Diagnostic Imaging of the Patellar Height with Own Proposition of Patellar Height Measurement Criteria
by Zbigniew Czyrny*
Private Practice, Enel-Sport, Warszawa ul. Łazienkowska 3, Warszawa, Poland
*Corresponding author: Zbigniew Czyrny, Private Practice, Enel-Sport, Warszawa ul. Łazienkowska 3, Warszawa, Poland, zbigniew.czyrny@wp.pl
Received Date: 11 February 2025
Accepted Date: 17 February 2025
Published Date: 19 February 2025
Citation: Czyrny Z (2025) Diagnostic Imaging of the Patellar Height with Own Proposition of Patellar Height Measurement Criteria. Arch Surg 5: 123 https://doi.org/10.29011/3066-2559.000023
Summary
The paper presents author’s experience and view on the evaluation of one of the parameters defining Patello-Femoral Joint (PFJ)-The patellar height. The proposition of patellar height measurement is based on biomechanics of the PFJ.
Keywords: Patellar height; Patello-femoral joint; US; Xray; MRI.
Introduction
Patellar height is one of many factors defining a predisposition of the PFJ to develop anterior knee pain in some time of life. Particular role of patella is that it is a part of a pulley which is smoothly changing the vectors of forces generated by the extensor mechanism during movement and in static positions. Patella glides on femoral trochlea and with it forms (or not) a Patello-Femoral Joint (PFJ). All the elements of the extensor mechanism at least in part insert to the patella and interweave their fibers there, to finalny attach directly or indirectly to the femur or tibia. The extensor mechanism is a complex of tendons and ligaments which attach to the patella to control its position against femoral condyles during movement and in static positions from full flexion to full extension.
Extensor apparatus consists of:
- Tendons of the quadriceps femoris muscle,
- Lateral retinaculum,
- Ilio-tibial tract,
- Lateral patello-tibial ligament,
- Medial retinaculum (medial patello-femoral ligament),
- Medial patello-tibial ligament,
- Patellar ligament.
Important factors contributing to patellar stability and wellbeing:
- The angle/depth of the upper part (max 10mm) of the femoral groove,
- The axis of the limb,
- Rotation of the shin,
- Rotation of the femur,
- Localization of the tibial tuberosity/patellar ligament insertion,
- Efficiency and balance of the forces generated by the extensor mechanism.
It is as it looks-the patellar height is one of many factors which influence on pain-free loads generated in PFJ. Patellar stability is burdened by many variables, of which the most important are patellar height and upper part of the femoral groove angle/depth.
Patellar Height Measurement
Before we start with patellar height measurement one fundamental question must be stated - what does it mean for the PFJ, high, normal or low patella? The name patello-femoral joint directly suggests that we should focus on patella and femoral condyles.
Particurally the position of the patellar to femoral cartillage. There are many methods of patellar height measurement. The first group are indirect indexes of different component of the patellar length and the distance between different points of patella and tibia. Available in the literature indexes belong to Insall-Salvati, Blackourne-Peel, Caton-Deschamps, de Carvahlo, Micheli, Egund, Koshino i Sugimoto, Grelsamer i Meadows, Leung [1]. Many indexes, nobody knows which is good. In fact it is hard to say what they actually represent in terms of an idea. Fundamental fault of all of them is the patello-tibial distance which doesn’t have anything to do with the patello-femoral joint. Second group are indexes based on the relation between the patella and the femur. Some of them are indexes by Bernageau, Labell, Norman, Hepp, Bugress, Miller, Seyahi, Biedert and Albrecht [1-3].
The most popular and recommended by medical societys are index of Insall-Salvati and Caton-Deschamp. I would like to stop on them because they are completely ridiculous but popular in many countries. Insall-Salvati (Figure 1) is based on the length of the whole patella from the apex to the base (lateral xray knee flexed 30⁰) and the length (not defined where it should be measured except that at the tibial insertion of the patellar ligament, which length varies from 2 to 4cm) The relation between the patellar length and the length of the patellar ligament should measure 1,02 (!). So it is a quotient of the patellar ligament length and patellar length. A complete nonsense carying no useful information about the PFJ. It means that all indirect indexes are useless in terms of PFJ homeostasis. Nearly the same situation with the Caton-Deschamp (Figure 2). The idea is identical, Only slightly modified. The difference is that instead of full patellar length the patellar articular surface is used and the distance from patella to tibia is measured between different points. As useless as Insall-Salvati.
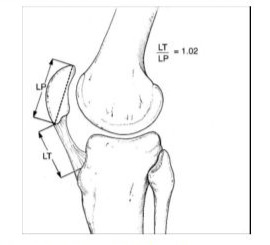
Figure 1: Insall-Salvati patellar height measurement method.
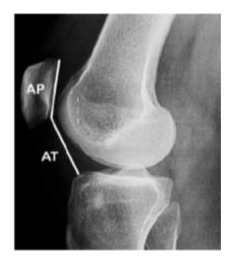
Figure 2: Caton-Deschamp patellar height measurement method.
For completely different reasons I need to say about patellar height measurement metod published by a radiologist Bernageau [1,2]. I based my measurements on his metod (Figure 3).
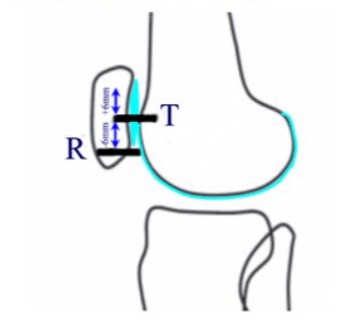
Figure 3: Bernageau patellar height measurement method. . Line R - Lower margin of the patellar cartillage, line T - Upper margin of the cartillage of the femoral condyles (the border between epiphysis and metaphysis). Line R should, according to Bernageau, be max 6mm below or above Line T. The knee extender with quadriceps femoris muscle tension.
Bernageau as first relates patellar cartilage distal margin (Line R) to femoral condyles cartillage upper margin (Line T), and all that in full extension with quadriceps femoris muscle tension. Bernageau analysed 44 patients and drew a conclusion that the normal patella is when Line R is max 6mm below or above Line T. It is Worth commenting on paper by Roland M. Biedert i Silvia Albrecht. The index proposed by the authors i salso based on relation of Line R and Line T but the measurement criteria are different. This paper, similarly to Bernageau’s i salso a population-based work with 66 knees MRI scanned in patients without anterior knee pain. Similiarly to Bernageau the number of patients is small. Second fault is that the kenes were scanned if full extension but without quadriceps muscle tension. Tension of the quadriceps musle in an extended knee will rise the patella by 2-5mm what is easily observed in US scanning in the relaxed and tensioned muscle. That means that criteria for the measurement itself are not repetitive. The third problem is the lack of grup of patients with anterior knee pain. In this work I use Bernageau’s metod but propose different, logical criteria, based on the PFJ biomechanics, and their usefulness for the surgeons [3].
High Patella (Patella Alta)
High patella criteria are easy and simple (Figure 1).
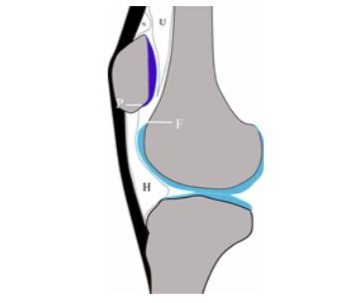
Figure 4: A scheme showing the idea of high patella - no contact of the patellar and femoral cartillage in full extension and quadriceps muscle tension. Line of the distal margin of the patellar cartillage (line P for patella) is above the line of the proximal margin of the femoral cartillage (line F for femur). N - suprapatellar fat fold, U - femoral fatty fold, H - Hoffa fat pad.
High patella is the situation where there is no contact od the PFJ cartillages in full extension and quadriceps muscle tension. Patella instead is lying on femoral fattty fold. In the setting of PFJ presented on Figure 4 patello-femoral joint is a potential structure when carillages don’t touch each other and actually starts working in small degrees of flexion of the knee - when the cartillages will start overlapping and if there is trochlear femoral groove then the patella is stabilised. This stabilisation will be called hard patella stabilisation. What happens when the patella is not hard-stabilised by a femoral groove? It is compressed against soft femoral fatty fold and it is stabilised only by the extensor apparatus and influenced by factors mentioned before deciding on patellar stability. Patella alta is in most cases prone to lateralization, subluxation or even dislocation. I would like to stress here that high patella is an element predisposing to patellar instability not defining it [4,5].
Normal Patella
Normal patellar height range (Figure 2) means tere is contact of the PFJ surfaces in full range of motion, and that means in full extension with quadriceps femoris muscle tension. This is the position of the leading leg preparing for the next step.
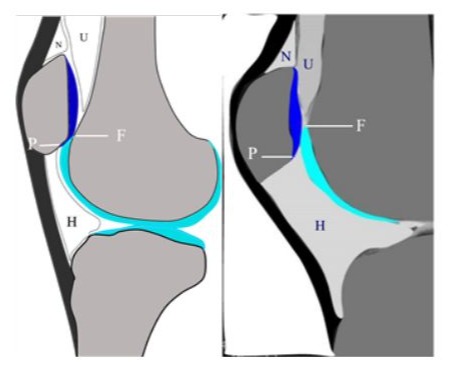
Figure 5: Schemes presenting normal patellar height - tere is contact of articular surfaces of the PFJ from 1 to teen mm, but no more overlapping of the cartilages than 40% of the patellar cartillage length. Line P is below Line F. N - suprapatellar fat fold, U - femoral fatty fold, H - Hoffa fat pad.
This range of patellar positions is the best from the PFJ stand point because the patella is hard-stabilized (if the intertrochlear groove is deep enough in its upper part) in the extended knee with quadriceps muscle tension applied. In extension only the lower part of the patella is compressed against upper femoral condyles and most of the patellar cartillage is resting on the femoral fat pad not un the hard condyles [6].
Low Patella
Low patella is a bit more difficult than criteria for high patella. And it is difficult not only for there is no strict definition of what low patella means for the PFJ. Majority if not all of norms are based on population based data. I present a proposition of biomechanical approach to this problem. It seems that 40% of the patellar cartillage surface length of PFJ cartillages overlapping is already dangerous. Patella at this point is nearly maximally anteriorrly placed in relation to femoral condyles which means that the vector compressing the patella against femoral condyles is submaximal . So between 40% and 50% is a danger zone. Starting from 50% of cartillages overlapping the patella is placed most anteriorly therefore the compression vector is maximal [7].
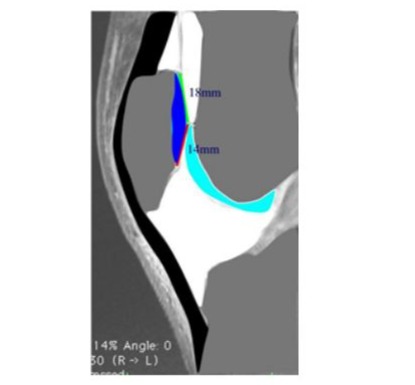
Figure 6: PFJ cartillages overlapping by 40% of the patellar cartillage length. Patella is nearly maximally anteriorly placed what generates larger compression vector than in normal or high patella.
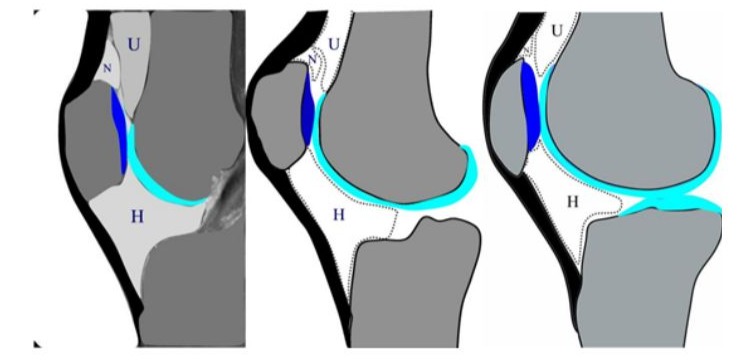
Figure 7: Schemes of low patella staring from approx 60% to 100% overlapping. Articular patellar surface (line P) ovelaps femoral condyles surface by more than 40% of the patellar cartillage length (line P below Line F). N - suprapatellar fat fold, U - femoral fatty fold, H - Hoffa fat pad. Note that the patella in the middle and on the right would be high patella by Insall-Salvati and Caton-Deschamp!
One thing in this definition of the patellar height is certain - the patella never rests. It is for the lifetime compressed against femoral condyles with maximum force and never rests on the femoral fatty fold. Its lower part never articulates with femoral condyles. In the situation of more than 40% overlapping of the PFJ surfaces the vectors generated by the extensor mechanism are at the smaller angle therefore generate larger resultant vector compressing the patella against femoral condyles than in normal or high patella. Morover patella never rests on the femoral fatty fold.
Of course low patella means the opposite of high patella - overstability of the patella. We can describe that state as excessive pressure in the PFJ, not necessarily lateral or medial, that is depending on many other factors located in and outside the knee. The thing is that the pain in both low and high patella will be the same and the therapeutic procedures not so much. Of course when you are out of luck and have a low pain threshold the anterior knee pain will appear no matter what. That also depends on the level of exploitation of ten locomotor system.
Diagnostic Methods for Patellar Height Measurement
It seems that the best and cheapest is lateral Xray in a standing position with knee hyperextended and quadriceps femoris muscle tension applied (Figure 5) - it is a simple and repetitive method showing most proximal patellar position.

Figure 8: Patellar height measurement on an lateral Xray of the hyperextended knee and quadriceps muscle tension. Line P - orange, Line F - yellow (the anterior end of the border between epiphysis and metaphysis). Normal patellar height.
Secon, as good ast the Xray, but unfortunately much more expensive is MRI (Figure 6). However there is a little trick to it for no patient would stand a 12minutes sequence with quadriceps muscle tension. We need a 2-4, 4-5mm slices sequence which lasts approx 35seconds. Slices located in the middle towards lateral edge of the lateral femoral condyle. This time of musce tension is well tolerated and in most cases the images are clear. Even if they are a bit shaky it is still good for measurement and proper definition of patellar height in an extended/hyperextended knee with quadriceps muscle tension [8].
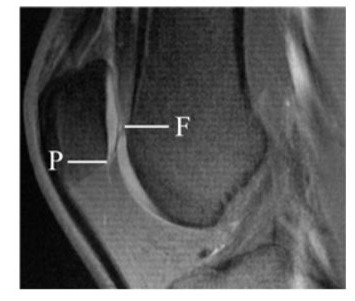
Figure 9: One slice of 4slices 4mm thick ready for measurement. Knee extended/hyperextended with quadriceps muscle tension applied. Slice in the mid-lateral part of the lateral femoral condyle. Overlapping below 30% - normal.
A method worthy mentioning is dynamic US examination of the patellar height. It is mainly useful in high/normal patella. In high patella we can be a 100% sure that there is no contact of the patellar and femoral cartilages when the apex of the patella shadows at the upper margin of the femoral cartillage or higher (Figure 7). We asses patellar height with knee extended/hyperextended and quadriceps muscle tension applied. One word of explanation why we can be sure about high patella in US examination - patellar types according to Grelsamer (Figure10).
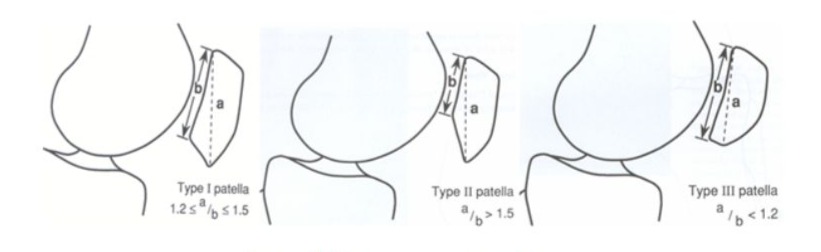
Figure 10: Patellar types according to Grelsamer.
Grelsamer highlited three types of patella depending on the value of the index of the total patellar lengt/cartillage length. In my own research 105 MRI examinations were vieved in the sagittal planes. Type I Grelsamer - 94 knees, type II - 1 knee, type III 10 knees. This means that the patellar cartillage lower margin is approx. at least 3mm above the patellar apex which is our landmark. So it is enough that we see upper margin of the femoral cartillage for the diagnosis of high patella with 90% accuracy. If the ortopedist needs to find out how high the patella is, an Xray or MRI solves the problem. Ultrasound is not of much use in low patella but it can be a flag warning for the ortopedist to look into PFJ more carefully on other modalities.
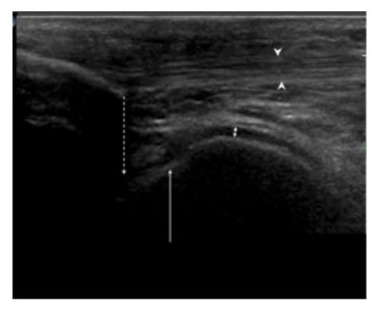
Figure 11: US, sagittal with knee extended and quadriceps muscle tension applied. High patella - the apex (hyphenated arrow) is shadowing approx 4mm above the F line (long arrow). To that we can add min 3mm. That adds up to 7mm high patella. Arrowheads - patellar ligament margins, double arrow - femoral cartillage.
How to Write an Assesment
In case of high patella we give the distance between cartillage of the femur and patella. In case of normal and low patella we give the distance of overlapping of the femoral and patellar cartilages and we also measure the distance of the patellar cartillage length. In this way the clinician can judge for her/himself how serious is the problem if it exists. This approach to patellar hight measurement can be very useful in planning of distalization of the tibial tuberosity/patellar ligament insertion. If for example the patella is 5mm high and we have a good trochlear groove, the desired overlapping could be 8mm. So we have the result – 8mm+5mm=13mm of distalization resulting in optimal patellar height. Patellar height is one of several parameters of the PFJ, however very important, predisposing to patellar instability or hyperstability and anterior knee pain. High patella means lack of hard stabilisation in full extension and small angles of flexion and that means stability controlled only by extensor apparatus. The good news is that well carried out rehabilitation has a good chance to prevent the patient from anterior knee pain.
Low patella is a completely different story. Here we are coping with extensive patello-femoral pressure and patellar hyperstability which are difficult to controll by rehabilitation. If there is a technique allowing for proximalization of the tibial tuberosity it could be beneficial for these patients who othervise can be saved only by a high pain treshold.
References
- Phillips CL, Silver DAT, Schranz PJ, Mandalia V (2010) The measurement of patellar height. A Review of the Methods of Imaging. J Bone Joint Surg 92: 1045-1053.
- Roland M. Biedert, Silvia Albrecht (2006) The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc 14: 707-712.
- Fulkerson JP (1997) Disorders of the patellofemoral joint, III edition, Williams&Wilkins 1997.
- Fathian DC, Paxton EW, Stone ML, Silva P, Davis DK, et al. (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32: 1114.
- Koh Jl, Stewart C (2015) Paterllar instablity. Orthop Clin North Am 46: 147.
- Zaffagnini S, Dejour D (2010) Patellofemoral pain, Instability, and Arthritis. Clinical Presentation, Imaging, and Treatment 2010.
- Dejour (2021) Updated treatment guidelines for patellar instability: “un menu à la carte”. Journal of Experimenta Orthopedics 8: 109.
- Luyckx T (2009) Is there a biomechanical explanation for anterior knee pain in patientrs with patella alta? influence of partellar height on patellofemoral contact force, contact area and contact pressure. J Bone Joint Surg Br 91: 344.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.