Down Syndrome Female with Acquired Complete Labial Fusion: A Case Report
by Suzan Alshdefat1*, Wafa Alsardieh2, Rana Alshdaifat3, Yazan Mahafza4
1Consultant Obstetrics and Gynecology, Ain Alkhaleej Hospital, Al Ain, United Arab Emirates
2Senior Resident, Obstetrics and Gynaecology Department, Faculty of Medicine, Jordan University Of Science and Technology, Irbid, Jordan
3Full Time Lecturer, Adult Health Nursing, Princess Salma Faculty of Nursing, Al Albayt University, AL Mafraq, Jordan
4Super-microsurgery & Lymphatic Reconstruction Research fellow, department of Plastic Surgery, Cleveland Clinic Foundation, Ohio, USA
*Corresponding Author: Suzan Alshdefat, Consultant Obstetrics Gynecology & Gyn-oncology, Ain Alkhaleej Hospital, Al Ain, United Arab Emirates
Received Date: 01 December 2025
Accepted Date: 10 December 2025
Published Date: 15 December 2025
Citation: Alshdefat S, Alsardieh W, Alshdaifat R, Mahafza Y. (2025). Down Syndrome Female with Acquired Complete Labial Fusion: A Case Report. Ann Case Report. 10: 2078. https://doi.org/10.29011/2574-7754.102078
Abstract
The association of Down syndrome (DS) with complete labial fusion (CLF) in females has never been reported before; extensive literature review did not reveal any reported case. We present a unique case involving a 32-year-old female with DS, menopausal for two years; otherwise healthy. She sought medical attention for recurrent urinary tract infections, urinary incontinence and vulvar discomfort over the past year. A gynaecological examination revealed CLF, surgical release of labial adhesion was performed with excellent outcome. This case highlights the occurrence of labial fusion in patients with DS who are prone for early menopause and the associated genitourinary syndrome of the menopause (GSM) and underscores the efficacy of labial reconstruction and adhesion release in such patients.
Keywords: Down Syndrome; Complete Labial Fusion; Genitourinary Syndrome Of The Menopause; Postmenopausal Labial Fusion; Trabeculated Wall.
Introduction
Trisomy 21, the presence of an extra chromosome 21, leads to a set of clinical features collectively known as Down syndrome [1]. DS is one of the most genetically intricate conditions that can survive post-term, and the most prevalent autosomal aneuploidy [1] , as the world's population grows, the lifetime prevalence of DS increased substantially, for instance, in the United States(US), the prevalence of DS rose from approximately 50,000 cases in 1950 (3.3 per 10,000 individuals) to around 212,000 in 2013 (6.7 per 10,000 individuals), largely due to improvement in the survival rates of children with DS [2,3]. The life expectancy for individuals with DS in the U.S has also improved dramatically, increasing from an estimated average of 26 years and a median of 4 years in 1950 to 53 years and 58 years, respectively, by 2010 [4]. women with DS experience menopause at an earlier age and this may be associated with accelerated aging [4] The earlier-than-expected age at onset of menopause suggests that women with DS are at an increased risk for post-menopausal health disorders [5] this leads to the occurrence of some of the unusual conditions associated with menopause in younger women with DS, as the case of our patient.
CLF constitutes a severe form of genitourinary syndrome of the menopause (GSM) [6]. caused by the decline in estrogen levels with aging [7]. The partial or complete adherence of the labia minora towards the midline is described in the literature as labial fusion, vulvar fusion, synechia of the labia minora, adhesions, or agglutination or conglutination of the labia minora [8]. Postmenopausal labial fusion constitutes a severe form of GSM [7]. In severe cases, the labia minora are completely attached to each other at the midline and no opening at the level of the introitus can be found on clinical examination; this is termed complete labial fusion (CLF) [9], labial adhesion is common before puberty and after menopause, it is thought that estrogen deficiency plays a major role in the formation of adhesions [10].
The exact cause of CLF is not known, but sometimes it occurs after an inflammation of the labial area (e.g. after a simple infection such as vulvovaginitis, or after mild trauma to the area).
CLF has been linked to a condition described as pseudoincontinence [11]. Women with pseudo-incontinence complain of continual dribbling of urine that cannot be classified either as stress urinary incontinence (SUI) or as urge urinary incontinence (UUI). In the literature, remission of pseudo-incontinence is clearly demonstrated after the correction of the CLF [12].
If the labial fusion is causing significant problems (e.g. problems urinating), treatment options may include gentle massage or applying estrogen cream; surgery to pull apart the labia is a last resort. Surgical separation of the complete labial fusion appears to have good long-term anatomic and functional outcome [13].
Case presentation
A 32-year-old female, DS (47 XX, +21), menopausal for 2 years, she was examined at birth and told to have normal genitalia. She presented to our clinic complaining of 1-year history of recurrent UTI, urinary incontinence and vulvar discomfort. Her medical history is significant for hypothyroidism post Iodine ablation of the thyroid gland at the age of 10, and since then she is on thyroxine.
On physical examination, she appeared well, her height was on the 10th centile and weight was in the 90th centile, as measured for age and sex according to DS growth charts, gynecologic exam revealed CLF with a few millimeters pin hole in the middle of the fusion line (Figure 1), No other abnormalities were found, except for the physical features of DS (slanting eyes, epicanthic folds, and protruding tongue) she has no other abnormalities.
Trans-abdominal ultrasound examination revealed normal appearing anteverted uterus with small normally looking both ovaries.

Figure 1: Pelvic MRI showing complete labial fusion with a small central pinhole opening.
Pelvic MRI: the uterus appears normal in shape and position with normal slightly small in both ovaries, the bladder showed normal contour and shape with slightly thickened trabeculated wall, normal anatomical position and relation of the urethra, vagina, and rectal opening, the rest of the report is unremarkable. [14-18]
Treatment
The patient was placed in lithotomy position under sedation and local anesthesia. After prepping and draping, infiltration of the fusion line started by injecting (Lidocaine and Adrenaline) locally. Left labial biopsy taken (histopathology: vascularized fibrous tissue with prominent nerve fibers and chronic inflammation). At first manual separation of the labia minora was attempted trying to gently separate the fused labia in a lateral direction with both index and thumb fingers, (Figure 2,3), this was unsuccessful.
A surgical incision was made through the fusion line, we were able to visualize the vaginal orifice (identified using surgical forceps), and the urethral orifice, a Foleys catheter was inserted.

Figure 2: Attempted manual separation of the fused labia minora.

Figure 3: Incision through the fusion line exposing the vaginal and urethral openings.

Figure 4: Layered suturing of the separated labia minora.
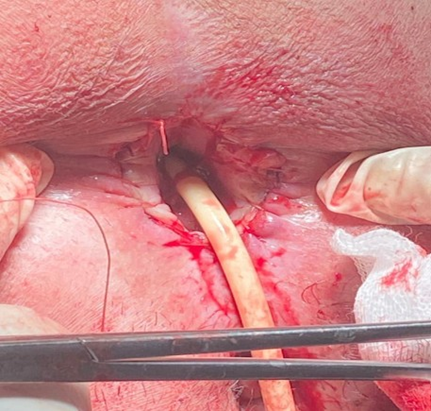
Figure 5: Reconstructed labial edges following surgical separation.
Separate sutures (Vicryl 2.0) were used to close the opened incision and approximate the edges of each labia minora in two layers, as the skin was tight over the edges, (Figure 4, 5). After finishing closure of the skin, the outcome is seen in (Figure 6,7).
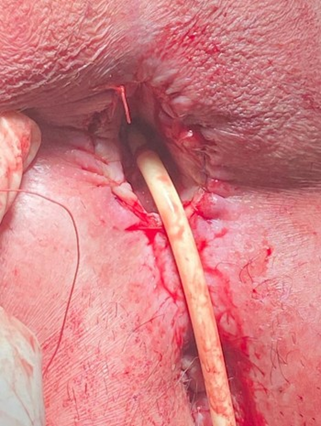
Figure 6: Immediate postoperative appearance after labial reconstruction.

Figure 7: Final postoperative outcome showing restored vaginal introitus.
Postoperative Care
Postoperatively, the foleys catheter removed the same night; she ambulated, and was discharged the following day on analgesia and a 5-day course of second-generation cephalosporin. Topical estrogens were prescribed for 6 months after the procedure, every day for two weeks, twice weekly thereafter; instructions were given for proper hygiene of the genital area; the first postoperative follow-up visit was after 2 weeks and she did really well with complete resolution of the urinary incontinence and vulvar discomfort.
Ethical Considerations: An informed consent was obtained from the patient father to take pictures of her condition and the surgical procedure and to publish her unique case.
Conflict of Interest: All authors declare no conflict of interest, no financial support was provided for this work from any source.
References
- Antonarakis SE, Skotko BG, Rafii MS, Strydom A, Pape SE, et al. (2020). Down syndrome. Nature Reviews Disease Primers. 6: 9.
- De Graaf G, Buckley F, Skotko B. (2019). People living with Down syndrome in the USA: Births and population. Down Syndrome Education International. 3: 1-5.
- De Graaf G, Buckley F, Skotko BG. (2017). Estimation of the number of people with Down syndrome in the United States. Genetics in Medicine. 19: 439-447.
- Schupf N, Zigman W, Kapell D, Lee JH, Kline J, et al. (1997). Early menopause in women with Down’s syndrome. Journal of Intellectual Disability Research. 41: 264-267.
- Seltzer GB, Schupf N, Wu HS. (2001). A prospective study of menopause in women with Down’s syndrome. Journal of Intellectual Disability Research. 45: 1-7.
- Mikos T, Lioupis M, Grimbizis GF. (2019). Postmenopausal complete labial fusion and pseudo-incontinence: A case series. Case Reports in Women’s Health. 21: e00101.
- Gandhi J, Chen A, Dagur G, Suh Y, Smith N, et al. (2016). Genitourinary syndrome of menopause: An overview of clinical manifestations, pathophysiology, etiology, evaluation, and management. American Journal of Obstetrics and Gynecology. 215: 704-711.
- Girton S, Kennedy CM. (2006). Labial adhesion: A review of etiology and management. Topics in Obstetrics & Gynecology. 26: 1-5.
- Julia J, Yacoub M, Levy G. (2003). Labial fusion causing urinary incontinence in a postmenopausal female: A case report. International Urogynecology Journal. 14: 360-361.
- Capraro VJ, Greenberg H. (1972). Adhesions of the labia minora: A study of 50 patients. Obstetrics & Gynecology. 39: 65-69.
- Girton S, Kennedy CM. (2006). Labial adhesion: A review of etiology and management. Topics in Obstetrics & Gynecology. 26: 1-5.
- Acharya N, Mandal AK, Ranjan P, Kamat R, Kumar S, et al. (2007). Labial fusion causing pseudoincontinence in an elderly woman. International Journal of Gynecology & Obstetrics. 99: 246-247.
- Mikos T, Lioupis M, Grimbizis GF. (2019). Postmenopausal complete labial fusion and pseudo-incontinence: A case series. Case Reports in Women’s Health. 21: e00101.
- Peng L, Baradar AA, Aguado J, Wolvetang E. (2023). Cellular senescence and premature aging in Down syndrome. Mechanisms of Ageing and Development. 212: 111824.
- Dube R. (2016). An approach to women with labial agglutination at different stages of life: A review. International Journal of Advanced Multidisciplinary Research. 3: 1-10.
- Chang CP, Hsu FK, Lai MJ, Lee HL, Horng HC, et al. (2020). Voiding difficulty due to nearly complete labial fusion in a post-menopausal woman. Taiwanese Journal of Obstetrics & Gynecology. 59: 621-622.
- Maeda T, Deguchi M, Amano T, Tsuji S, Kasahara K, et al. (2021). A novel surgical treatment for labial adhesion – The combination of Z-and YV-plasty: A case report. Case Reports in Women’s Health. 32: e00363.
- Santos-Neto OO, Mariano MH, Marques-de-Faria AP, Andrade JGR, Vieira TAP, et al. (2021). Association between Down syndrome and disorders of sex development: Report of three cases and review of 188 cases in the literature. Sexual Development. 14: 3-11.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.