Deficient Rectovaginal Septum and Uterine Prolapse through the Anal Margin
by Fatima Sheerin*, Joanne Bennett
Gloucestershire Hospitals NHS Foundation Trust, Alexandra House, Cheltenham General Hospital, Sandford Rd, Cheltenham GL53 7AN, United Kingdom
*Corresponding author: Fatima Sheerin, Gloucestershire Hospitals NHS Foundation Trust, Alexandra House, Cheltenham General Hospital, Sandford Rd, Cheltenham GL53 7AN, United Kingdom
Received Date: 12 July 2024
Accepted Date: 16 July 2024
Published Date: 18 July 2024
Citation: Sheerin F, Bennett J (2024) Deficient Rectovaginal Septum and Uterine Prolapse through the Anal Margin. J Surg 9: 11088 https://doi.org/10.29011/2575-9760.11088
Abstract
Background: Rectovaginal septum keeps the urogenital system and the anorectum separate. This report describes a unique case of uterine prolapse through the anal margin with a deficient rectovaginal septum. To the best of our knowledge, there are no previous reports detailing a similar presentation.
Case Presentation: A 90 year old woman was referred to the Colorectal team with what seemed to be a rectal prolapse. On Examination under anesthesia, she was found to have a uterine prolapse through the anus. This was successfully repaired after a vaginal hysterectomy, anterior repair and perineal reconstruction.
Conclusion: Multidisciplinary evaluation forms an integral part of the surgical management of rare rectovaginal septal defects, and approaches to such cases must be individualized.
Introduction
Prolapse is a condition in which an organ (rectum or uterus) gets displaced downward to protrude out through the anus or vagina. Normally, rectovaginal fascia keeps rectum and vagina separate. Defect in the fascia can result in vaginal herniation into rectum, and vice versa [1]. When small, patient might be asymptomatic. As the size of the defect increases, prolapse can become apparent [2]. Multiparity, Childbirth, trauma and congenital weakness of supporting ligaments are recognized risk factors of pelvic organ Prolapse [3]. We came across a rare case of uterine prolapse through the anal margin with deficient rectovaginal septum.
Presentation of Case
The patient is a 90-year-old woman who was referred to the colorectal department for assessment of her colostomy and management of a full-thickness rectal prolapse. Colostomy was made as an emergency in 1983 for IBD so no operation notes were available. She was seen in a Colorectal outpatient clinic with a stoma nurse on 11-11-2021. She had started noticing a lump around her stoma since 2020 which bled frequently, and what appeared to be a rectal prolapse that bled and caused discomfort. On examination her colostomy was sited in the left iliac fossa, was stenosed and had a pedunculate lesion at the mucocutaneous junction which looked like a pyogenic granuloma. Rectal Prolapse was patulous and full thickness and had some apical ulceration. It was reducible and the surrounding skin and sphincters appearing markedly atrophic. The plan was to book her for a Flexible Sigmoidoscopy prior to the combined procedure of excising the lesion at the colostomy site and applying a Thiersch wire around the anus.
Flexible sigmoidoscopy reported a severe stenosis short way up into the rectum, which was confirmed by digitation. During the wait for the procedure, colostomy site lesion had increased significantly in size and was believed to be causing a degree of obstruction & anemia. Hence, she was listed for revision of the stoma and Thiersch wire insertion on 15-02-2023. Her colostomy was revised and the granulomatous lesion sent away for histology. However, during examination of her perineum she had a completely deficient recto-vaginal septum and what was initially believed to be a rectal prolapse actually turned out to be her uterus prolapsing out of the anal margin. There was only a thin flap of skin between vaginal and anal orifices. There was very little rectal mucosa left and no rectal lumen. Patient was also examined by a gynecologist intra-operatively who agreed with the findings and suggested a vaginal hysterectomy with pelvic floor repair, & potentially a Sacrospinous fixation and rebuilding of her perineum. Hence, she was listed for a joint procedure between Colorectal and Gynecology on 19-04-2023 (Figure 1-5).
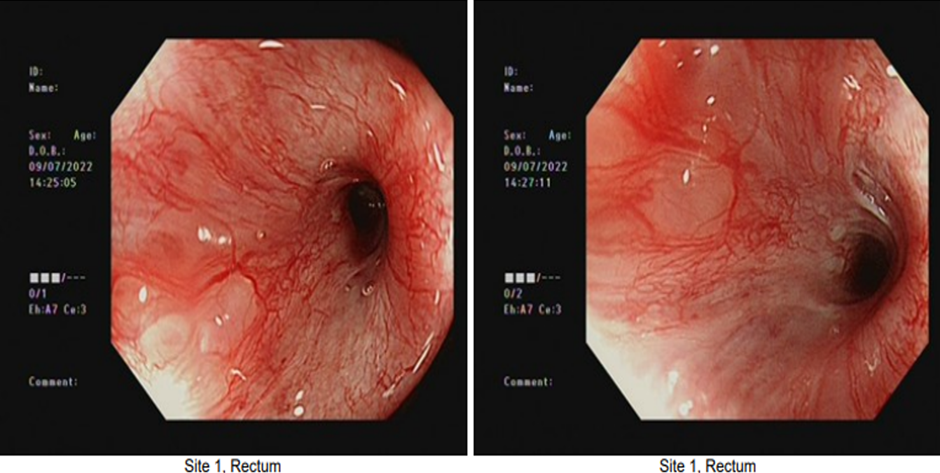
Figure 1: Images from Flexible Sigmoidoscopy.

Figure 2: Uterine Prolapse through the anal margin.

Figure 3: Atrophied rectal mucosa.

Figure 4: Deficient rectovaginal septum.

Figure 5: Uterus reduced for total Vaginal Hysterectomy.
The procedure carried out was Vaginal Hysterectomy, Anterior Repair, Sacrospinous Fixation and Perineal Reconstruction (Figure 6).
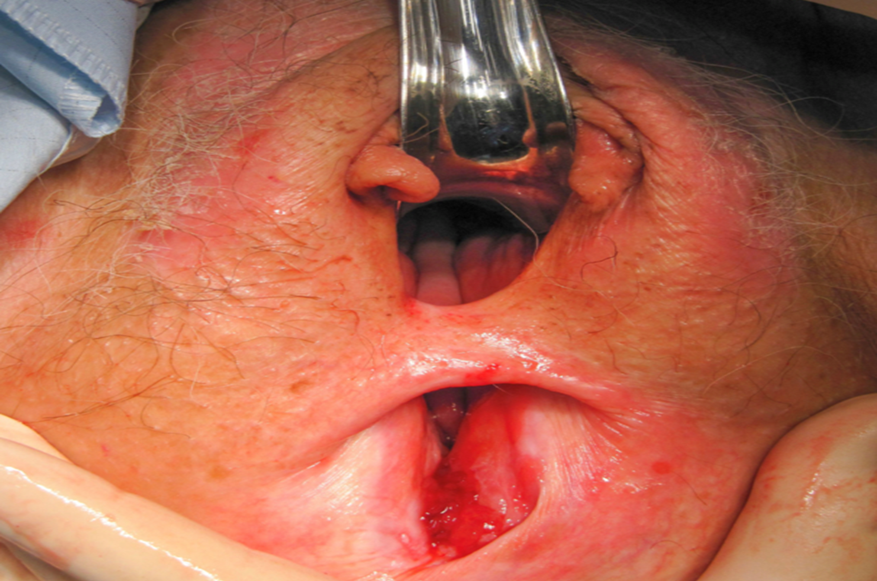
Figure 6: Perineum following Vaginal Hysterectomy and Reconstruction.
Discussion and Conclusion
There has been a lot of controversary regarding the rectovaginal septum, with a group of clinicians only considering it as a potential space while others insisting that it is a distinct structure. People who advocate the latter describe it to be synonymous with the Denonvillier’s fascia [4]. According to Aigner et al [5] it is a ‘clearly defined plate in the coronal plane consisting of fibrous connective tissue and longitudinal muscle fibers between the rectum and the vagina’. It joins the uterosacral ligament complex with the perineal body and prevents formation of a rectocele. To the best of our knowledge, there is no mention in the literature of a case of uterine prolapse through the anal margin due to an absent rectovaginal septum. Hence, there are no established standard surgical approaches for this condition. Anterior colporrhaphy is plication of pubo-cervical fascia in an attempt to correct anterior vaginal wall prolapse. Vaginal Sacrospinous Ligament Fixation involves suturing the cervix or vagina to the sacrospinous ligament with non-absorbable sutures. It can be done anteriorly and posteriorly, and can be both unilateral or bilateral [6]. In our patient we used a combination of vaginal hysterectomy, anterior colporrhaphy, sacrospinous fixation and perineal reconstruction. After vaginal hysterectomy, a midline anterior incision was given and bladder and fascia were reflected. Buttressing was done using 6 X 2.0 vicryl sutures. The vault was then closed with a continuous vicryl 1 suture. Posterior vaginal wall was then opened and sacrospinous fixation using 2 x PDS sutures were used to support the vaginal vault. Lavator Ani plication was performed and the perineal muscles stitched with interrupted 2/0 Vicryl to form rectovaginal septum. Following this, posterior recess was opened and vicryl 2.0 was used to recreate the perineal body. To conclude, rare cases pose unique challenges in pelvic floor surgery, however, individualized, multidisciplinary approaches can lead to successful results.
Reference
- Beck DE, Allen NL (2010) Rectocele. Clin Colon Rectal Surg 23: 90-98.
- Bump RC, Norton PA (1998) Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am 25: 723-746.
- Schaffer JI, Wai CY, Boreham MK (2005) Etiology of pelvic organ prolapse. Clin Obstet Gynecol 48: 639-647.
- Dietz HP (2011) Can the rectovaginal septum be visualized by transvaginal three-dimensional ultrasound? Ultrasound Obstet Gynecol 37: 348-352.
- Aigner F, Zbar A, Ludwikowski B, Kreczy A, Kovacs P, et al. (2004) The rectogenital septum: morphology, function, and clinical relevance. Dis Colon Rectum 47: 131-140.
- Ouzaid I, Ben Rhouma S, de Tayrac R, Costa P, Prudhomme M, et al. (2010) Sacrospinofixation mini-invasive avec le dispositif CAPIO : étude anatomique [Mini-invasive posterior sacrospinous ligament fixation using the CAPIO needle driver: an anatomical study]. Prog Urol 20: 515-519.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.