Delayed Vascular Injury Caused by Retained Temporary Epicardial Pacing Wire Following Minimally Invasive Cardiac Surgery
by Syed Al Nahian1, Onaisa Shahzad1, Enoch Akowuah2*
1Cardiothoracic Surgery, South Tees NHS Foundation Trust Middlesbrough, United Kingdom
2Academic Cardiovascular Unit, South Tees NHS Foundation Trust and Newcastle University, UK
*Corresponding author: Enoch Akowuah, Academic Cardiovascular Unit, South Tees NHS Foundation Trust , Middlesbrough and Newcastle University, UK
Received Date: 30 July 2024
Accepted Date: 02 August 2024
Published Date: 05 August 2024
Citation: Al Nahian S, Shahzad O, Akowuah E (2024) Delayed Vascular Injury Caused by Retained Temporary Epicardial Pacing Wire Following Minimally Invasive Cardiac Surgery. Ann Case Report. 9: 1919. https://doi.org/10.29011/2574-7754.101919
Abstract
Temporary epicardial pacing wire (TEPW) placement is one of the key intervention the management of patient undergoing cardiac surgery, precisely in the immediate post-operative period. The placement of temporary epicardial pacing wire is not free of risks and can present with a hand full of complications. Here we report a case of 71 years aged male presenting with chest wall vascular injury and hematoma long time after his minimally invasive cardiac surgery. Patient was managed conservatively with excellent recovery.
Keywords: Retained Pacing Wire; Temporary Epicardial Pacing Wire; Minimally Invasive Cardiac Surgery; Chest Wall Hematoma.
Introduction
Temporary epicardial pacing wire (TEPW) placement is one of the key intervention the management of patient undergoing cardiac surgery, precisely in the immediate post-operative period. Despite advancements in surgical technique and perioperative management, dysrhythmia remains a common complication following cardiothoracic procedures. They are routinely used in majority of the cardiac operations to manage these dysrhythmias and conduction abnormalities, allowing for safe recovery and hemodynamic stability in the early post-operative period [1]. The use of temporary epicardial pacing-wire in cardiac surgery is well established throughout the world. TEPW are snuggly anchored to the epicardium with a view of ease of removal via traction from outside the chest before discharge of the patient, instances of any resistance the wires are cut flush with gentle traction at the skin [2] hence could be retained within the chest cavity in such situations. The placement of temporary epicardial pacing wire is not free of risks. Potential complication reported include haemorrhage, cardiac tamponade, wound infection, dysrhythmia, migration of pacing wire [3,4], even endocarditis with subsequent stroke [5]. We describe herein a rare and unprecedented complication of retained TEPW following minimally invasive mitral valve surgery presenting as large chest wall hematoma due to chest wall vessel injury.
Case Presentation
71 years old male with known paroxysmal atrial fibrillation (PAF) and Mitral valve prolapse presented with breathlessness on exertion. He was known to have mitral valve prolapse with minimal symptoms and was under follow up of cardiology team from 2013 to 2019, for his PAF he was not on any anticoagulation since his CHA2DS2 VASc score was 1 for his age and he had chosen to not be on anticoagulation due to history of gum bleeding with Rivaroxaban. His recent echocardiogram showed Normal LV systolic function, severe mitral regurgitation predominantly due to P2 prolapse extending to the medial aspect of P1 associated with rupture chordae and billowing of P3/A3, mild central aortic graduation, mild tricuspid reputation with dilated tricuspid annulus of 43 mm. He had an MDT discussion regarding further management and the MDT consensus was to go for surgical repair of the mitral valve and not to intervene on tricuspid valve. He was deemed suitable for minimally invasive surgery (mini mitral trial). Eventually he had successful minimally invasive mitral valve repair on March 2021 via right thoracotomy, procedure was a bit challenging due to the kyphotic anatomy but uneventful and he was weaned from bypass usually with having 2 atrial pacing wires. Post-operative recovery was uneventful; however, what team was unable to remove the temporary pacing wires hence cut them flashing to the skin with gentle traction. His routine six week follow up was unremarkable.
For following three years after the operation there were no issues, albeit he was slightly aware of the wires in his chest, and he could feel the end of them occasionally. In April 2024 while he was lying in bed, he felt a sharp pain in the upper right side off his chest with immediate small swelling, he rang 999 take it to the hospital by the time swelling was getting slightly bigger (Figure 1). On examination he was hemodynamically stable, with right sided chest pain, and bruising to the armpit and large approximately 10x 10 cm hematoma noted which had no thrill what the right pectoral muscle. Right arm distal neuro-vascular function was intact. Subsequently he had a contrast enhanced CT angiogram to exclude ongoing bleeding which showed a large mixed density collection within the right chest wall measuring approximately 14 cm x 7 cm (Figure 2). On portal venous phase it appeared to be a branching vessel coursing into the collection (Figure 3) and possible contrast excavation, suggestive more of a venous bleed from a very small subdivision of lateral thoracic artery. On the arterial phase no injuries to the right subclavian or axillary artery. He was admitted in the hospital for close monitoring of the progress of the hematoma, on next day he required blood transfusion following a witnessed collapse in the ward which unfortunately caused a fracture of his nose- he did not have any other injury. He was stable for next 3 days, repeat CT angiogram of the whole aorta showed a redundant pacing wire (Figure 4) overlying right pectoralis major muscle, large right chest wall hematoma compared to the previous one was unchanged, no injury to the right subclavian artery, and no extravasation of contrast in the arterial phase to suggest active bleeding. He was discharged in a stable condition with a follow up appointment after 6 weeks as an outpatient. On his follow up visit his hematoma/bruise disappeared and he was feeling well with all normal finding. Since his condition was stable and no further complication noted it was decided to monitor the area for now as chances of repeating this is very small with a view in mind that if this happened again to any extent we would certainly go in and remove the wires surgically. Patient was happy with the plan and agreed to be under follow up.
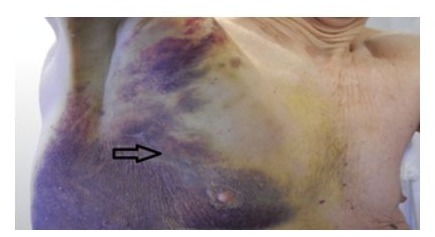
Figure 1: Photograph of the hematoma and bruise on right chest wall (Arrow - scar mark from lateral thoracotomy).
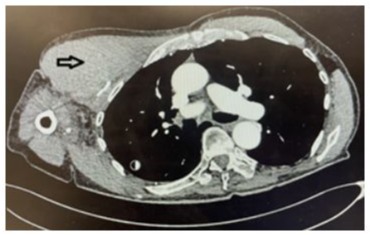
Figure 2: Contrast Ct angiography axial view showing large hematoma on the right side of the chest wall (Arrow hematoma on right chest wall).

Figure 3: A small branching vessel coursing to the extravasation on 3D reconstruction of CT angiogram coronal view 3D reconstruction.
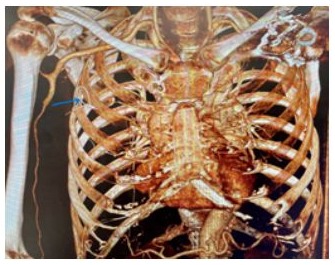
Figure 4: 3D reconstruction of bone window coronal section, arrow showing redundant pacing wire.
Discussion
Temporary pacing wires are almost routinely used at the end of cardiac surgical procedure to provide necessary support to cardiac rhythm in the post-operative period when required. They are usually placed on the surface of right atrium and/or right ventricle depending on the procedure and clinical requirement of the patient. Subsequent removal of the pacing wire usually takes place on 3rd to 5th POD depending on clinical status of the patient. This TEPW placement is in practice as there is very less complication with placing the wires in compared to the complication and risks associated with it. Unfortunately, this is not entirely without any risk. A recent systematic review of over 18,000 patient described incidence of overall complication of about 1.74% with temporary pacing wires with the most common ones being arrythmia, retention of wire, delayed discharge and cardiac tamponade [4]. While removing the TEPW if any significant resistance felt then usually it is cut flushed to the skin after gentle traction with a view to let it retract inside safely. However, this results in retention of the part of the wire within the chest cavity which in turns can potentially cause various complications. Recent literature confirmed majority of the retained TEPW undergoes some form of migration and presents with symptoms within six years (mean) of placement, with a range of 1 month to 24 years [6]. Several cases reported for rare complications of migration with retained epicardial pacing wire like, terminating in the left heart, ascending aorta, aortic arch, abdominal aortic aneurysm and pulmonary artery [7-10]. Additionally, cases with infective endocarditis with stroke [5], migration of retained TEPWs in colon [11] even stomach causing dyspepsia [12] has been reported. To the best of our understanding, chest wall hematoma following minimally invasive cardiac surgery due to retained TEPW has not been reported till now. Our probable conjecture is that the wire was not cut properly flushed with the skin after gentle traction which essentially left it with more redundant segment in the tissue with a sharp end and subsequent injury to the small chest wall vessel. Experienced radiological diagnosis along with proper history, examination and reconfirming documentation of pacing wire removal was the key steps for correctly diagnosing this case. As the complication was managed with minimal intervention and without any major complications, we chose to settle for wait and watch strategy rather than going for more invasive redo surgical intervention. Albeit the chance of any similar injury is extremely small, should there be a second event we would prefer to intervene surgically straightway to remove the retained wire.
Conclusion
Use of temporary pacing wire is considered generally to be a safe procedure with a small number of complications. Temporary epicardial pacing wire retention is one of the recognised complications. Once retained it has potential to present with various form of complication even after long time after the initial procedure. Timely identification and rational intervention approach should be taken on an individual case basis based on risk versus benefit and severity of the complications.
Conflict of interest: The authors have no conflict of interest in the current publication.
References
- Reade MC. (2007) Temporary epicardial pacing after cardiac surgery: a practical review. Part 1: general consideration in the management of epicardial pacing. Anaesthesia 62: 264-271.
- Shaikhrezai K, Khorsandi M, Patronis M, Prasad S. (2012) Is it safe to cut pacing wires flush with the skin instead of removing them? Interact Cardiovasc Thor Surg 15: 1047-1051.
- Rahmouni K, Hebert Y, Pellerin M, Perrault LP. (2021) Sudden tamponade from vein graft side branch avulsion on removal of temporary pacemaker wires. Ann Thorac Surg 112: e23-e25.
- Mubarak FS, Ellepola Y, Chamba KN, Agrawal S, Makhoul M. (2023) Complications of epicardial pacing wire removal following adult cardiac surgery: A systematic review. Cerues 15: e49076.
- Dyal HK, Sehgal R. (2015) The catastrophic journey of a retained temporary epicardial pacemaker wire leading to Enterococcus faecalis endocarditis and subsequent stroke. BMJ Case Rep Published online.
- Wald G, Van YR, Pain KJ, Otterburn DM. (2020) Retained Temporary Epicardial Pacing Wires: A Systemic Review and Treatment Algorithm. Ann Plast Surg 85: S44-S49.
- Hua JD, Ali SS, Reddy V, Patel SJ. (2020) Wandering Atrial Pacemaker Wire: Migration of a Temporary Epicardial Pacing Wire Into the Left Heart. JACC Case Rep 2: 1046-1048.
- Wolf LG, Scaffa R, Maselli D, Weltert L, Nardella S, et al. (2013) Intraaortic migration of an epicardial pacing wire: percutaneous extraction. Ann Thor Surg 96: e7-8.
- Mukaihara K, Yotsumoto G, Mutsomoto K, Imoto Y. (2015) Migration of a retained temporary epicardial pacing wire into an abdominal aortic aneurysm. Eur J Cardiothor Surg 48: 169-170.
- Kageyama S, Ohashi T, Kojima A. (2024) Temporary Epicardial Pacing 12. Aksaka G, Kubat E, Erdogan MA, Unal CS. (2016) An Unusual Case of Wire Migration to the Pulmonary Artery in the Early Postoperative Dyspepsia due to retained epicardial pacing wire. Acta Gastroenterol Stage. Cureus 16: e56446. Bel 79: 509-510.
- Gonzales S, White H, Echavarria J. (2015) Transcolonic Migration of Retained Epicardial Pacing Wires. Case Rep Radiol 2015:416587.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.