Current Concepts Review: The Key to Anatomic Reconstruction of the Anterior Cruciate Ligament: The Resident’s Ridge, Lateral Intercondylar Ridge – Fu’s Ridge
by Rui W Soares, Jose F Vega, Lutul D Farrow*
Department of Orthopaedic Surgery, Cleveland Clinic Foundation, USA
*Corresponding author: Lutul Dashaun Farrow, Cleveland Clinic Orthopaedic and Rheumatologic Institute, Cleveland Clinic Sports Health Center, 5555 Transportation Boulevard, Garfield Heights, OH 44125, USA.
Received Date: 02 February, 2025
Accepted Date: 11 February, 2025
Published Date: 14 February, 2025
Citation: Soares RW, Vega JF, Farrow LD (2025) Current Concepts Review: The Key to Anatomic Reconstruction of the Anterior Cruciate Ligament: The Resident’s Ridge, Lateral Intercondylar Ridge – Fu’s Ridge. J Orthop Res Ther 10: 1377. https://doi.org/10.29011/2575-8241.001377
Abstract
Techniques in arthroscopic knee surgery and anterior cruciate ligament (ACL) reconstruction have steadily progressed as advancements in research and patient reported outcomes become more available. Biomechanical and cadaveric anatomical studies have laid the foundation and guide surgeons with surgical techniques. Specifically, investigation of osseous landmarks has provided a blueprint in accurate femoral and tibial tunnel placement to recreate the native ACL anatomy in ACL reconstructive surgery. “Resident’s ridge,” or the lateral intercondylar ridge, and the lateral bifurcate ridge have been identified as important landmarks for femoral tunnel placement. The aim of this study was to review the current concepts and evolution of the lateral intercondylar ridge and the lateral bifurcate ridge’s importance in anatomic ACL reconstruction.
Keywords: Anterior cruciate ligament, lateral intercondylar ridge, bifurcate ridge, resident’s ridge, knee, arthroscopy
Introduction
ACL injuries are the most common ligamentous injury with incidence of approximately 100,000 to 200,0000 cases reported annually [1]. Through this, the anatomy of the anterior cruciate ligament (ACL) has been extensively studied over the last two decades, [2-4] and surgical techniques with outcomes have been a focus of ongoing research [2,5-8]. As the biomechanics and anatomy of the ACL become better understood, an anatomic approach to ACL reconstruction has become a staple in surgery [9]. Furthermore, graft failure has been identified as a wellestablished complication, and prior literature has reported less than 50% of athletes return to their previous level of functioning following reconstruction [10,11]. Graft failure is most commonly caused by incorrect femoral tunnel placement during “anatomic” ACL reconstruction [11]. As a result, a deeper understanding of accurate femoral tunnel placement has been recognized by many surgeons.
The term “Resident’s ridge” was first described by Dr. Clancy after orthopaedic residents inadequately debrided the posterior aspect of the lateral femoral condyle when in fact, they were looking at the “resident’s ridge [12].” The “resident’s ridge” is defined as the vertical to transverse ridge that is about 75% posterior from the anterior aspect of the lateral femoral condyle when knee is flexed to 90° [12,13]. Regardless, various techniques for ACL reconstruction have evolved over the last two decades which have included extra-articular and intra-articular procedures relying on this anatomic structure to restore “native” anatomy [3].
Anatomy and Histology
The ACL is made up of type I collagen fibers [6,9,13], and is a main resistor to anterior tibial translation and rotational loads [3,14]. Briefly, the ACL consists of two bundles, posterolateral and anteromedial both of which originate on the posteromedial surface of the lateral femoral condyle just anterior to tibial eminence [3]. On the tibial side, as the name implies, the anteromedial bundle inserts slightly anterior while the posterolateral bundle inserts slightly posterior. According to various cadaveric and biomechanical studies, the mean length of the posterolateral bundle is 18mm and 33mm for the anteromedial bundle [13,15,16]. Biomechanically, the ACL provides a crucial role in joint stability and is the primary restraint to anterior translation of the tibia relative to the femur [9]. Additionally, when the knee joint is in full extension, the ACL functions as a major secondary restraint to internal rotation [17]. Specifically, the anteromedial resists anterior tibial translation while the posterolateral resists rotational loads [18]. Furthermore, the ACL serves as a minor secondary restraint to external rotation and varus-valgus angulation especially while weightbearing [17]. This function can be tested with a well-known clinical exam, the pivot shift,” which involves a combined internal tibial and valgus torque while ranging the lower extremity from flexion-extension [17].
The femoral ACL insertion covers a large portion of the intercondylar notch, extending posterior from the lateral intercondylar ridge to the articular surface5. One of the hallmarks and foundational studies by Girgis et al. [19], showed that the ACL was found to be attached to the posterior aspect of the medial surface of the lateral femoral condyle. This semi-circular attachment noted in the figure below (Figure 1) determined the first insight to an anterior border. This position was deemed with a straight and a convex posterior side that was oriented in an oblique direction from vertical. This is one of the first studies to mention a straight anterior border which will conventionally be known today as the lateral intercondylar ridge.
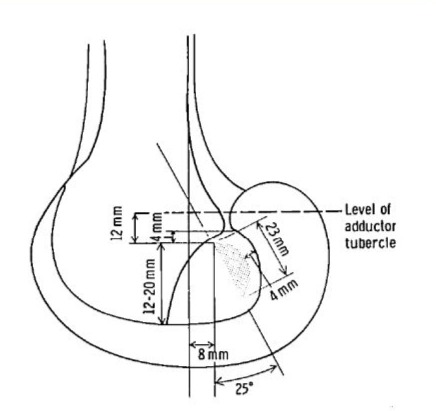
Figure 1: Early representation of the medial surface of the right lateral femoral condyle showing average measurements and bony relations of the ACL femoral attachment. Adapted with permission from Girgis et al. [19].
Hutchinson and Ash [12] better delineated the anatomy of the resident’s ridge by obtaining 10 cadaveric distal femurs to better evaluate for cortical thickness at distinct sites, slope, and the ACL attachment site. They found that 9 out of 10 specimens had a resident’s ridge. Posterior to this ridge the lateral wall of the intercondylar notch had a change in slope (Figure 2) and a change in mean cortical thickness at the ACL attachment site of 1.6mm. They found that this was thicker than at the cartilage-intercondylar notch junction (mean 0.96 mm), a point midway between the ACL attachment and the cartilage-intercondylar notch junction (mean, 0.9 mm), and resident’s ridge (mean 0.90mm). Consequently, they concluded that resident’s ridge is accounted for by a distinct change in slope of the femoral notch roof (anterior to the femoral attachment of the ACL). This important concept will be revisited throughout this paper.
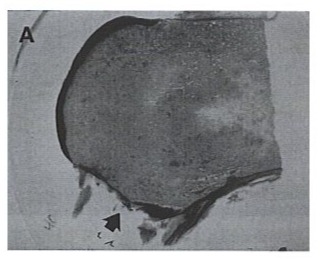
Figure 2: Histological cross-sectional sagittal section of distal femur cadaveric specimen. The arrow denotes the change in slope of the notch roof correlating with the resident’s ridge. Adapted with permission from Hutchinson et al. [12].
In a cadaveric anatomic study conducted by Farrow et al. [20] evaluating the anatomy of 200 skeletally mature specimens, they found the presence of a “residents ridge” in 196/200 cases. Furthermore, the authors proposed that this ridge should be renamed as the “lateral intercondylar ridge” (Figure 3) based on the anatomic location as it represents the anterior border of the femoral attachment of the ACL.
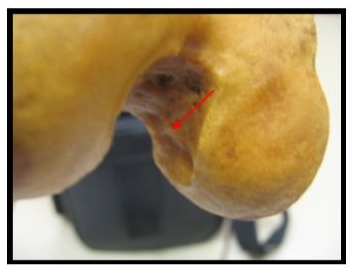
Figure 3: This is an axial view of the intercondylar notch of a left femur. The lateral intercondylar ridge is depicted in the red arrow. Adapted with permission from Farrow et al. [20].
Having expanded on the work from Hutchinson and Ashe, Ferretti et al. [3] determined qualitative and quantitative osseous landmarks of the ACL femoral attachment site. Seven human fetuses, sixty patients who underwent arthroscopically assisted ACL reconstructions, and sixteen cadaveric knees were included in the study. They determined that two osseous landmarks: one that runs from proximal to distal was present in all arthroscopic and cadaveric patients, named the lateral intercondylar ridge and another osseous landmark between the femoral attachment of the anteromedial and posteromedial bundles termed the lateral bifurcate ridge (Figure 4). They also found a change of slope that was observed in all specimens studied between the femoral attachment of the posterolateral and anteromedial bundles. This study paved the way for better topographical placement of femoral tunnels during surgery and helped surgeons better perform anatomic ACL reconstruction surgery.
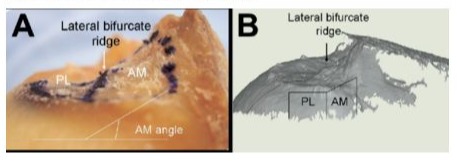
Figure 4: Gross cadaveric (A) and 3-dimentional (3D) (B) representation of the change in slope at the ACL femoral attachment. (A) White line demonstrates the angle formed between the anteromedial and posterolateral femoral attachments with noted lateral bifurcate ridge. (B) Topographic 3D representation of the ACL femoral attachment with depicted change in slope. Adapted with permission from Ferretti et al. [3].
Further histologic and advanced imaging studies were also performed to better delineate the previous studies. Iwahashi et. Al [18], histologically identified the direct and indirect insertion of the femoral ACL insertion while quantitatively measuring the direct femoral insertion area by use of 3-dimentional (3D) volume rendered CT scan. Eight cadaveric knees were used, and CT was used to obtain 3D volume rendered images of the femur then the lateral femoral condyle including the ACL femoral attachment were sectioned histologically (Figure 5). They found that the direct ACL insertion was microscopically identified at the region between the linear bony ridge (known as the lateral intercondylar ridge) 7-10 mm anterior to the articular cartilage margin and the posteromedial articular cartilage margin of the lateral femoral condyle (Figure 6).
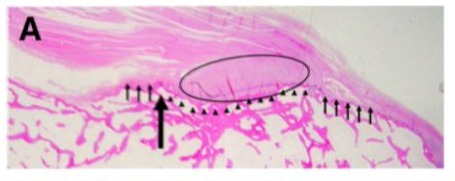
Figure 5: Oblique axial plane histologic image (parallel to roof of notch). Bony prominence is confirmed with large arrow adjacent to anterior border of concave area (depicted by arrowheads).
Central dense collagenous fibers are depicted by the oval and they can be seen inserting into the concave area behind bony ridge. The small arrows depict the course fibrous region which is surrounded by the central dense collagenous ACL fibers and attached to bone around the concavity and bony ridge. Adapted with permission from Iwahashi et al. [18].
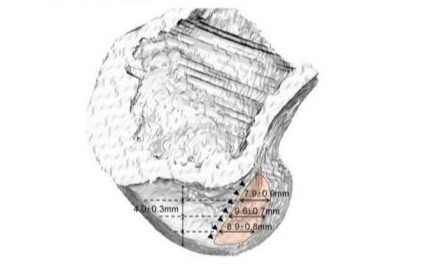
Figure 6: Arrowheads showing residents ridge located proximaldistal along entire ACL attachment through a 3D virtual reality CT model of the lateral femoral condyle. Adapted with permission from Iwahashi et al. [18].
Further histologic and macroscopic studies have determined the femoral insertion of the ACL. Sasaki et al. [21] included 20 cadavers which were observed macroscopically, histologically, and immune histologically (staining for type I and II collagen). They found that in 16 knees the femoral insertion was oval and the proximal ACL fibers spread in a fanlike manner on the medial aspect of the lateral femoral condyle. Importantly, microscopically, the insertion was located just posterior to the lateral intercondylar ridge and was divided into direct and indirect insertions. The direct insertion did not continue to the posterior cartilage and the indirect insertion was posterior to the direct insertion (Figure 7). Another bony ridge was found at posterior margin of the direct insertion. This bony ridge was termed the lateral posterior ridge. This study further showed the anatomical significance of the lateral intercondylar ridge (Figure 8).
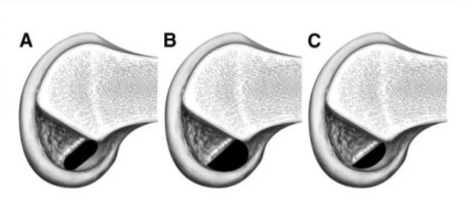
Figure 7: Variations of ACL femoral insertions denoting a narrow short axis on A (ACL insertion narrow between posterior cartilage and ACL insertion), a semi-circular shape in B (ACL insertion located between posterior cartilage and lateral intercondylar ridge), a small semi-circular shape (ACL insertion was wide and separated from posterior cartilage). Adapted with permission from Sasaki et al. [21].
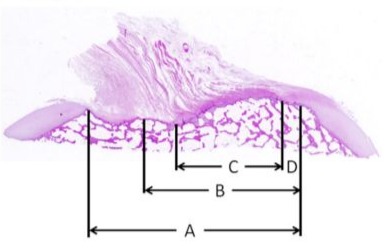
Figure 8: This is a histologic image of the ACL femoral insertion with (A) denoting the distance from anterior to posterior cartilage border. (B) is the distance from the lateral intercondylar ridge to the posterior cartilage border. (C) is the width of the direct insertion and (D) is the distance from the direct insertion to posterior cartilage border. Adapted with permission from Sasaki et al. [21].
This anatomic relationship allows surgeons to determine appropriate placement of a typical 8-10mm femoral tunnel to restore knee stability. Furthermore, these landmarks are important for the correct placement of both the femoral and tibial tunnel [22]. Specifically, the lateral intercondylar ridge demarcates the anterior border of the ACL footprint and serves as a reference for drill placement [20]. In addition, Ferretti et al. [3] identified the existence of the lateral bifurcate ridge which runs from anterior to posterior and separates the anteromedial and posterolateral bundles of the ACL at the femoral attachment site landmark.
Radiographic Anatomy
Multiple radiographic and advanced imaging studies have been performed to better delineate the bony landmarks of the ACL origin and insertion. Farrow et al. [14] identified 20 lateral distal femora radiographic images to determine the length of Blumensaat’s line and the distance of the anterior extent of Blumensaat’s line to the point where the lateral intercondylar ridge intersects Blumensaat’s line. They determined that the lateral intercondylar ridge intersects Blumensaat’s line at a point defined by multiplying Blumensaat’s line length by 0.79. At this point, the ridge runs at a 75.5 angle with respect to Blumensaats. Consequently, using this method may help determine, through radiographs, if revision surgery can be performed in a “single stage” without the need of increased radiation exposure from computed tomography (CT) scanning (Figure 9). This further corroborates the use of radiographic and advanced imaging techniques to better determine and confirm accurate tunnel placement prior to ACL reconstruction.
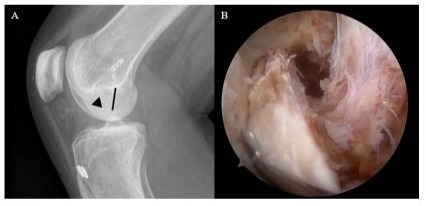
Figure 9: (A) Lateral Radiograph of a right knee of a 19-yearold female patient demonstrating the location of the lateral intercondylar ridge (black line) based on Blumensaat’s RidgeRatio. The existing femoral tunnel (arrowhead) is anterior to the ridge indicating sufficient space posterior to the ridge for anatomic ACL reconstruction. (B) Arthroscopic view of the femoral tunnel in a revision ACL surgery in which a 10 mm tunnel was able to be drilled posteriorly in relation to the prior primary ACL femoral tunnel.
Recent studies looking at the anatomy of the intercondylar notch and lateral intercondylar wall through CT knee images have further characterized bony relationships. Li et al. [11] identified 89 patients with CT images of the knee joint observing full lateral views of the lateral femoral condyle and evaluated for the presence of a lateral intercondylar ridge. The area and height of the lateral intercondylar wall and length of Blumensaat’s line were calculated. They found that the lateral intercondylar ridge demonstrated 3 types of morphological variations. These morphological variations included the no ridge (20 knees), the ridge type or one ridge (23 knees), and the plateau type or two ridges (46 knees). There were significant differences in Blumensaat line length, notch height, lateral notch area, and denser bone among the three morphological variations. Importantly, there was an anterior margin line that was denoted on the denser bone area on the lateral intercondylar wall that was found on the ridge and plateau types (Figure 10).
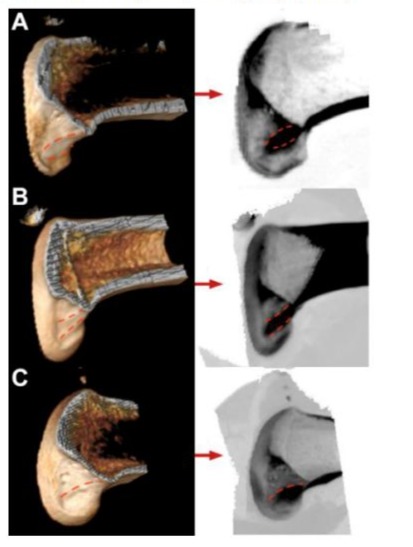
Figure 10: Left sided images show the location of the lateral intercondylar ridges on 3D CT images for the varying ridge types (plateau type and ridge type). The right sided images demonstrate the area of denser bone on maximum intensity projection. (A) posterior ridge located anterior, (B) posterior to posterior margin and (C) All 23 knees with lateral intercondylar ridges (one ridge) in this study corresponded to an anterior margin of denser bone. Adapted with permission from Li et al. [11].
Other advanced imaging studies have looked at femoral tunnel preparation during ACL reconstruction using 3D models. Laverdiere et al. [23] used 3D printed models to determine osseous landmarks and the ACL footprint and comparing these models with intraoperative placement. 3D printed models were obtained from 20 patient and 12 fellowship trained sports orthopedic surgeons identified the femoral landmark and ACL footprint. They found that none of the surgeons were able to identify the bony ridges such as the junction of the intercondylar and bifurcate ridges on the 3D models. Interestingly, operatively placed tunnels were more accurate noting the importance of soft tissue landmarks through arthroscopic visualization in ACL footprint localization intraoperatively. In comparison, Laverdiere et al. [24] reported on the ability of thirteen residents in identifying the native ACL footprint and the femoral bony landmarks from real patient 3D models. Thirteen residents began with teaching sessions in properly identifying anatomical bony landmarks and appropriate ACL positioning. Interestingly, there was no significant difference before or after the teaching sessions in identification of either the intersection of the bifurcate and intercondylar ridges or the center of the femoral footprint. These results show that formal teaching sessions with hands on sessions have no direct impact on identifying the femoral ACL footprint or bony landmarks.
Magnetic resonance imaging (MRI) has also been used to better determine ACL femoral condyle anatomy. Tanaka et al. [25] evaluated the course of the anteromedial and posterolateral bundles using coronal oblique images. They studied 81 knees with intact ACLs and obtained the oblique images with the knee in extension understanding the course of the ligament and analyzing the femoral attachment/geometry of the lateral femoral condyle inner wall. They found that the resident’s ridge was found in 91% of knee in the anteromedial bundle image whereas it was only visualized in only 17% of knees in the posterolateral bundle image. They concluded that the anteromedial was confluent with the apex of the intercondylar ridge along with the ability to denote femoral condyle osseous landmarks.
Femoral Tunnel Placement
Through all of the radiographic, histologic, and anatomical representations depicted, accurate tunnel placement arthroscopically is crucial in ACL reconstructive surgery. Foundationally, Aglietti et. Al [26] discuss the importance of the accuracy in tunnel positioning as essential for success in ACL surgery. Specifically, their study reviews 89 arthroscopically assisted patellar tendon ACL reconstructions for chronic isolated injuries with an average of 7 years follow up. They showed that misplacement of the intraarticular exit of the femoral tunnel was misplaced in the anterior 50% of the condyles along the superior aspect of the notch in 10% of knees. This positioning was determined to significantly increase graft failure in 62.5% of cases as compared with placement more posteriorly (12% failure).
Zauleck et al. [22] conducted a cadaveric study to evaluate the discernibility of the lateral bifurcate ridge and the lateral intercondylar ridge during ACL femoral tunnel placement. Cadaveric models were divided into two groups (group A and group B), and a coordinate system was used to measure dimensions, position, and orientation of the femoral footprint of the ACL. The authors found that the lateral bifurcate ridge was found in 24.7 and 13.2% in group A and B, respectively. Additionally, the angles and shapes of the osseous landmarks situated near Blumensaat’s line were highly variable. Conversely, the lateral intercondylar ridge was found in 97.9% and 85.3% of specimens in group A and B, respectively. Based on the findings of the study, the lateral bifurcate ridge was determined to be an unreliable intraoperative landmark for femoral tunnel placement during arthroscopic ACL reconstructions due to the low prevalence.
In another investigation, Iriuchishima et al. [27] detail a cadaveric study observing the morphological correlation between the lateral wall of the femoral intercondylar notch and Blumensaat’s line. Forty-one cadaveric knees (23 females, 18 males; median age 83 years) were included in the study, and three-dimensional computed tomographic knee imaging (3D CT) was performed with resident’s ridge (lateral intercondylar ridge) noted on axial CT imaging. The length of the superior aspect of the ridge was measured to the most anterior, middle, and posterior border of cortical thickness along with the distance to the posterior femoral condylar line. The author then categorized the morphology of Blumensaat’s line into small or large hill types. In all cadaveric knees, increased cortical thickness was identified on the lateral wall of the femoral intercondylar notch, and the residents ridge had significant correlation with hill location on Blumensaat’s line. This study found a continuation of cortical bone from the posterior cortex of the femoral shaft via the hilltop of Blumensaat’s line to the lateral wall cortical thickness of the femoral intercondylar notch. In effect, the hilltop location on Blumensaat’s line with relation to resident’s ridge distinguishes an important new bony landmark in ACL reconstructive surgery.
Shino et al. [28] establish a technique to arthroscopically identify resident’s ridge without bony notchplasty and in patients with chronic ACL insufficiency and to elucidate proper anatomical femoral tunnel ACL graft placement. Fifty consecutive patients undergoing arthroscopic ACL reconstructions were included. If the ridge was found soft tissue was removed with radiofrequency energy and a socket (Figure 11) with a rectangular aperture of 5x10mm was created just posterior to the ridge. At 3-4 weeks after surgery, 3D CT was used to identify the location of the ridge and socket was used as reference point. Arthroscopically, the linear ridge was seen consistently running from superior-anterior to inferior-posterior on lateral notch wall typically observed 7-10mm anterior to the posterior articular margin. 3D CT further confirmed the arthroscopically identified ridge ad resident’s ridge. This study has served as a hallmark study in showing the ridge as a useful landmark in anatomic femoral arthroscopic tunnel placement during ACL reconstruction.
Subsequently, Ziegler et al. [29], quantified the anteromedial and posterolateral bundles centers with respect to pertinent bony and soft tissue landmarks using a radio-frequency tracking device. Eleven cadaveric knees were studied, and they showed that the femoral attachment center was 1.7 mm proximal to the lateral bifurcate ridge and 6.1mm posterior to the lateral intercondylar ridge. Specifically, the femoral anteromedial attachment center was 4.8 mm proximal to bifurcate edge and 7.1mm posterior to the ridge. The femoral posterolateral bundle center was found to be 5.2 mm distal to the bifurcate ridge and 3.6mm posterior to the ridge. The authors concluded that understanding these discrepancies may enhance arthroscopic femoral tunnel placement during single or double bundle reconstruction through more anatomic graft placement.
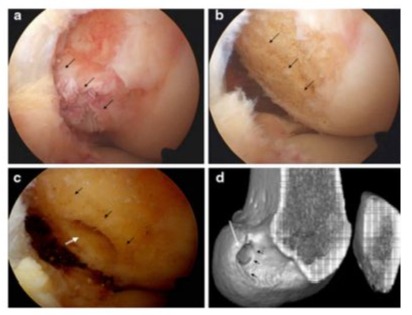
Figure 11: (A) Arthroscopic view of an 18-year-old male left ACL femoral stump sustaining injury 16 days prior. This is an anteromedial portal view. (B) Clearage of the remnant stump with black arrows depicting ridge which is 9mm anterior to the posterior articular cartilage margin. (C) White arrow depicts the rectangular aperture of the femoral socket behind the black arrows showing the ridge. (D) 3D CT representation of ridge (black arrows) and socket behind the ridge (white arrow). Adapted with permission from Shino et al. [28].
In a retrospective case series, Rowan et al. [1] further discusses the accurate placement of the femoral tunnel and emphasizes its clinical success in ACL reconstruction. The authors included 80 patients (24 female, 56 male) with anatomic single bundle ACL reconstruction. Intraoperative arthroscopic images and operative reports were examined, and placement was confirmed by review of lateral radiographs using both the quadrant method and Blumensaat-ridge ratio. The authors concluded that, using the quadrant method, all femoral tunnels were placed anatomically, and the lateral intercondylar ridge and lateral bifurcate ridge were reliable landmarks for anatomic ACL placement of femoral tunnel. Conversely, Laverdier et al. [23] conducted a 3D model study identifying the ACL femoral ridges landmark and optimal tunnel placement. Twelve sports fellowship-trained orthopedic surgeons were asked to identify femoral landmarks on an ACL footprint on 10 different 3D printed knees with none of the surgeons able to consistently identify the junction of the bony ridges. Interestingly, the magnitude of error was 3.72 + 2.43 mm from actual surgery performed compared to 5.82+1.97 on the 3D models. They conclude that operatively placed (i.e arthroscopically or looking for soft tissue landmarks) tunnels (Figure 12) were more accurate than using 3D models to correctly identify the junction of the intercondylar and bifurcate ridges and the native ACL footprint.
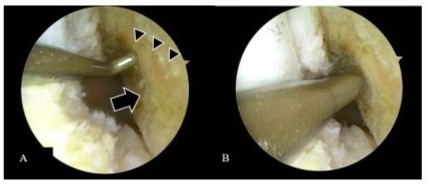
Figure 12: (A) Arthroscopic view of lateral intercondylar ridge (arrowheads) and lateral bifurcate ridge (block arrow) of a 33-yearold male patient demonstrated using a prob. (B) Arthroscopic view of awl being used to denote and set reference point for femoral tunnel drill placement in order to establish appropriate anatomical placement of graft adjacent to lateral intercondylar ridge. Adapted with permission from Laverdier et al. [23].
Furthermore, the question of the lateral intercondylar ridge being present in acute versus chronic ACL tears has also been studied. Van Eck et al. [30] report on 25 chronic ACL injured patients and compared them to 25 acute ACL matched for gender and age. Using a scoring system, the lateral intercondylar ridge and lateral bifurcate ridge were deemed as present, absent or indeterminate due to insufficient visualization. They found that the lateral intercondylar ridge was seen in 88% of subacute patients and 88% of chronically torn patients. The lateral bifurcate ridge was seen in 48% of subacute and chronically torn ACLs. They concluded that when assessing for a lateral intercondylar ridge there was no difference between acute and chronic ACL injuries. The lateral intercondylar ridge should remain as the femoral osseous landmark during arthroscopic ACL reconstruction regardless of injury time [31].
Bhattacharyya et al. [32] detail a study to further evaluate the lateral intercondylar ridge as a reliable landmark to minimize errors in femoral tunnel placement during ACL reconstruction. In this twostage study, 23 femoral dry bone specimens were first examined using a digital microscribe to evaluate a bony ridge on the medial surface of the lateral femoral condyle. In phase 2, the femoral ACL insertion of seven cadaveric specimens were identified using 3D reconstruction of the lateral intercondylar ridge. The authors found that all specimens had a defined lateral intercondylar ridge, and the ridge was consistently noted to be located just anterior to the femoral insertion. Specifically, they identified that the ACL footprint was present in the depression between the inferior articular margin and the ridge with a mean distance of 10.1mm between this midpoint. This was the first study to use a microscribe to reconstruct the medial surface of the lateral femoral condyle and demonstrated that the lateral intercondylar ridge was a consistent anatomic structure that defines the anterior margin of the femoral ACL insertion.
Furthermore, it is important to consider the pediatric population when assessing femoral tunnel placement during arthroscopic ACL reconstruction. Liu et al. [33] present 103 preserved femora aged 3 to 20 years old (33 femurs were aged 7-20 years of age). Distance between the resident’s ridge and the “over the top” position were measured, along with the angles between the femoral surface, distal femoral physics, and femoral shaft on the coronal and sagittal planes. They showed that femurs from the 13- to 15-yearold subgroup had clearly defined resident’s ridge than younger subgroups. Furthermore, it was noted that the average angles between femoral surface and physics in the coronal and sagittal planes were noted to be 58 and 28 degrees in the 10- to 12-yearold group and 47 and 36 degrees in the 13- to 15-year-old group. Additionally, the average angles between the distal femoral shaft and the physics in the coronal and sagittal planes were calculated at -6 and 7 degrees in the 10- to 12-year-old subgroup and -9 and 7 degrees in the 13- to 15-year-old group. Analysing gender differences, male had larger distances between resident’s ridge and the over-the-top position in males but no angular measurement differences. They concluded that in younger patients the resident’s ridge is less commonly present and less apparent. Consequently, in both males and females tunnel position should be aimed medial and posterior with respect to the perpendicular of the femoral surface and medial and anterior with respect to the shaft to drill though the physis with less obliquity. Additionally, further studies by Wu et al. [34] have also shown that there was no correlation between the ACL femoral footprint size (lateral intercondylar ridge length) and gender or footprint size and height.
Lastly, substantial attention has also been implemented to establish accurate tibial tunnel positioning [4,5,7,31,35-37]. The ACL fibers attach to a fossa located anterior and lateral to the medial tibial spine [6,9]. The fossa itself is approximately 11mm wide and 17mm in the antero-posterior direction [6,15,38]. In addition, the ACL sends a variable number of fibres anteriorly beneath the transverse intermeniscal ligament with some extensions blending with the attachment of the anterior or posterior horn of the lateral meniscus [6]. As a result of its broad extensions, the tibial attachment may be wider and stronger than the femoral attachment site described above. This anatomic relationship is taken into consideration when assessing the impossibility of recreating the ACL’s C shaped insertion around the lateral meniscus anterior root with a single transtibial cylindrical tunnel [35].
Conclusion
Advances in ACL reconstruction have been well documented over the last two decades. The early work of Dr. Clancy to identify “resident’s ridge” or the lateral intercondylar ridge, has laid the framework for subsequent research to characterize anatomic relationships in the ACL. With improved technology, osseous landmarks continue to be better defined and provide surgeons with a guide when re-establishing “native” anatomy in ACL reconstruction. Consequently, new data has further delineated the importance of the lateral intercondylar ridge and lateral bifurcate ridge.
Farrow et al. [20] also concurred with Hutchinson and Ash [12], based on the research that has been conducted, the lateral intercondylar ridge represents the anterior border of the femoral attachment of the ACL. This has allowed surgeons to better assess appropriate femoral tunnel placement as improper femoral tunnel placement is a common error in ACL reconstructive surgery. Prior to these studies, surgeons would oftentimes remove the lateral intercondylar ridge during notchplasty which a staple in ACL reconstruction in the past was. Fu et al. [39] detail sixty arthroscopic dissections in which they consistently mark the anterior border with knee in extension and superior border with knee in 90° flexion as the lateral intercondylar ridge. They also detail the discovery of another osseous ridge labeled, “the lateral bifurcate ridge,” as the ridge separating the anteromedial and posteromedial bundles of the ACL during reconstruction. This ridge is now used as an anatomic landmark to guide placement of individual posterolateral and anteromedial bundle placement during ACL reconstruction.
The lateral intercondylar ridge continues to be studied to this day and remains a consistent anatomical structure that defines the anterior margin of the femoral ACL insertion. A more recent study by Li et al. [11] in 2022 has shown there may be morphologic variations within the lateral intercondylar ridge. They found that in 46 out of 89 cadaveric femurs there were 2 ridges with a plateau between them. Another finding showed that the lateral notch area, Blumensaat line length, notch height was significantly different among lateral intercondylar ridge types. Furthermore, it was seen that the presence of such variations may affect measurement accuracy during evaluation of ACL tunnel position while using the lateral intercondylar ridge as a landmark during ACL reconstruction.
The early work that was researched by Dr. Clancy, Farrow et al., Fu et al., and Hutchinson and Ash have paved the way to better determine femoral tunnel placement and have guided surgeons for better native anatomical ACL graft placement. Successful femoral tunnel placement is integral in ACL reconstruction. Many studies have shown that the lateral intercondylar ridge continues to be an integral osseous landmark and represents a part of the functional footprint of the ACL. Further studies continue to evaluate osseous landmarks as patients may represent various anatomical variants.
Acknowledgement
This article is dedicated to Dr. Freddie Fu, whose countless dedication and innovation to the field of orthopedics, enthusiasm, and energy have been palpable for decades. We thank all of his contribution and his research and drive will forever be a part of the orthopedic field.
Level of Evidence: Level V, review article
Conflict of Interest
Rui W Soares, MD, Jose Vega, MD, and Lutul D Farrow, MD have no disclosures.
References
- Rowan FA, Marshall T, Gombosh MR, Farrow LD (2017) Utilization of Osseous Landmarks for Anatomic Anterior Cruciate Ligament Femoral Tunnel Placement. J Knee Surg 30(4): 359-363.
- Ferretti M, Ekdahl M, Shen W, Fu FH (2007) Osseous Landmarks of the Femoral Attachment of the Anterior Cruciate Ligament: An Anatomic Study. Arthroscopy - Journal of Arthroscopic and Related Surgery 23(11): 1218-1225.
- Hara K, Mochizuki T, Sekiya I, Yamaguchi K, Akita K, Muneta T (2009) Anatomy of normal human anterior cruciate ligament attachments evaluated by divided small bundles. American Journal of Sports Medicine 37(12): 2386-2391.
- Tensho K, Shimodaira H, Aoki T, Naritha N, Kato H, et al. (2014) Bony landmarks of the anterior cruciate ligament tibial footprint: A detailed analysis comparing 3-dimensional computed tomography images to visual and histological evaluations. American Journal of Sports Medicine 42(6):1433-1440.
- Angelini FJ, Albuquerque RFM, Sasaki SU, Camanho GL, Hernandez AJ (2010) Comparative study on anterior cruciate ligament reconstruction: Determination of isometric points with and without navigation. Clinics 65(7): 683-688.
- Duthon VB, Barea C, Abrassart S, Fasel JH, Fritschy D, Ménétrey J (2006) Anatomy of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 14(3): 204-213.
- Musahl V, Plakseychuk A, VanScyoc A, Sasaki T, Debski RE, et al. (2005) Varying femoral tunnels between the anatomical footprint and isometric positions: Effect on kinematics of the anterior cruciate ligaments-reconstructed knee. American Journal of Sports Medicine 33(5): 712-718.
- Zantop T, Diermann N, Schumacher T, Schanz S, Fu FH, Petersen W (2008) Anatomical and non-anatomical double-bundle anterior cruciate ligament reconstruction: Importance of femoral tunnel location on knee kinematics. American Journal of Sports Medicine 36(4): 678-685.
- Siegel L, Vandenakker-Albanese C, Siegel D (2012) Anterior cruciate ligament injuries: Anatomy, physiology, biomechanics, and management. Clinical Journal of Sport Medicine 22(4): 349-355.
- Ardern CL, Taylor NF, Feller JA, Webster KE (2011) Return-toSport Outcomes at 2 to 7 Years After Anterior Cruciate Ligament Reconstruction Surgery 40(1): 41-48.
- Li Z, Zhang W, Ren S, et al. (2022) Relationship Between Number of Lateral Intercondylar Ridges and Area of Denser Bone on the Lateral Intercondylar Wall. Orthop J Sports Med 10(5): 23259671221091332.
- Hutchinson MR, Ash SA (2003) Resident’s ridge: assessing the cortical thickness of the lateral wall and roof of the intercondylar notch. Arthroscopy 19(9): 931-935.
- Giuliani JR, Kilcoyne KG, Rue JPH (2009) Anterior cruciate ligament anatomy: a review of the anteromedial and posterolateral bundles. J Knee Surg 22(2): 148-154.
- Farrow LD, Gillespie RJ, Victoroff BN, Cooperman DR (2008) Radiographic location of the lateral intercondylar ridge: its relationship to Blumensaat’s line. Am J Sports Med 36(10): 2002-2006.
- Schillhammer CK, Reid JB, Rister J, Jani SS, Marvil SC, et al. (2016) Arthroscopy up to date: Anterior cruciate ligament anatomy. Arthroscopy - Journal of Arthroscopic and Related Surgery 32(1): 209212.
- Zantop T, Petersen W, Sekiya JK, Musahl V, Fu FH (2006) Anterior cruciate ligament anatomy and function relating to anatomical reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy 14(10): 982-992.
- Markatos K, Kaseta MK, Lallos SN, Korres DS, Efstathopoulos N (2013) The anatomy of the ACL and its importance in ACL reconstruction. European Journal of Orthopaedic Surgery and Traumatology 23(7): 747-752.
- Iwahashi T, Shino K, Nakata K, Otsubo H, Suzuki T, et al. (2010) Direct anterior cruciate ligament insertion to the femur assessed by histology and 3-dimensional volume-rendered computed tomography. Arthroscopy - Journal of Arthroscopic and Related Surgery 26(9 SUPPL 1): S13-S20.
- Girgis FG, Marshall JL, Al Monajem AR (1975) The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res 106(106): 216-231.
- Farrow LD, Chen MR, Cooperman DR, Victoroff BN, Goodfellow DB (2007) Morphology of the femoral intercondylar notch. J Bone Joint Surg Am 89(10): 2150-2155.
- Sasaki N, Ishibashi Y, Tsuda E, Yuji Yamamoto, Shugo Maeda, et al. (2012) The femoral insertion of the anterior cruciate ligament: discrepancy between macroscopic and histological observations. Arthroscopy 28(8): 1135-1146.
- Zauleck MK, Gabriel S, Fischmeister MF, Hirtler L (2014) Origin of the anterior cruciate ligament and the surrounding osseous landmarks of the femur. Clin Anat 27(7): 1103-1110.
- Laverdiere C, Schupbach D, Schupbach J, et al. (2020) Can Surgeons Identify ACL Femoral Ridges Landmark and Optimal Tunnel Position? A 3D Model Study. Arthrosc Sports Med Rehabil 2(4): e361-e368.
- Laverdiere C, Harvey E, Schupbach J, Boily M, Burman M, Martineau PA (2020) Effect of Teaching Session on Resident Ability to Identify Anatomic Landmarks and Anterior Cruciate Ligament Footprint: A Study Using 3-Dimensional Modeling. Orthop J Sports Med 8(3): 2325967120905795.
- Tanaka Y, Shiozaki Y, Yonetani Y, Kanamoto T, Tsujii A, Horibe S (2011) MRI analysis of the attachment of the anteromedial and posterolateral bundles of anterior cruciate ligament using coronal oblique images. Knee Surg Sports Traumatol Arthrosc 19 Suppl 1: S54-59.
- Aglietti P, Buzzi R, Giron F, Simeone AJV, Zaccherotti G (1997) Arthroscopic-assisted anterior cruciate ligament reconstruction with the central third patellar tendon. A 5-8-year follow-up. Knee Surg Sports Traumatol Arthrosc 5(3): 138-144.
- Iriuchishima T, Suruga M, Yahagi Y, Iwama G, Aizawa S (2020) Morphology of the resident’s ridge, and the cortical thickness in the lateral wall of the femoral intercondylar notch correlate with the morphological variations of the Blumensaat’s line. Knee Surg Sports Traumatol Arthrosc 28(8): 2668-2674.
- Shino K, Suzuki T, Iwahashi T, Tatsuo Mae, Norimasa Nakamura, et al. (2010) The resident’s ridge as an arthroscopic landmark for anatomical femoral tunnel drilling in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 18(9): 1164-1168.
- Ziegler CG, Pietrini SD, Westerhaus BD, Colin J Anderson, Coen A Wijdicks, et al. (2011) Arthroscopically pertinent landmarks for tunnel positioning in single-bundle and double-bundle anterior cruciate ligament reconstructions. Am J Sports Med 39(4): 743-752.
- van Eck CF, Morse KR, Lesniak BP, Eric J Kropf, Michael J Tranovich, et al. (2010) Does the lateral intercondylar ridge disappear in ACL deficient patients? Knee Surg Sports Traumatol Arthrosc 18(9): 11841188.
- Sirleo L, Innocenti M, Innocenti M, Civinini R, Carulli C, Matassi F (2018) Post-operative 3D CT feedback improves accuracy and precision in the learning curve of anatomic ACL femoral tunnel placement. Knee Surgery, Sports Traumatology, Arthroscopy 26(2): 468-477.
- Bhattacharyya R, Ker A, Fogg Q, Spencer SJ, Joseph J (2018) Lateral Intercondylar Ridge: Is it a reliable landmark for femoral ACL insertion?: An anatomical study. Int J Surg 50: 55-59.
- Liu RW, Farrow LD, Messerschmitt PJ, Gilmore A, Goodfellow DB, Cooperman DR (2008) An anatomical study of the pediatric intercondylar notch. J Pediatr Orthop 28(2): 177-183.
- Wu E, Chen M, Cooperman D, Victoroff B, Goodfellow D, Farrow LD (2011) No correlation of height or gender with anterior cruciate ligament footprint size. J Knee Surg 24(1): 39-43.
- Borque KA, Laughlin MS, Pinheiro VH, Jones M, Williams A (2023) Rebranding the ‘anatomic’ ACL reconstruction: Current concepts. Journal of ISAKOS 8(1): 23-28.
- Hoshino Y, Kim D, Fu FH (2012) Three-dimensional anatomic evaluation of the anterior cruciate ligament for planning reconstruction. Anat Res Int 2012:1-5.
- Xerogeanes JW, Hammond KE, Todd DC (2012) Anatomic landmarks utilized for physeal-sparing, anatomic anterior cruciate ligament reconstruction: An MRI-based study. Journal of Bone and Joint Surgery 94(3): 268-276.
- Tsukada S, Fujishiro H, Watanabe K, Akimoto Nimura, Tomoyuki Mochizuki, et al. (2014) Anatomic variations of the lateral intercondylar ridge: Relationship to the anterior margin of the anterior cruciate ligament. American Journal of Sports Medicine 42(5): 1110-1117
- Fu FH, Jordan SS (2007) The lateral intercondylar ridge-A key to anatomic anterior cruciate ligament reconstruction. Journal of Bone and Joint Surgery 89(10): 2103-2104.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.