when patients reach adolescence, to correct the dental and skeletal malposition and primarily base their therapy on functional and/or fixed orthodontic appliances or clear aligners. The results, likewise, are often not stable [2], but longer lasting due to better intercuspation of the permanent teeth as well as life-long retainers regularly applied at the end of the treatment.
But why is orthodontic treatment often not stable? What are the reasons for relapse? What are the causes for malocclusion? According to Schopf [3], only 25% of all malocclusions seen in day-to-day practice derive from genetic predispositions, implying that the majority of roughly 75% arise from functional imbalances of the orofacial system [4]. These include, among others, a low resting position of the tongue and mouth breathing [5-7].
Form follows function (and vice versa) in the growth of the maxillofacial complex [8]. The jaw bones - and consequently the teeth - develop in the direction they are guided towards by the pressure and traction of the muscles and surrounding tissues. Therefore, the teeth (or the malocclusion) reflect the prevalent orofacial function or dysfunction.
Thus, successful treatment of malpositions and prevention of relapses requires a combination of the orthodontic treatment with myofunctional therapy, especially in early-age orthodontics.
Correcting orofacial dysfunction early, allows the jaws and teeth to grow into their physiological position, instead of having to compensate the malposition when they have already been manifested. This topic is controversially debated in recent literature and online: Some studies and trials support the effectiveness of an early approach interceptive orthodontic treatment. This treatment approach is not a novelty since functional appliances such as the Bionator by Balters and the Frankel Functional Regulator by Fränkel have been used successfully for decades in countries all over the world [9, 10]. The comprehensive concept of all these functional appliances is the guidance of the teeth into their optimal position by manipulation or training of the orofacial soft tissues. By retaining the tongue, lips and/or cheek muscles, the appliances allow the teeth to develop into the intended direction.
There exist multiple other approaches on how to treat 6- to 10-year-old patients. The concept of orthotropics, created by Mew in the 1970’s, for instance, focusses not primarily on correcting every single malpositioned tooth, but rather on promoting facial growth [11].
During the last decades, many companies worldwide have developed prefabricated appliances made of silicone (eruption guidance appliances = EGA). The mutual aim of all these appliances is to positively influence the orofacial tissues, establish nose breathing and high tongue posture and to guide erupting teeth into the desired direction. To support the effectiveness of their appliances, companies like Myofunctional Research Co. (MRC, Helensvale, Australia), LM-dentalTM (LM-Instruments Oy, Parainen, Finland) and Orthoplus® (Igny, France) have invented treatment approaches which combine these appliances with a standardized training schedule to exercise the orofacial tissues in the sense of a rudimentary myofunctional therapy.
Since, for the author team, none of the above-mentioned treatment options seemed satisfying enough in synergizing contemporary, viable orthodontics with holistic myofunctional training, Dr. Freudenberg and her team developed their own treatment concept mykie® (= myofunktionelle Kieferorthopädie, German for myofunctional orthodontics). The objectives were the following:
- to develop an efficient interdisciplinary early age treatment with reduced relapse tendency
- to select appliances from available sources solely based on their performance and remain independent from specific suppliers/companies
- to create a treatment approach that is feasible for children in contemporary society
- to be focused on the total cost of a child’s treatment as sometimes a second phase of treatment is necessary that also needs to be financed.
Materials and Methods
Additional information to the case-presentation and the treatment concept mykie®
The concept mykie® has been invented to reach the four objectives mentioned above. Ideally, prevention should start directly after birth of a child in form of parental education. In our experience, active treatment with sufficient compliance can start as soon as the child reaches primary school age – sometimes earlier, depending on the child’s maturity and ability to learn and comply. Our treatment plan is spread over 1.5 years, including monthly visits to the orthodontic office. Every appointment comprises two steps: the adjustment of the appliances as well as an assessment of progress by the orthodontist, followed by myofunctional training performed by a specialized myofunctional therapist. Patients are instructed to wear trainers (EGAs) one hour per day and all night. In most cases, transversal and sagittal expansion of the upper jaw is necessary. Those patients have to wear an additional removable appliance 24 hours a day, only taken out for oral hygiene, for about 6 months (Figure 1). All patients are further instructed to perform selected myofunctional exercises for 10 minutes daily.

Figure 1: Bioplate appliance modified from Bioblock (orthotropics).
Good compliance and motivation are indispensable, making education and motivation, first of the parents and then the patient, a major part of the mykie®-therapy concept. After every treatment phase of 6 months, the patient and the parents receive verbal feedback and are shown photographs of the patient’s teeth and facial development status to provide both, the patient and the parents, with information of their joint achievements.
After active treatment of 1.5 years, we offer an one-year sustainability phase comprising 5 appointments, again with both, the orthodontist and the myofunctional therapist, present during the appointments. Afterwards, the patient is instructed to wear the EGA only at night and is scheduled at least biannually to monitor the further dentition development as well as the new muscle balance’s stability.
EGAs / Myotrainers
Eruption guidance appliances (“EGAs” or more commonly referred to as “Trainer” or “Myotrainer”, Figure 2) are not very popular among orthodontists who often criticize the lack of patients’ compliance as well as the fact that they are not made-to-measure for the individual patient. Furthermore, many practitioners might be discouraged by the wide variety of prefabricated appliances available as there are multiple different companies offering a large number of different appliances in varying sizes and for different malpositions.
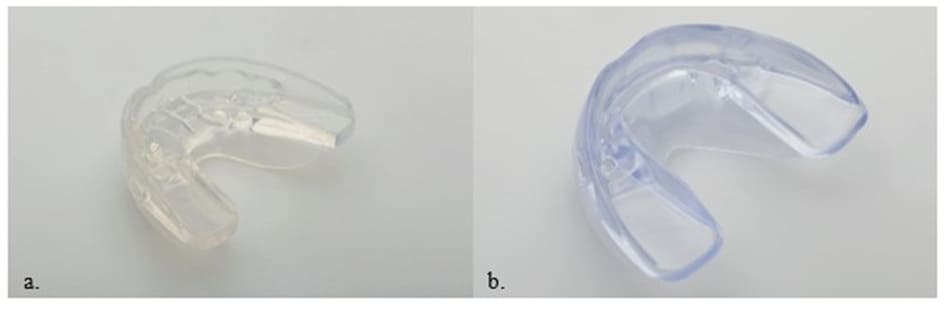
Figure 2: a. LM-ActivatorTM 2, b. orthoplus® EFT slim
Despite the downsides arising from the use of EGAs, many benefits can be discovered: The first to be named is the undeniable cost benefit, in comparison to individually produced appliances, which plays an important role because early treatment is often fully or partially self-paid by parents in Germany. While the function as a guard against the pressure of the cheek and the tongue is undeniable, trainers prevent mouth breathing and direct the breathing current automatically to the nose (all other functional appliances do not provide a big labial shield).
Additionally, their function as an orthodontic appliance is surprisingly beneficial and has been shown by Keski-Nisula [12]. In 5-year-old children statistically significant improvements in terms of molar relationship, overjet, overbite, incisor alignment and mandibular growth enhancement can be achieved after three years of treatment compared to a control group, even without any additional myofunctional training and exclusive nighttime ware [13]. Furthermore, these results proved to be stable 11 years posttreatment [13]. In growing patients, teeth (and jaws) are guided by very mild pressure into the space provided by the EGA which act like a set-up or the final aligner in a treatment plan. Thus, the choice of the correct EGA for the respective malocclusion is crucial to allow an effective treatment. Figure 3 shows the alignment that can be achieved with one EGA after 6 months only.
In compliance with the recommended wearing time, the information provided by the EGA is being translated into the position of the teeth. The bony structures are still malleable and respond very well to gentle pressure which is exerted for one hour a day and at night. Therefore, pre-treatment, it is important to know which amount of overjet and overbite is prescribed by the EGA used (Figure 4). The same applies to the transversal width. All these factors vary between manufacturers.
To use the suitable set-up for every single patient and reduce the number of EGAs stored in our office we did a survey, in which we evaluated the prescribed information of more than 100 individual EGAs from different companies by pouring plaster in the EGAs followed by relevant measurements. Out of more than 100 EGAs from different companies, we created our concept that includes about 10 EGAs, particularly from the companies Orthoplus® and LM-Activator®. This survey has been published [14-16].
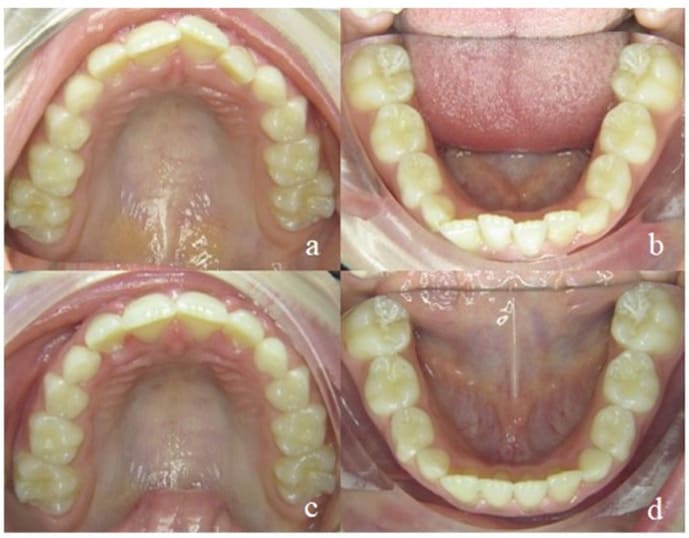
Figure 3: Alignment of the upper (a, c) and lower (b, d) jaw after 6 months of EGA-treatment.
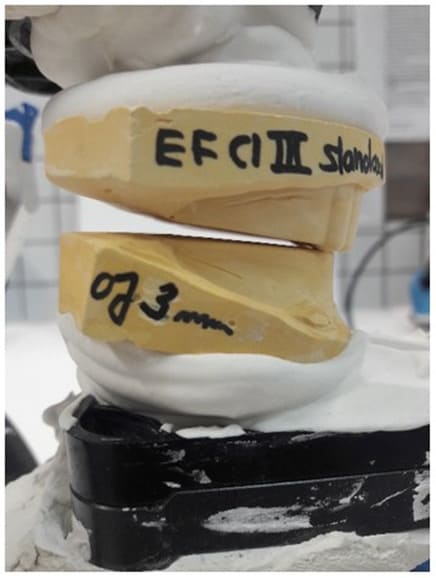
Figure 4: EGA from Orthoplus® EFT Classe 3 articulated.
Myofunctional Treatment
In our opinion, to benefit the most from EGAs, from the myofunctional point of view, it is necessary that myofunctional specialists carry out the treatment simultaneously to the patient wearing an EGA. Myofunctional treatment is a highly specialized part in the field of speech-therapy and, thus, cannot be carried out by dental assistants or orthodontists with the same high-quality standard. In addition, myofunctional therapy on prescription is covered by statutory health insurances in Germany, an important fact from the patient’s perspective as well.
Patient selection
Our office is divided into two separate areas, one reserved for general orthodontics and the other fully dedicated and specialized on early treatment. The latter has exclusively focused on treatments according to the mykie® concept for the past 6 years which we will continue to review and develop. Overall, more than 350 cases have already been treated, most of them very successfully. Since the cross-bite and the open bite are very common treatments and the deep-bite is quite a challenging one to treat without fixed appliances, the following two examples have been selected to demonstrate the effectiveness of the mykie® concept.
Case Report
Case 1 - Deep Bite
During her first appointment in our orthodontic office, this 8-year-old girl showed an age-appropriate mixed dentition, a bilateral mandibular retrognathism, an increased overjet of 7mm, an increased overbite of up to 80%, moderate crowding in the upper and mild crowding in the lower jaw. Myofunctional, an open mouth resting posture was observed (also described as lip incompetence) which led - in combination with the aforementioned increased overjet - to a resting position of the lower lip behind the maxillary incisors, favoring a large overjet. There were no speech impediments to be diagnosed but during swallowing, activation of the M. orbicularis oris and M. mentalis was observed. The lingual frenulum was short, her body posture normal (Figure 5). The defined orthodontic goals included the overjet and overbite reduction, mandibular advancement as well as elimination of crowding in both jaws. The myofunctional goals were the establishment of a habitual closed-lip position and nasal breathing to provide negative pressure in the oral cavity in order to ensure a physiological resting position of the tongue on the palate.
Orthodontic treatment was performed by using an EGA, chosen according to the occlusal factors and growth deficits of the jaws. Control intervals took place once a month. Directly following every orthodontic control, the patient received myofunctional therapy in the orthodontic office conducted by a specialized myofunctional therapist. After only six months, significant improvements, in both, the occlusal and myofunctional situation could be observed (Figure 6): the overjet was reduced to 3.5 mm, bringing the mandible forward by around ½ of a premolar width. In addition, there was an overbite reduction to 30%, while crowding in both jaws had almost completely been resolved. Due to the EGA and the lip closure exercises, the patient broke the habit of resting her lower lip behind her maxillary front teeth. Nasal breathing had been established in most situations except during physical exertion. The resting position of the tongue and its strength still needed further improvement.
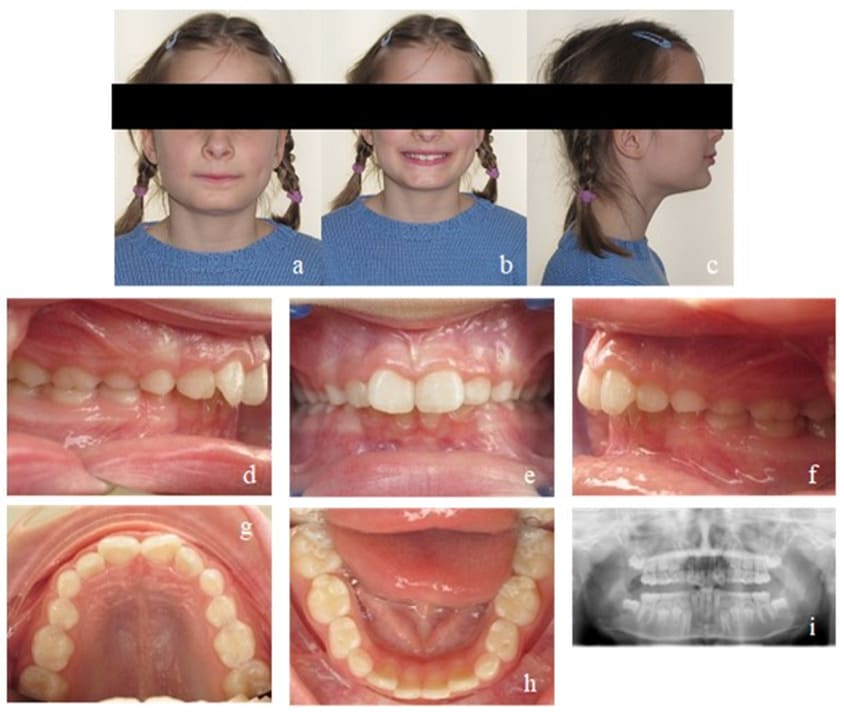
Figure 5: Case 1. Initial findings. En face (a, b) and profile of the patient (c). Frontal view of the occlusion (e), occlusion right (d) and left (f). Upper (g) and lower arch (h). Initial Panoramic x-ray (i).

Figure 6: Case 1. Interims findings after 6 months of treatment. Frontal view of the occlusion (b), occlusion right (a) and left (c). Upper (d) and lower arch (e).
During the next treatment phase (another six months), the patient continued wearing the appliance and performing selected exercises as advised. The dental situation continued to improve, showing a physiological overjet of 2 mm with occlusal contact of all incisors and no crowding. However, the torque of the maxillary front teeth had still to be corrected (Figure 7). The strength of the tongue and its resting position on the palate also improved.

Figure 7: Case 1. Second interims findings after 12 months of treatment. Frontal view of the occlusion (b), occlusion right (a) and left (c). Upper (d) and lower arch (e).
In the last phase (again six months) of the active treatment process, the Class II occlusion was fully corrected into a Class I relation on both sides. From the myofunctional perspective, the resting position of the tongue was stable in its physiological position. Closure of the lips could be accomplished without hypertension of the M. mentalis and the perioral muscles. Nasal breathing was established even during physical exertion. The active treatment time of 18 months was followed by a 12-months retention phase, during which orthodontic appointments in combination with myofunctional therapy took place every two months and a consolidation of the accomplishments was achieved.
During all treatment phases, the patient had been highly compliant and motivated. 18 months of active mykie®-treatment showed significant improvements on the dental as well as on the myofunctional side. To ensure a stable retention of what was achieved, the patient continued wearing an EGA on a nightly basis throughout the transitional phase of dentition until all second molars erupted and visited the orthodontic office biannually. No further orthodontic treatment was necessary (Figure 8). Finally, for perfect alignment, a short aligner treatment could be recommended (Figure 9).
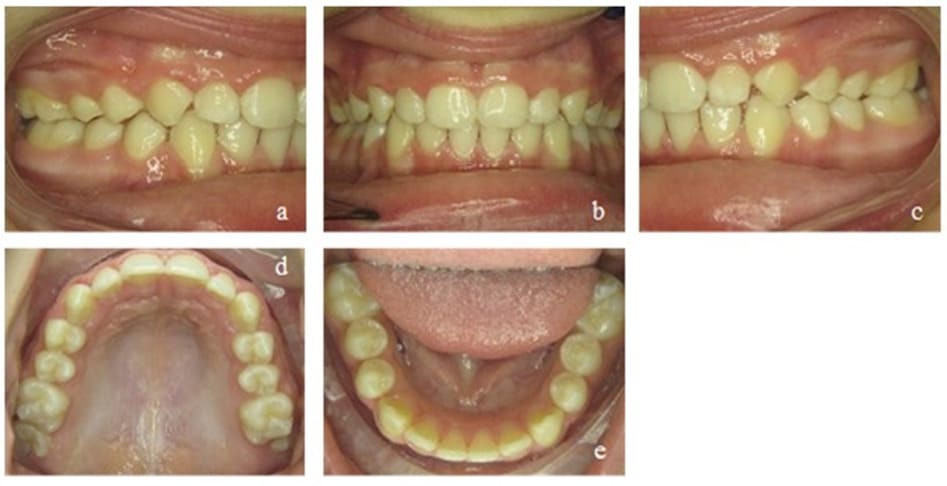
Figure 8: Case 1. Final findings. Frontal view of the occlusion (b), occlusion right (a) and left (c). Upper (d) and lower arch (e).
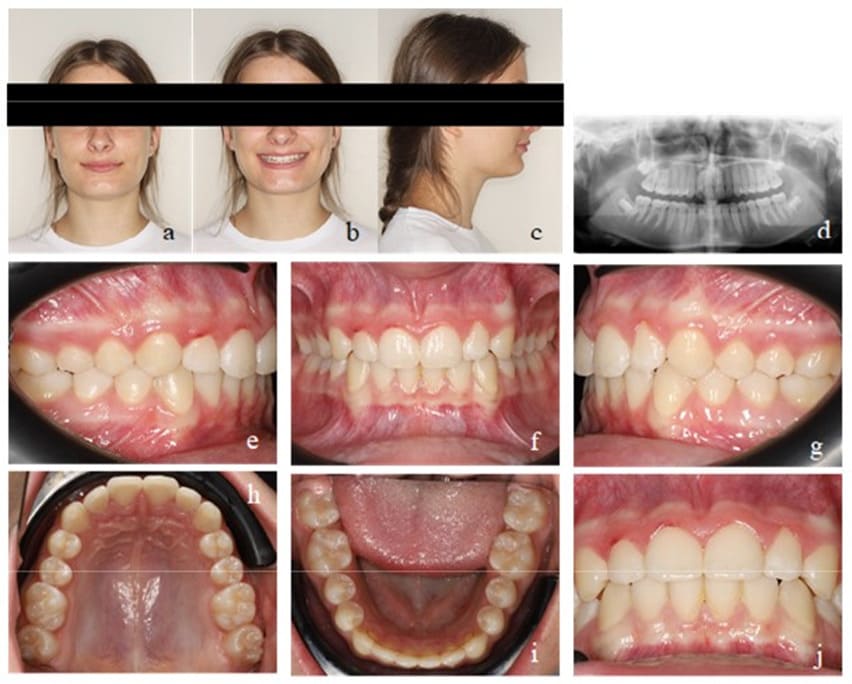
Figure 9: Case 1. Final findings after a short Invisalign® treatment. En face (a, b) and profile of the patient (c). Final Panoramic x-ray (d). Frontal view of the occlusion (f), occlusion right (e) and left (g). Upper (h) and lower arch (i). View of the final overjet and overbite (j).
Case 2 - Cross Bite/ Open Bite
This patient was transferred to our orthodontic office by her speech-therapist at the age of 6. During initial diagnosis, a unilateral posterior cross bite on the right side and an anterior open bite of 3 mm were apparent. Accordingly, the upper arch was too narrow and needed further transversal development. Mild crowding in the lower front segment and an exaggerated Wilson’s curve of the lower permanent and deciduous molars could be seen. The dental situation confirmed the myofunctional diagnosis of a habitual open mouth posture, infantile swallowing, a low resting position of the tongue and enlarged palatine tonsils. Nasal polyps had already been removed at an earlier stage (Figure 10).
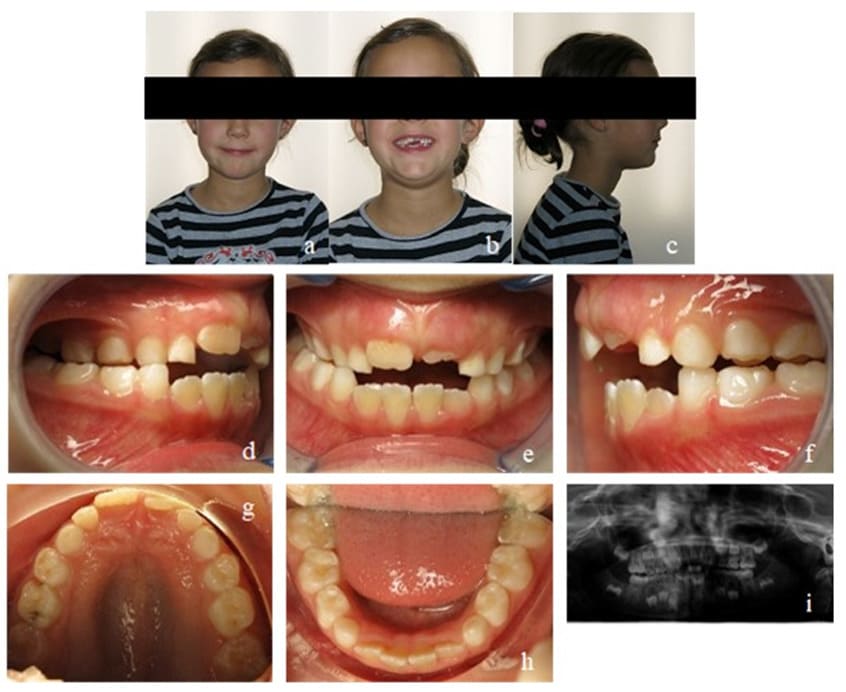
Figure 10: Case 2. Initial findings. En face (a, b) and profile of the patient (c). Frontal view of the occlusion (e), occlusion right (d) and left (f). Upper (g) and lower arch (h). Initial Panoramic x-ray (i).
Our initial orthodontic goal was the posterior cross bite elimination by maxillary expansion to create enough space for the tongue. The second goal was to straighten up the lower molars and to close the anterior open bite. Myofunctional goals comprised the establishment of nasal breathing, mature swallowing, and the physiological resting position of the tongue.
The most important task during the first treatment phase was to expand the maxilla. Due to their comparatively soft structure, parttime worn EGAs alone are not suitable to perform that expansion. Therefore, in addition to an appropriate EGA, the patient received a removable appliance named Bioplate (Figure 1) based on the Biobloc invented by Mew (orthotropics). It is worn for 24 hours per day and is only removed once a day for cleaning and daily activation. Maxillary incisor protrusion, maxillary expansion as well as a lateral bite block in combination with provision of improved space for the tongue on the anterior palate are the major advantage of this appliance. Additionally, the Bioplate is almost invisible, allows clear speaking, and can be worn in combination with an EGA to straighten up the lower molars, aligning the lower teeth, allow bite jumping and influence mouth breathing as well as tongue posture.
After the first treatment phase, the posterior cross bite was corrected and the anterior open bite reduced, but still remained present. The patient adapted the mature swallowing pattern rather quickly, but an interdental lisp remained and showed extensive tongue movement while wearing the EGA. The strength of the tongue was still low (Figure 11). The appliance of choice for the second phase was a Bionator instead of an EGA, because a Bionator allows speaking and can therefore be worn for more hours during the day. We controlled compliance with a Theramon® chip (MC Technology GmbH, Hargelsberg, Austria). The tongue movements calmed down and its strength increased while the open bite was further reduced to 1 mm. The maxillary transversal width was successfully retained. Mouth breathing could still be observed at times (Figure 12).

Figure 11: Case 2. Interims findings after 6 months of treatment. Frontal view of the occlusion (b), occlusion right (a) and left (c). Upper (d) and lower arch (e).
In the last active treatment phase as well as sustainable phase, the patient continued wearing an EGA. For the first time, we achieved a positive overbite, and the patient could fully establish a closed lip posture with nasal breathing. The tongue could be strengthened, and the resting position was stable in its physiological state. However, for a long time, there was still no contact of the upper and lower front teeth. This could be fully achieved 2 years later and stayed stable in the long term (Figure 13).

Figure 12: Case 2. Second Interims findings after 12 months of treatment. Frontal view of the occlusion (b), occlusion right (a) and left (c). Upper (d) and lower arch (e).

Figure 13: Case 2. Third interims findings after 18 months of treatment. Overjet and overbite (b), occlusion right (a) and left (c). Upper (d) and lower arch (e).
Up until the end of the treatment, the patient participated highly motivated, wearing the appliances, and performing the exercises as desired. The shaping of the dental arches could already be corrected during the first six months of treatment, solely the closing of the frontal open bite needed more time due to underlying myofunctional deficits. The patient is currently still wearing an EGA on a nightly basis until all permanent teeth will have fully erupted to ensure the dental and myofunctional retention (Figure 14, 15).
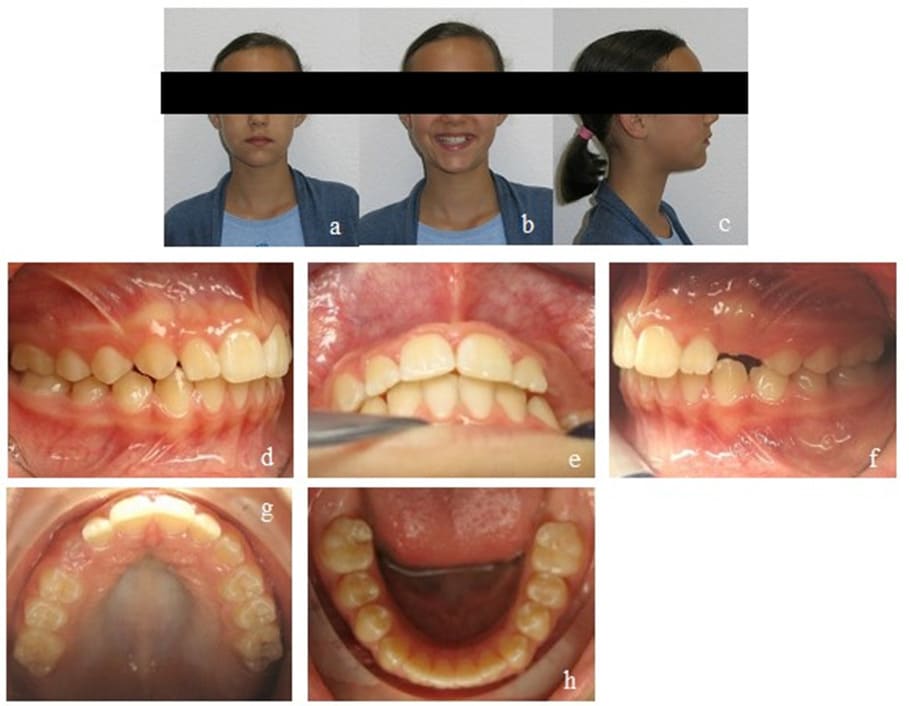
Figure 14: Case 2. Final findings. En face (a, b) and profile of the patient (c). Final overjet and overbite (e). Occlusion right (d) and left (f). Upper (g) and lower arch (h).

Figure 15: Case 2. Final findings after 2 years post-treatment. En face (a, b) and profile of the patient (c). Frontal view of the occlusion (e), occlusion right (d) and left (f). Upper (g) and lower arch (h). View of the final overjet and overbite (i).
Discussion
Both examples demonstrate the magnificent potential of a prefabricated Eruption Guidance Appliance (EGA) that was able to successfully correct most of the orthodontic issues concerning young and growing patients in a very short overall treatment time. However, it needs to be considered that these results depend a lot on good compliance and motivation - the key to success.
An early start of treatment is an essential aspect of successful therapy with EGAs: In our experience, treatment should commence around seven to eight years of age. At this age, children already understand the meaning of homework and compliance. Furthermore, the jawbones and teeth react to very light forces and the nocturnal sleep lasts mostly around 10 hours. In this way, the malocclusion and myofunctional deficits can be corrected before the prepubertal growth spurt starts, preventing the jaws (and face) to grow further into an unphysiological direction.
In most cases, a transversal deficit is present, and a maxillary expansion is required (case 2). When the tongue is not habitually positioned in its physiological resting position on the palate, the maxilla cannot develop properly. However, a too narrow maxilla, does not provide enough space for the tongue to take its natural position. According to Hotz [17] and Proffit [6], skeletal transversal growth happens most distinctly between eight and ten years. Thus, this age period is most effective for the mykie®-treatment. A lot of maxillary expansion, however, cannot be achieved by an EGA alone which is why an additional appliance, the Bioplate, is needed. Special EGAs, which can be worn above the Bioplate, direct the tongue to its physiological position and lead to a neuromuscular consolidation of this position, while maxillary expansion is happening. Once the required expansion is accomplished, the Bioplate can be worn on a nightly basis for a couple of months until the physiological resting position of the tongue is learned habitually. The placement of the tongue (which is favored by the EGA), the EGA itself and the occlusion will then retain the maxillary width (case 2).
Clear aligners like Invisalign®* First (Invisalign®, Align Technology, Santa Clara, CA, USA) represent an alternative for maxillary expansion. However, unlike clear aligners, the Bioplate is hardly removed, not even during meals, and therefore cannot be forgotten to be put back in. On the other hand, clear aligners leave a free palate, making it much easier for the tongue to find its physiological place in the roof of the mouth.
Vertical malocclusions like deep bites and open bites can also be treated using EGAs and myofunctional therapy. As shown in Case 1 an EGA can correct deep bites by encouraging premolars and molars to extrude while performing intrusive forces on the incisors. Leveling the curve of Spee works excellent with EGAs – treatments which are more challenging with aligners. In return, specific open-bite-EGAs exert intrusive forces on premolars and molars while shielding the incisors against tongue thrust and lip biting, providing space for them to extrude which facilitates open bite closure. However, due to the fact that speaking is not possible, the EGAs wearing time is limited. For this reason, in our office, a Bionator is used in cases with extensive frontal tongue pressure (substantial open bites, Case 2).
An unilateral space opening, e.g. for permanent canines (due to early root resorption) is difficult to treat with EGAs exclusively. In these cases, a combination with aligners for example Invisalign® First (Invisalign®, Align Technology, Santa Clara, CA, USA) is advantageous. Most EGAs can easily be worn together with clear aligners so they can support the tooth movements as planned and the myofunctional balance to ensure a long-lasting retention. However, the overall costs must considered.
Interestingly, by establishing habitual nose breathing, many positive side-effects considering general health can often be observed [18]: Mouth-breathing children suffer disproportionally more often from allergies and/or already have a history of tonsillectomy and polyp removals. Opening the nasal airway allows the filter effect of the nose to work properly and warms up the inhaled air, protecting the lymphatic tissues. During treatment, the physiological resting position of the tongue is trained simultaneously to the correct posture of the whole body. Learning the erection of the spine in childhood may prevent back pain in adulthood [19].
Conventional early age orthodontic treatment has always been criticized for not being sustainable. Indeed, many cases relapse and need a second stage treatment in adolescent age. Relapse happens when the force of the surrounding muscles, predominantly the tongue, lips and cheeks, is not balanced. However, when an adequate myofunction, embedded in the orthodontic treatment, is learned and preserved in the long term, growth is directed into the right direction and later relapse is unlikely to happen.
The case studies presented in this article are two examples among many successfully treated children in our orthodontic office during the last 6 years. The mykie®-concept shows that an EGA cannot only guide erupting teeth, but rather can align the arches, correct a Class II malocclusion, level the curve of Spee and resolve an anterior deep bite while simultaneously encouraging a myofunctional correct environment - given sufficient compliance. Treatments with EGAs is much cheaper compared to individually fabricated appliances or clear aligners. Regarding the overall costs, this concept represents a very interesting approach, even if a second phase treatment is necessary as the latter is often just a simple case that can be successfully addressed with a small number of clear aligners, resulting in a healthy and esthetically perfect outcome.
Conclusion
Early-childhood orthodontics in combination with concurrent myofunctional therapy can provide an excellent way of helping young individuals to grow physiologically in an improved balance of their orofacial tissues surrounding the teeth. A reduced need for complex and challenging orthodontic treatments in adolescence or adulthood, sometimes even involving surgery, and more long-term stable results can be achieved. Thus, EGAs represent medically superb and cost-effective devices, especially when compared to other treatment options. However, some tooth movements cannot be carried out by EGAs alone (such as maxillary transversal expansion or unilateral space opening), making combinations with an additional removable plastic appliance or clear aligners useful in some cases. Here, special EGAs can be worn on top of clear aligners or other removable orthodontic appliances in order to support the desired tooth movements while establishing myofunctional balance to ensure long-lasting retention and fewer relapses.
For further information and more case studies, please check our website mykie.de (temporarily only available in German).
Disclosure
Author Contributions: Conceptualization, A.F., D.F. and J.C.B..; methodology, A.F. and D.F., investigation A.F. and D.F.; resources, A.F., D.F. and J.C.B.; data curation, A.F. and D.F.; writing— original draft preparation, D.F. and J.C.B.; writing—review and editing, D.F., M.B., C.E. and J.C.B.; supervision, A.F. and C.E.
Funding: This research received no external funding.
Informed Consent Statement: Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement: Data supporting the study results can be provided followed by request sent to the corresponding author’s e-mail.
Conflicts of Interest: None.
References
- Sunnak R, Johal A, Fleming PS (2015) Is orthodontics prior to 11 years of age evidence-based? A systematic review and meta-analysis. J Dent 43(5): 477-486.
- Little RM, Riedel RA, Artun J (1988) An evaluation of changes in mandibular anterior alignment from 10 to 20 years postretention. Am J Orthod Dentofacial Orthop 93(5): 423-428.
- Schopf P (1981) Der Anteil exogener Faktoren an der Entstehung von Dysgnathien. Fortschritte der Kieferorthopädie 42(1): 19-28.
- Moss ML, Salentijn L (1969) The primary role of functional matrices in facial growth. Am J Orthod 55(6): 566-577.
- Proffit WR (1978) Equilibrium theory revisited: factors influencing position of the teeth. Angle Orthod 48(3): 175-186.
- Proffit WR (1986) On the aetiology of malocclusion. The Northcroft lecture, 1985 presented to the British Society for the Study of Orthodontics, Oxford, April 18, 1985. Br J Orthod 13(1): 1-11.
- Proffit WR, Fields H, Larson B, Sarver D (2018) Contemporary Orthodontics, vol. 6th Edition: Mosby.
- Kieferorthopädie und Funktion. https://www.zm-online.de/ artikel/2019/2019-01-02-nachhaltige-versorgung-sieht-andersaus-01-02-2019-nachhaltige-versorgung-sieht-anders-aus/ kieferorthopaedie-und-funktion
- Balters W (1960) Ergebnis der gesteuerten Selbstheilung von kieferorthopädischen Anomalien. DZZ 15: 241-248.
- Fränkel R, Fränkel C (1992) Der Funktionsregler in der orofazialen Orthopädie: Karl F. Haug Fachbuchverlag.
- Mew J The Cause and Cure of Malocclusions; 1981.
- Keski-Nisula K, Hernesniemi R, Heiskanen M, Keski-Nisula L, Varrela J (2008) Orthodontic intervention in the early mixed dentition: a prospective, controlled study on the effects of the eruption guidance appliance. Am J Orthod Dentofacial Orthop 133(2): 254-260; quiz 328 e252.
- Keski-Nisula K, Keski-Nisula L, Varrela J (2020) Class II treatment in early mixed dentition with the eruption guidance appliance: effects and long-term stability. Eur J Orthod 42(2): 151-156.
- Freudenberg A, Fuchs D, Rhein S, Adam C, Pumm Jn (2020) Konfektionierte Silikontrainingsgeräte für eine kombiniertmyofunktionell-kieferorthopädische Frühbehandlung - Teil 1 Ortho Orofacial 1.
- Freudenberg A, Fuchs D, Rhein S, Adam C, Pumm J (2020) Konfektionierte Silikontrainingsgeräte für eine kombiniertmyofunktionell-kieferorthopädische Frühbehandlung - Teil 2 Ortho Orofacial 2.
- Freudenberg A, Fuchs D, Rhein S, Adam C, Pumm J (2020) Konfektionierte Silikontrainingsgeräte für eine kombiniertmyofunktionell-kieferorthopädische Frühbehandlung - Teil 3. Ortho Orofacial 3.
- Hotz R: Orthodontie in der täglichen Praxis: Huber; 1954.
- Flutter J (2006) The negative effect of mouth breathing on the body and development of the child. Int J Orthod Milwaukee 17(2): 31-37.
- Grabowski R, Stahl F (2008) Die offene Mundhaltung im Kindesalter – Häufigkeit und Folgewirkungen. Informationen aus Orthodontie & Kieferorthopädie 40: 101-109.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.