COVID-19 Policy Handling – The Case of Sweden: Lessons in Effective Policymaking
by Mats Danielson1,2*
1Department of Computer and Systems Sciences, Stockholm University, PO Box 1073, SE-164 25 Kista, Sweden
2 International Institute for Applied Systems Analysis, IIASA, Schlossplatz 1, AT-2361 Laxenburg, Austria
*Corresponding author: Mats Danielson, Department of Computer and Systems Sciences, Stockholm University, PO Box 1073, SE-164 25 Kista, Sweden
Received Date: 14 July, 2025
Accepted Date: 26 August, 2025
Published Date: 29 August, 2025
Citation: Danielson M (2025) COVID-19 Policy Handling – The Case of Sweden: Lessons in Effective Policymaking. J Family Med Prim Care Open Acc 9: 288. https://doi.org/10.29011/2688-7460.100288
Abstract
This article examines Sweden’s response to the COVID-19 pandemic compared to the more restrictive policies adopted by many other countries. It argues that Sweden’s moderate and legally constrained approach, which emphasised personal responsibility and voluntary compliance, resulted in better overall outcomes than strategies focused on severe lockdowns. Using excess mortality as a primary indicator, the analysis shows that Sweden had one of the most successful policies in Europe between 2020 and 2022. Using additional dimensions such as economic performance, mental health, and educational continuity suggests that Sweden avoided many of the broader harms associated with strict containment policies.
A key theme is the contrast between single-metric decision making and a broader policy approach. Most governments prioritised short-term infection control above all other considerations, often overlooking the long-term effects of their interventions. In contrast, Sweden’s public health institutions simultaneously considered multiple objectives, including protecting vulnerable people, maintaining essential services, and preserving public trust. The article interprets this approach as an implicit application of multicriteria decision analysis.
Based on outcomes and underlying processes, the article calls for more conscious use of multicriteria methods in planning future public health crises. It outlines how structured decision modelling, including medical, economic, educational, and psychological expertise, can help balance competing objectives and minimise unintended harm. The Swedish case is not presented as flawless, but it offers a strong example of how proportionality and long-term thinking can guide more effective policymaking. The argument concludes by recommending institutional reforms to embed this approach in future planning, including impact assessments and multidisciplinary advisory bodies. If implemented, such structures would allow governments to respond with greater clarity and effectiveness when faced with future complex societal threats.
Keywords: Effective pandemic policy handling; MCDM; MCDA; Multicriteria policymaking; COVID-19 responses; Public health governance; Societal resilience
Declaration of Purpose
The author was not a health policy researcher before the pandemic and will not be one after it either. Now that COVID-19 has been downgraded from a pandemic to merely a disease of societal concern (as it was declared in Sweden on March 31, 2022), the time has come to reflect on work conducted during this period of more than two years. This text represents an attempt to summarise observations and results, hoping that others may carry them forward in developing more effective methods for policymaking in the future, methods that will be needed when, not if, the next pandemic arrives. It is written primarily as a means of personal mental closure, not with publication in mind. The perspective is a mixed one, shaped by witnessing the pandemic unfolds in Sweden in a way that diverged notably from most other countries and thus offering a different perspective on national crisis management and policy formation, while at the same time reflecting on policies in other countries, based partly on work in projects assessing pandemic policymaking in Botswana, Jordan and Romania (see References). In short, the article discusses policymaking during the pandemic from a decision-analytic viewpoint.
Background
More than two and a half years have passed since the initial outbreak in Wuhan, China, in November 2019. The perceived early situation can be characterised like this: The emergence of the COVID-19 pandemic situation highlighted that many countries were, to a large extent, unprepared for it (GHS, 2020). Policymakers had to operate in conditions of severe uncertainty about the case fatality rate, the spreading patterns of the virus, the timing of incubation, and the number of asymptomatic cases, just to mention a few parameters (Andersen et al., 2020). Risk mitigation measures such as vaccines were missing (Amanat et al., 2020) and proved to be long in the making. Policymakers did not have reliable information about critical measures to protect society from the virus’ spread or at least to reduce its exposure and vulnerability.
Another critical problem in assessing the risk was that the evidence about the case fatality rate was unknown (Muttarak, 2020). As a result of this and many other factors during the COVID outbreak, public authorities had to make decisions based on uncertain quantitative evidence and expert scientific advice (e.g. about possible future scenarios), on assessments of the health system capacity (especially of intensive care units), on expected public adoption of more or less restrictive measures, and on the evolution of national public debates about the issue (NYT, 2020; Time, 2020). Nevertheless, the disaster risk reduction of the pandemic showed that in deciding which measures to implement, many countries acted in an apparently uncoordinated manner.
The measures undertaken by bordering countries or regions within one country were often inconsistent, and decisions on whether or not to impose lockdown were taken based on various, sometimes undisclosed, grounds. Transparency was not high on the agenda, it was often not on the agenda at all. Moreover, many non-pharmaceutical measures were almost immediately limiting individual freedom. They led to high economic and societal costs when undertaken only to avoid fatalities in the short term, disregard the risks that the same measures might produce indirect long-term fatalities due to economic recession and restricted access to healthcare by non-COVID patients, limited access to education (UNESCO, 2020) and other socioeconomic effects.
Initial measures to contain the spread of the SARS-CoV-2 virus were to a large extent based on various epidemiologic risk assessments, which were made primarily by centres of disease control and prevention in Europe and the US and by the World Health Organization (Walker et al., 2020). These assessments established scenarios starting from the number of confirmed infections in a country, effectively downplaying other societal factors. Some countries, such as Japan, initially mainly focused on contact tracing and testing, recommending people to restrict their travels and to teach and work from home. South Korea had a similar approach but with more intensive contact tracing using digital systems. Interestingly, Taiwan, despite its proximity to China, had one of the lowest stringency levels (Hale et al., 2020), as they did not close down schools, workplaces or public transport, and instead mostly focused on tracing and isolating measures. Taiwan’s experience with the 2003 SARS epidemic could account for a series of quick policy decisions involving traveller screening, a wide distribution of masks, hand sanitisers and thermometers (Business Insider, 2020), as well as a large investment in 60 face mask production lines, the latter more of a political control move.
The medium- and long-term socioeconomic costs associated with these initial extreme measures could have put pressure on countries to relax their restrictions. However, it was often argued that the incremental effect of adding another restrictive measure was only minimal (Nussbaumer-Streit et al., 2020). Such was the initial state of affairs in the spring of 2020 when unreflective and poorly deliberated policy decisions dominated the measures taken. After more than two years, what do we know now? How did things go and what could we have done better?
The Case of Sweden
In the global responses to the COVID-19 pandemic, Sweden represented a notable outlier. Unlike most European countries, which imposed sweeping lockdowns, school closures, and other stringent restrictions, Sweden’s strategy was relatively permissive and relied more on public guidance and personal responsibility than coercive legal measures. This approach drew intense criticism early in the pandemic. Many media outlets and even some world leaders labelled Sweden’s policy a reckless experiment, and major newspapers cast Sweden as insane for skipping the strict measures seen elsewhere. The expectation among many experts was that Sweden’s lighter-touch strategy would result in significantly higher COVID-19 mortality compared to its neighbours and other European nations that aggressively cur¬tailed social and economic activity. Indeed, during the first wave of the pandemic in the spring of 2020, Sweden’s COVID-19 death toll per capita did exceed that of neighbouring countries that had implemented hard lockdowns.
Yet, as the pandemic progressed into 2021 and early 2022, a striking outcome emerged: by the end of the pandemic’s major waves (March 2020–June 2022 in Sweden), Sweden had the lowest cumulative excess mortality rates in the European Union. Excess mortality (the number of deaths above the historical baseline) is considered the best measure of the pandemic’s overall impact, capturing both direct COVID deaths and indirect mortality from pandemic-related disruptions. It is independent of the big differences in reporting methods between countries that plague almost every other quantitative measure, such as cumulative confirmed deaths, where the confirmation method differs vastly among countries. According to data submitted to Eurostat (EU’s statistical agency), Sweden’s excess death rate for the period of March 2020–June 2022 is around 3.7% higher than pre-pandemic baseline levels, the lowest such increase among all EU countries. This number is less than a third of the average excess mortality across EU (11.9%) and markedly below many countries that have imposed far stricter COVID-19 control measures. By comparison, for instance, the United Kingdom (not in EU) and Spain, countries that implemented multiple strict lockdowns, have excess mortalities on the order of 10–11%, three times higher than Sweden’s rate. Bulgaria, Poland and Slovakia, the top three in the EU, are all above 18%. Even countries outside Europe with stringent approaches, such as the United States, have excess death rates far above Sweden’s. For example, the U.S. excess mortality is roughly 14%, almost four times Sweden’s. Perhaps revised numbers will change the percentages a bit, but if so probably in favour of Sweden since the accumulated rates are declining faster here. These at first surprising outcomes should prompt a re-examination of pandemic policymaking: How could a country that took such a lenient path avoid the heavy death toll many anticipated, and fare considerably better by the accepted measure of excess deaths?
This article analyses the Swedish pandemic experience in depth, to understand why Sweden ended up with Europe’s (and probably the world’s) lowest excess mortality despite one of the least restrictive responses. The analysis will begin with a comprehensive background on Sweden’s COVID-19 strategy and how it differed from the rest of Europe’s approaches. It will set the stage by detailing the Swedish policies, the rationale behind them, and contemporary reactions. Then, drawing on empirical data from Eurostat, national statistical agencies, and independent studies, we will examine the pandemic outcomes in Sweden versus other European countries, not only in terms of mortality (both COVID-specific and excess deaths) but also economic, educational, and social indicators that reflect the broader multicriteria impact of pandemic responses. Central to this analysis is the role of policymaking structures and paradigms: we will critically assess how Sweden’s governance and public health institutions influenced its policy choices, and contrast this with decision making in other countries where shortterm COVID metrics often dominated. The concept of singlecriterion thinking will be explored as a key explanation for why many governments enacted extremely strict measures, arguably focusing almost exclusively on minimising COVID-19 case and death counts while neglecting other criteria such as mental health, education, economic stability and civil liberties. We will argue that this one-dimensional focus led to dis-proportionate restrictions in many cases, whose benefits in saving lives were relatively small, or even counterproductive when weighed against their sweeping collateral costs. In evaluating this argument, a broad array of peerreviewed studies and data will be used, including meta-analyses of lockdown efficacy, public health assessments of indirect effects (like mental illness prevalence and learning loss), and economic analyses of the pandemic’s toll.
Ultimately, the article will make the case that Sweden’s experience underscores the need for multicriteria decision making frameworks in future public health crises. Rather than singlemindedly pursuing one goal (such as reducing infection numbers at all costs), policy-makers should adopt a balanced approach that considers multiple objectives and trade-offs, from preserving lives to maintaining a functioning economy and overall societal well-being. Such an approach could lead to more proportionate and effective responses when facing future pandemics or similar emergencies. The discussion will conclude by reflecting on lessons learned and how these might be institutionalised in preparedness plans so that the world’s reaction to the next pandemic can avoid some of the pitfalls observed during COVID-19.
Sweden’s Approach in a European Context
Sweden’s strategy: From the outset of COVID-19, Sweden had a pandemic response that differed markedly both in philosophy and execution from that of most other European and non-European nations. The Swedish government, guided by its Public Health Agency (Folkhälsomyndigheten), opted not to impose a legally enforced lockdown at any point in 2020. Instead, Sweden’s response relied heavily on voluntary measures and recommendations. Schools for children under 16 (primary and lower secondary schools) remained open throughout the pandemic, and businesses like restaurants, shops and gyms were not ordered to close, though many did see reduced patronage due to the restrictions on crowd size in an establishment. Rather than mandates, authorities issued guidelines. Citizens were urged to practice social distancing, work from home if possible, avoid non-essential travel, and maintain basic hygiene. Limits were placed on large public gatherings (for example, events were initially capped at 500 attendees, later reduced to 50), and in late 2020 some tighter rules were introduced on restaurant opening hours and crowd sizes. But there were no curfews, no general stay-at-home orders, and no requirement for healthy individuals to isolate beyond common-sense precautions. Swedish health officials did not widely recommend wearing masks in early 2020 and was never mandated in general public spaces. Masks were later advised but not mandated in some crowded settings like public transport during peak hours, but it was not enforced and compliance remained low. The policies were based on disease control practices, not on the early herd immunity hypothesis that soon turned out to be false. In the words of the independent Corona Commission appointed by the Swedish government to review the response: “The approach chosen by Sweden was based on voluntary measures and personal responsibility, rather than more intrusive interventions” (Coronakommissionen, 2021). This emphasis on individual personal responsibility reflected both a legal reality, Sweden’s Infectious Diseases Act did not initially grant authorities broad powers to quarantine healthy populations, and a public health philosophy that trusted citizens to adapt their behaviour when given credible information and guidance.
Under Sweden’s governance structure, the decision-making authority in health crises is somewhat decentralised and technocratic. Folkhälsomyndigheten and its experts held a constitutionally and culturally respected role in guiding policy, and there was relatively little direct political interference in the day-to-day management of the pandemic. The government largely heeded the advice of its health agency. This meant that Sweden’s measures were calibrated based on the agency’s assessment of what was epidemiologically warranted and societally sustainable, rather than on political demands to do something dramatic in response to rising case numbers. There is evidence that Swedish health officials were consciously weighing not only infection control but also the long-term sustainability and side effects of restrictions. For instance, keeping schools open for younger children was a deliberate choice informed by i) a recognition that school closures could cause serious harm to children’s learning and well-being, also in a longer perspective, and ii) early studies showing that school-aged children did not significantly contribute to the spread. Folkhälsomyndigheten often spoke of finding a balanced and evidence-based approach, instead of copying more drastic measures witnessed in other European countries, whose effectiveness and costs were unproven. While critics argued that Sweden’s response was slow or even inhuman, internal documents and later testimony suggest the strategy was intentional. The idea was to introduce interventions that could be maintained over a long period without undermining public trust or causing undue damage to society, again displaying multi-dimensional thinking. Pandemic preparedness plans that existed before COVID-19 (in Sweden and many other countries) generally did not include full lockdowns as a recommended measure for influenza-like pandemics. Instead, they envisioned voluntary quarantine of the sick, public advice, and only limited compulsory restrictions. Sweden largely followed its plan, whereas many other countries diverged radically from pre-existing plans in favour of harsher single-perspective emergency measures. Naturally, Sweden had its share of alarmist reports, many of them academic, projecting a monumental disaster unless a strong lockdown was immediately imposed, and also an early general appeal from over 2000 academic researchers from a variety of fields calling for an immediate lockdown without any evidence that it would be effective (DN, 2020). But already in late 2020, academic research suggested that the Swedish nonlockdown policy had been successful (Kavaliunas et al., 2020).
Rest of Europe’s Approach: In contrast, from March 2020 onward, most of Europe undertook far more restrictive policies. Italy, which faced the earliest outbreak in Europe, initiated a full national lockdown in early March 2020, shutting down workplaces, retail, and hospitality, and confining residents to their homes except for essential needs. Spain and France soon followed with similarly draconian stay-at-home orders. The United Kingdom, after some hesitation and debate, imposed a lockdown by late March 2020 as well. Across Europe, schools and universities were closed and moved to remote learning; restaurants, bars, gyms, cinemas, and non-essential shops were closed; travel was severely restricted with closed borders and quarantine rules. Many countries deployed emergency powers or special legislation to enforce these measures, often with police fines for violators. For example, France required permission slips for anyone to leave their home during the lockdown, and the UK government introduced regulations enforceable by law to ban gatherings and non-essential movement. In the spring of 2020, virtually every European country except Sweden and perhaps Belarus (which also controversially stayed largely open) had some form of mandatory lockdown or comprehensive closure regime. Even Sweden’s Nordic neighbours, Denmark, Norway, and Finland, broke from their traditionally liberal approaches by quickly enacting school closures and lockdowns in March 2020, albeit generally for shorter durations and with earlier reopening than seen in Southern Europe. Denmark, for instance, closed its borders and schools and banned gatherings of over ten people in March 2020, though it began reopening primary schools as early as April 2020. Norway also imposed lockdown measures, closing educational institutions and many businesses, which helped keep its cases and deaths low during the first wave.
The prevailing rationale across Europe for these unprecedented peacetime restrictions was the precautionary principle in the face of a poorly understood and fast-spreading deadly virus. Early epidemiological modelling, most notably the very influential report from Imperial College London in March 2020, had predicted catastrophic death tolls (hundreds of thousands of deaths in the UK) unless drastic measures were taken (Ferguson et al., 2020). Confronted with reports of overcrowded hospitals in Wuhan and Northern Italy, policymakers felt compelled to prioritise the immediate goal of suppressing or even halting the virus’s spread to save lives and prevent health system collapse, although it was not known whether that was even remotely possible. This led to what can be described as single-criterion decision making in many cases. The only criterion was minimising COVID-19 transmission and mortality in the short term. Other considerations, such as the economic cost, impacts on mental health, child development, and civil liberties, were claimed to be secondary, on the logic that a temporary sacrifice was needed to control the emergency. Public communication in many countries reinforced an atmosphere of imminent existential threat. Governments framed the situation as a war against the virus, thereby justifying extraordinary measures. As one multicriteria risk governance analysis later observed, crisis messaging often used aggressive metaphors (such as fight the virus or flatten the curve) and sometimes assigned blame towards those not complying or towards external actors, in order to force compliance (Ekenberg et al., 2021). The result was a high degree of social and political consensus in favour of strong lockdowns in early 2020, with a few notable exceptions like Sweden where officials were more cautious about such extreme steps.
Key Differences and Initial Outcomes: By mid-2020, these divergent strategies yielded very different immediate outcomes. Countries that locked down hard generally crushed the first wave. Norway, Finland, and Denmark kept COVID-19 deaths very low in the spring of 2020. Sweden, by not imposing a lockdown, experienced a larger first wave of infection and deaths. It was even on par with the UK and Italy by mid-2020, though lower than Belgium’s extremely high toll. Within Europe, Sweden ranked in the worst half of per-capita mortality in the initial wave (March– May 2020), though not among the worst. Critics pointed to this outcome as evidence that Sweden’s strategy had failed. The Swedish authorities themselves acknowledged some failures, particularly in protecting elderly residents in nursing homes, who accounted for a large proportion of Sweden’s early deaths. Problems in the nursing homes included the fact that many staff did not speak Swedish or English, thus not understanding information on new routines. In addition, a general mistrust of authorities among that personnel led to scepticism towards official guidance, resulting in the neglect or out-right dismissal of newly introduced procedures. The Swedish Corona Commission’s interim reports in late 2020 and 2021 criticised the government for insufficiently safeguarding elderly care homes, although they also noted that many of the failings (like structural shortcomings in elderly care and slow initial testing scale-up) were not unique to Sweden. Nevertheless, the short-term verdict in much of the global discourse was that Sweden’s choice to remain open led to unnecessary deaths that could have been avoided with stricter measures. Scandinavian neighbours Norway and Denmark were often seen as having done the right thing by locking down early, thereby presumably saving lives.
However, the picture became much more complex as the pandemic progressed into sub-sequent waves. Many countries that had implemented strict lockdowns in the spring of 2020 experienced significant COVID-19 outbreaks later that year or in 2021, once restrictions were lifted or relaxed. As predicted by e.g. Folkhälsomyndigheten, the virus proved difficult to contain in the long run, and nations like the UK, Spain, France, Italy, Poland, and others endured large waves in late 2020 and/or during 2021 despite continued intermittent restrictions. Cumulatively, their COVID death tolls climbed. In contrast, Sweden saw a much more moderate second wave in late 2020 and another in 2021, but the per-capita deaths in those later waves were below most lockdown countries. For instance, during the Delta and Omicron variant surges in late 2021, Sweden’s COVID-19 mortality rate was low compared to many parts of Eastern Europe that imposed harsh measures but had lower vaccination rates. Moreover, by the spring of 2022, after vaccines had been widely available for more than a year, some countries that had largely suppressed COVID until then (like New Zealand, Australia, or Iceland) experienced their first major COVID waves, temporarily giving them very high per-capita death rates, whereas Sweden by that time had built up a degree of natural immunity combined with vaccination. This natural immunity was largely built from exposure to the less harmful earlier mutations before Omicron. Thus, the timing and distribution of deaths vary widely. Sweden had more deaths upfront in 2020, whereas others had more later, even now in August 2022. These dynamics would eventually reflect in the excess mortality tallies over the full span of the pandemic.
Sweden’s Outcome Compared to Europe
Excess Mortality as a Metric: Excess mortality is widely regarded by demographers and epidemiologists as the most objective single measure of a pandemic’s impact on mortality. It captures all deaths above a baseline (usually the average from preceding pre-pandemic years), regardless of official cause. This is important because official COVID death counts can be affected by diagnostic capacity, testing criteria, and attribution policies. Some countries undercounted COVID deaths (for example, by not testing the deceased or excluding deaths outside hospitals), whereas others (such as Sweden) overcounted by testing all deaths from other causes as well and bookkeeping them as COVID cases if the virus was found at all, or had different definitions. Excess mortality sidesteps these issues by simply looking at total death deviations. It also implicitly includes indirect pandemic deaths, for instance fatalities resulting from healthcare disruptions, mental health crises, or economic hardship. Given this, many analysts argue it provides the broader perspective needed to evaluate how a country fared overall.
Continuously accumulated statistics have started to draw attention. By the end of 2022, data from Eurostat and other sources allowed a cumulative comparison of excess mortality across Europe’s pandemic experience. The results of this comparison confounded many experts. Sweden had the lowest cumulative excess mortality increase in Europe for 2020–2022 (Figure 1). According to figures compiled by Statistics Sweden and reported to Eurostat, Sweden’s
total mortality in those three pandemic years was only about 4.4% higher than in the immediately preceding years (adjusted for population size). This was indeed the smallest increase among all European Union member states. The average excess mortality across EU countries over 2020–2022 was about 11.1%. Many large countries had much worse outcomes. Italy and Spain, which were hit hard early, ended up with excess mortality of around 15%. Eastern European countries that suffered devastating waves in 2021 (and had lower vaccination uptake) topped the charts. Countries like Bulgaria, Poland, and Romania registered some of the highest excess death figures in Europe, exceeding 15% or even 20% above baseline over the period. Even Germany, often praised for managing the first wave well, eventually accumulated a significant excess death toll after successive waves. Its figure was around the European average by 2022. The United Kingdom, no longer in the EU but tracked by comparative studies, had about a 10% excess mortality, more than double Sweden’s rate. The United States fared worse, with around a 14% increase.
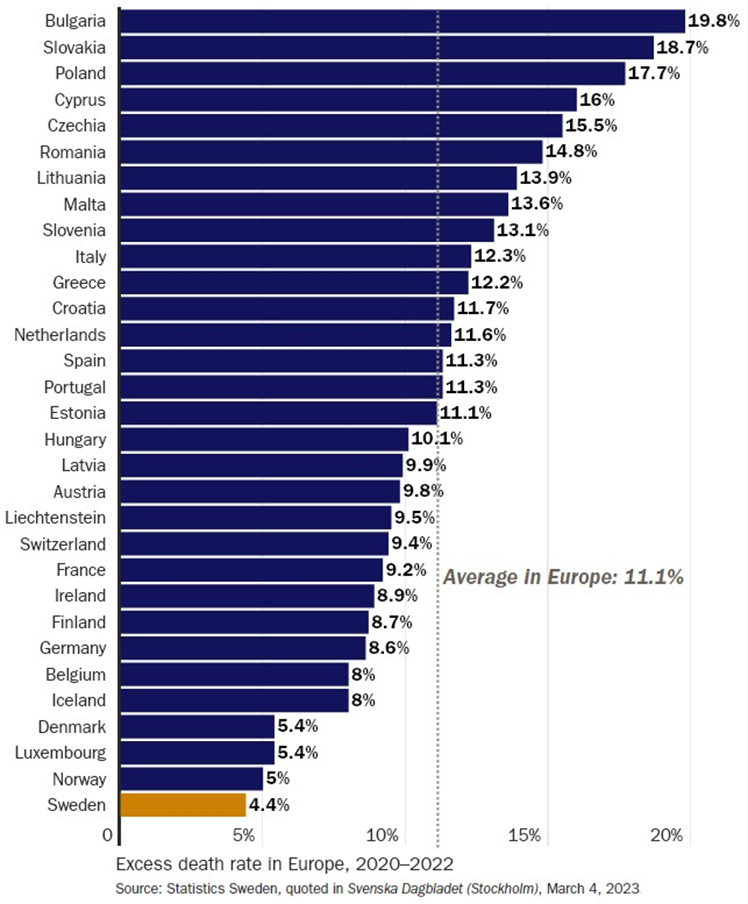
Figure 1: Excess mortality rates in mainland Europe during 2020–2022.
To put Sweden’s outcome in perspective, imagine two alternate scenarios. One resembling the average European pandemic impact (11% excess mortality) and one resembling Sweden’s. If Sweden had experienced the average European outcome, it would have seen roughly two to three times as many excess deaths as it did. Conversely, if countries with far harsher restrictions had matched Sweden’s outcome, tens of thousands of lives might have been saved in those countries (or at least, deaths deferred beyond 2022, we cannot know yet). This is paradoxical at first glance. Stricter measures did not translate into fewer deaths in the long run, and the country with one of the least stringent approaches had one of the fewest excess deaths. Such data challenges the initial narrative that Sweden’s strategy was a disastrous gamble. On the contrary, by this measure, Sweden outperformed the rest.
Other Impacts Beyond Mortality: A full comparison of Sweden versus other countries must look not only at mortality but also at the broader societal impacts of the pandemic and responses. Here, Sweden appears to have advantages precisely because it avoided many of the harshest measures. For instance, education outcomes in Sweden were far less impacted than elsewhere. Swedish elementary and middle schools remained open all throughout, while many countries kept children at home for months or shifted to inferior online learning. The result is that Swedish children suffered minimal learning loss. A study by Hallin et al. (2022) found no learning loss in Sweden during the pandemic for primary school students. Assessments of reading and word decoding skills showed that Swedish children’s performance in 2020–2021 was not significantly lower than pre-pandemic cohorts. Even children from low socioeconomic backgrounds, who in many countries were disproportionately hurt by school closures, did not experience learning declines in Sweden under the open-school policy. In contrast, another study by Betthäuser et al. (2022) reports that students worldwide lost on average more than one-third of a school year due to closures and disruptions. Many countries will suffer from these learning deficits, which are particularly pronounced in places that kept schools closed for long durations. Some countries in Europe and the U.S. had intermittent closures lasting a year or more in total. The World Bank and other organisations have warned of a generational catastrophe in education, with learning poverty increasing in low- and middle-income countries due to prolonged school shutdowns. While high-income countries provided remote education, outcomes were still worse than in-person schooling. By keeping schools open, Sweden spared its youth this educational setback. Only grades 10–12 went remote for some time. This is an important benefit that might not show up in death statistics but has long-term implications for human capital and well-being.
Economically, Sweden fared exceptionally well. The pandemic caused a global recession in 2020 as lockdowns and uncertainty suppressed activity. Sweden was not immune to these global forces; its economy, being very open and trade-dependent, saw GDP decrease as exports fell and consumer spending dipped. However, Sweden’s GDP decline in 2020 was smaller than that of most of Europe, and its recovery was faster. By the end of 2021, Sweden’s economy had not only rebounded but grown slightly above its pre-pandemic size, unlike many peers. Analyses by the OECD and others indicate that while the world economy in 2021 was still about 2.9% below the pre-pandemic trend and the Eurozone economy about 2.5% smaller, Sweden’s economy was approximately 0.4% larger than its pre-pandemic baseline. This occurred despite Sweden implementing far less fiscal stimulus than most countries. By comparison, the United States economy was still 1.2% below trend by the end of 2021, and many European countries lagged even further. In concrete terms, Sweden experienced a milder downturn and a quicker return to growth. Unemployment in Sweden did rise in 2020 but not drastically more than usual, and many businesses, especially in retail and hospitality, survived without the mandated closures that devastated such sectors elsewhere. Government finances in Sweden were also less strained: while many countries took on enormous debt to fund furlough schemes and bailout packages during lockdowns, Sweden’s fiscal response was more moderate, leaving it in a stronger fiscal position post-pandemic. Naturally, Sweden’s economy still suffered somewhat from the pandemic’s global impact (for example, its manufacturing and export industries were hurt by supply chain issues and reduced foreign demand), but it avoided the self-inflicted economic damages of domestic shutdowns.
Public Health and Mental Health: Another major area of impact is public health beyond COVID. Lockdowns and strict measures, while aiming to curb the virus, had side effects on mental health, healthcare access, and social well-being. Mental health problems rose worldwide during the pandemic. The isolation, fear, and disruption caused a spike in anxiety and depression: The World Health Organization reported a 25% increase in the global prevalence of anxiety and depression in the first year of the pandemic alone (WHO, 2022). Countries that endured long lockdowns often saw significant deteriorations in psychological well-being. For instance, youth mental health surveys in 2021 found very high levels of persistent sadness and hopelessness. In the U.S., over a third of high schoolers reported poor mental health during the pandemic and incidences of self-harm and suicidal thoughts increased (CDC, 2022). While Sweden certainly experienced bad times due to the pandemic, it did not subject its population to the same degree of isolation. People in Sweden could largely continue seeing friends or family, going outside freely, and maintain a fairly normal life. This mitigated some mental health harms. Sweden, by avoiding stay-at-home orders, spared many people the worst of these effects. Surveys in Sweden during 2020 showed some increase in worry and loneliness, but not as pronounced as in countries under lockdown. Moreover, maintaining open schools helped protect children and adolescents from some mental health harms associated with long periods out of school and parents forced to stay at home during what should have been school days.
There were also indirect health effects of strict pandemic measures. In many countries, hospitals postponed elective surgeries, cancer screenings, and routine care during lockdown periods, leading to untreated conditions and later-stage diagnoses. Fear of the virus kept people from seeking care even for urgent issues like heart attacks or strokes, contributing to non-COVID excess deaths. Alcohol and substance abuse reportedly rose in some countries as a coping mechanism during confinement. Domestic violence incidents increased as victims were trapped at home with their abusers. A United Nations report in 2020 warned of a shadow pandemic of domestic violence amid lockdowns. While Sweden likely faced some of these issues simply due to the global COVID stress, the continuous functioning of society at a moderate level may have reduced the severity of these secondary effects. Healthcare services remained accessible so people could leave home and seek help. Police data in some locked-down countries showed spikes in domestic disturbance calls during confinement. It would be worth examining Swedish data for comparison. Preliminary indications are that although domestic violence remained a concern, Sweden did not see the same jump correlated with a lockdown period, since there were no stay-at-home laws to trap people.
Thus, on a range of societal indicators, from economic output to student learning to mental and physical health side effects, Sweden appears to have mitigated the pandemic effects more smoothly than many nations that imposed harder restrictions. Its strategy sought to minimise disruption to normal life, consistent with a reasonable degree of infection control. By keeping much of society up and running, Sweden avoided some of the worst collateral damage of the pandemic response. Crucially, these benefits did not come at the expense of a high death toll. Quite the opposite, as we have seen with the excess mortality data. This combination of outcomes is what makes Sweden’s case so compelling and worthy of study: it challenges the assumption that there is an inevitable trade-off between saving lives and preserving normal life. The common narrative was that Sweden chose economy over lives, whereas others chose lives over economy. In reality, Sweden managed to preserve both lives and a degree of normalcy better than most. To understand how this happened, it is essential to examine the policymaking processes and frameworks behind these pandemic policies. The following sections will discuss how different governance structures and mindsets formed these different outcomes. Notably, the contrast between Sweden’s multicriteria long-horizon thinking and many other countries’ single-criterion short-term thinking.
Policymaking in Public Health Crises
A critical factor behind Sweden’s unique approach was the structure of policymaking and governance in the country’s pandemic response. This can be contrasted with how decisions were made in many other countries, highlighting how institutional setup and mindset can lead to very different policy choices during the same crisis.
Sweden’s Decentralised Expert Agency Model: Sweden’s public health policymaking is anchored by expert agencies with statutory independence. In a health emergency, Folkhäls omyndig heten takes the lead in formulating recommendations. During COVID-19, the agency became the primary architect of Sweden’s response. The government is role was largely to support and implement the agency’s advice, rather than to direct it. This model meant that decisions were driven by public health experts who were accustomed to weighing health measures against societal norms and scientific evidence, rather than by politicians facing immediate public pressures. Sweden also has a tradition of constitutional constraints on government power in peacetime. Before COVID, there was no legal provision for a general lockdown of citizens. Quarantine powers existed mainly for individuals who were sick, not for whole healthy populations. It was only in early 2021 that Sweden hastily introduced a temporary pandemic law to permit stronger measures such as capacity limits in shops or closing specific venues, but even that law did not allow for broad stay-at-home orders of the kind imposed in many other countries. Additionally, Sweden’s constitution protects freedom of movement and the right to education, making sweeping closures legally difficult to justify except under a declared state of emergency, which Sweden did not invoke during COVID. The Swedish government chose not to declare an emergency, instead operating within normal administrative law.
The policymaking structure in Sweden also emphasised consensus and public trust. The authorities communicated in a matter-of-fact, calm tone, with daily press conferences providing updates and rationale for guidelines. Surveys during the pandemic indicated that a majority of Swedes trusted the public health agency and complied with its advice (even absent legal coercion). The Swedish strategy was sometimes described as aiming for sustainable compliance: by not overreaching with draconian rules, they hoped to maintain public buy-in for the long haul. Indeed, one can argue that this strategy treated the pandemic as a marathon, not a sprint, in contrast to the more reactive strategies seen elsewhere.
Other Countries’ Emergency Command-and-Control- Structures: In many other European countries, policymaking during the pandemic quickly took a more top-down, politicised turn. Governments formed emergency cabinets or task forces; normal legislative processes were often sidestepped via decrees or special laws. In the UK, for example, pandemic policy was decided by the Prime Minister and a handful of ministers advised by select scientific committees (SAGE, the Scientific Advisory Group for Emergencies), with Parliament given little opportunity to debate before lockdowns were imposed. A similar pattern occurred elsewhere: political leaders, worried about an exponential spread, often centralised authority and acted quickly. While expert advice was sought, it frequently came from epidemiologists or modellers whose focus was the virus trajectory. Other domains of expertise (economists, mental health experts, educators) were usually not equally represented at the decision table in the critical early weeks. This meant that the policymaking structure was siloed, focused primarily on virology and acute healthcare capacity, with limited integration of other perspectives and not toward a multidisciplinary assessment of overall well-being. As one analysis noted, many countries acted in an apparently uncoordinated manner initially, with inconsistent measures even between neighbours, and decisions to lock down were not always based on transparent criteria but often on political and public pressure (Ekenberg et al., 2021). A sort of bandwagon effect occurred: once some countries locked down and were perceived to be successful (e.g. China’s Wuhan lockdown, then Italy’s), others followed suit in quick succession, fearing regret if they did not. This political dynamic can be described as better-safe-than-sorry, but sometimes it manifested as political leaders fearing blame more than they feared the harms of lockdown. In risk psychology, this is akin to aversion to visible loss: a death toll climbing on TV is a highly visible crisis for which officials might be blamed, whereas a rise in depression or a recession, being slower-moving and less direct, might not be immediately blamed on policy choices. Thus, the incentives in many policy structures skewed towards minimising COVID deaths at all costs, because those were being closely tracked in real time, easy to display and hard to refute on TV.
The institutional checks and balances also weakened in many places. Courts, legislatures, and civil society often rallied behind the executive in the interest of national unity against the virus, or they were undercut by states of emergency. This left few voices to advocate for considering alternative approaches. In some cases, experts who cautioned against overzealous measures or who pointed out the downsides were marginalised or accused of downplaying the threat. The public arena did not always allow for a balanced debate, especially in 2020 when fear was high. This environment nurtured single-criterion thinking: public health (narrowly defined as stopping COVID) became almost the sole lens of policymaking.
Precautionary Principle vs. Evidence-Based Balance: The decision-making divergence can also be framed as differing applications of the precautionary principle. In a scenario of uncertainty and potentially catastrophic outcomes, a precautionary approach argues for erring on the side of caution, i.e. doing more and sooner, to mitigate the worst-case scenario. Countries like New Zealand excelled at this by opting for a strict elimination strategy (aiming to reduce cases to literally zero) given the uncertainty. Sweden’s decision-makers took a different approach: they certainly did not dismiss the virus as harmless, but they also gave weight to the certainty of harm that extreme measures would cause. In other words, while much of the world fixated on the uncertain, worst-case fatalities from COVID, Sweden’s health officials also considered the certain, multi-faceted damage that draconian restrictions would inflict on society. This is a more evidence-based and pluralistic approach to precaution: it tries to minimise overall harm, not just harm from one source. For instance, Sweden’s officials explicitly mentioned early on that lockdowns could lead to long-term health problems by increasing unemployment (which is correlated with worse health outcomes), that school closures would harm children, and that severe curbs on movement could be unsustainable as the populace might eventually reject them or suffer fatigue. Folkhälsomyndigheten often raised the point that any measures must be feasible to keep in place, not just for weeks but potentially for many months, a valid concern given that the pandemic has last-ed over two years (and is not yet declared over in parts of the world). Many other policy-makers initially treated the pandemic as a short-term crisis where normal life should be paused for a few weeks and then return to normal after the virus was successfully sup-pressed. “When people have stopped coughing, it’s business as usual again.” When that strategy failed, they faced the dilemma of re-imposing measures repeatedly. Sweden’s structure, by planning for a long game, arguably avoided this situation.
It is also interesting that Sweden’s strategy was not entirely opposite to international expert circles. Many epidemiologists advocated approaches that were less invasive than full lockdowns. The difference is that Sweden’s system listened to and empowered those voices. The Great Barrington Declaration (an open letter in Oct 2020 by several epidemiologists and public health scientists from Harvard, Stanford, Oxford, etc.) is an example of an alternative strategy (focused protection of the vulnerable while allowing society to function for others) that aligns in spirit with multicriteria thinking. While that declaration was controversial and heavily criticised by proponents of lockdowns, Sweden’s actual policy in 2020 was not identical but closer to that approach than perhaps any other country. In other countries, even suggesting such ideas was often dismissed at the time. Folkhälsomyndigheten, by contrast, maintained a dialogue about how to protect nursing homes without shutting down schools and businesses completely. In short, the Swedish policymaking structure inherently forced a broader deliberation: the public health agency had to consider overall public health, not just COVID. By mandate, they oversee things like mental health, other diseases, etc., so they naturally were conscious of those aspects. In countries where COVID response was managed by a single-criterion strategy focused on the virus, that breadth of perspective was lacking.
Transparency and Accountability: One final structural aspect is accountability and evaluation. Sweden established its independent Corona Commission relatively early (in the summer of 2020) to investigate and report on the handling of the pandemic. This body provided interim reports during 2020 and 2021 and a final report in October 2021, offering critique and recommendations. This shows a structural commitment to learning and accountability even during the crisis. Other countries too would have inquiries (like the UK’s planned COVID inquiry, etc.), but often much later. The presence of a commission might have also influenced decision making by highlighting areas needing improvement (for example, after severe criticism, Sweden rightfully but very late intensified measures to protect the elderly by the fall of 2020). In contrast, some countries were so consumed by crisis management that little self-evaluation occurred until the worst was over. The constant self-reflection in Sweden may have helped correct errors where needed without abandoning the fundamental strategy.
In summary, Sweden’s decision structure, characterised by expertled policy, legal constraints against extreme measures, voluntary compliance, and a multi-dimensional notion of public health, enabled a response that inherently balanced multiple criterion. Many other countries, by centralising authority in political hands and framing the crisis as singularly about defeating COVID at all costs, predisposed themselves to a one-dimensional, shortterm strategy. This structural difference is key to understanding why responses differed and why outcomes like excess mortality converged paradoxically in favour of the more moderate approach. Next, we will delve deeper into the concept of single-criterion thinking and how it manifested in pandemic policies, and contrast that with what a multicriteria approach entails.
The Risks of Single-Criterion Thinking
Single-criterion thinking refers to a decision-making approach that fixates on one metric or objective to the exclusion of other important considerations. In the context of the COVID-19 pandemic, the singular criterion that drove many government responses was the short-term COVID-19 caseload and death count. Policies were often judged almost entirely by how effectively they could reduce the viral spread and prevent immediate COVID deaths. While saving lives is a paramount goal, the problem with this tunnel vision is that it can lead to policies that achieve the goal in the narrow sense but cause equal or greater harm in other domains. It also risks oversimplifying a complex problem: treating a pandemic as if the only thing that mattered was one virus’s death toll, rather than viewing it as a multifaceted societal crisis. In this section, three common mistakes by single-criterion thinking are highlighted.
One-Dimensional Metrics
Throughout 2020 and 2021, many officials and media outlets highlighted metrics like the R number (virus reproduction rate), daily new case counts, hospital occupancy, and daily reported COVID deaths. When these numbers rose, pressure mounted to impose or tighten restrictions; when they fell, restrictions eased. This feedback loop essentially made policy a function of one set of disease indicators. Little comparable quantitative weight was given to metrics of economic health (e.g., unemployment rate), educational progress (e.g., days of school missed), or mental health (e.g., rates of depression or anxiety). Indeed, some leaders explicitly stated that they were choosing human life over the economy. While sounding like a noble sentiment, it was a false dichotomy, ignoring that economic downturns also cost lives and well-being. In the heat of the moment, it may have seemed that every other concern was secondary and could be deferred (“We will deal with the economic and social fallout later; right now, we must stop COVID at any cost”). However, as months went by, it became clearer that “later” would be too late for many impacts. Many businesses would never recover, especially small and family-run ones. Some children would never fully catch up in school, and some health damage (suicides, advanced cancers from missed screenings, etc.) was irreversible.
Cost-Benefit Imbalance
By mid-2020, a few scholars began pointing out that many COVID measures were not subjected to rigorous cost-benefit analysis, the kind normally applied to major public policies. Allen (2021) early critically reviewed over 90 studies and found that most had overestimated the benefits of lockdowns and underestimated the costs. He noted that initial projections of lockdown benefits assumed unrealistically that populations would remain completely susceptible and not change behaviour unless mandated (whereas in reality, voluntary behaviour changes account for much virus mitigation). He also highlighted that many studies made heroic assumptions about the value of lives saved (using models that valued any life extension equally, even if only a few months for someone terminally ill, which can dramatically inflate the benefit side in calculations). When Allen performed a cost-benefit analysis in terms of life-years for a country like Canada, he found that the cost in life-years of lockdown (due to things like reduced healthcare, economic recession impacts, suicides, etc.) exceeded the life-years saved from COVID by lockdown by a factor ranging from about 3.6 to as high as 282 under plausible assumptions. In other terms, this means the collateral damage of lockdowns could be several times worse than the disease impact it prevented, in terms of years of life lost or impaired. He went so far as to suggest that lockdowns may rank as one of the greatest peacetime policy failures in modern history if evaluated on that basis. While that claim is strong, it underscores the extent to which focusing on one criterion (immediate COVID lives saved) and ignoring others (life-years lost elsewhere) can mislead policy.
Another way to see the imbalance is by comparing predicted lives saved versus actual. The infamous Imperial College model that influenced the UK and the US predicted that lockdowns would save hundreds of thousands of lives in each country (Ferguson et al., 2020). In reality, by the end of 2020, the UK still had one of the highest COVID death tolls in Europe despite multiple lockdowns, and the excess mortality suggests that even if many COVID deaths were delayed in the short run, other excess deaths or later COVID waves filled in much of that gap.
Overlooked Criteria
Let us look in more detail at four of the criteria that were underemphasised in typical single-criterion thinking:
Economic well-being: It is well-established in public health literature that economic downturns and poverty correlate with worse population health and higher mortality in the long run. Unemployment, for example, is associated with higher rates of suicide, cardiovascular disease, and overall mortality. The International Monetary Fund noted that the 2020 recession was the worst since the Great Depression in many countries. By prioritising COVID suppression above all, governments knowingly triggered recessions (some policy-makers said that “We can worry about the economy later”). While emergency financial aid blunted some immediate suffering, the long-term effects include ballooning public debt (which can crowd out future social spending), lost educational and employment opportunities for a generation, and small business failures. Sweden was not immune to a global recession but kept more of its economy functioning domestically, likely reducing business closures. To illustrate, countries like Spain or Italy saw GDP plunges around 10–12% in 2020; Sweden’s fell 2.8%. The Eurozone unemployment rate spiked while Sweden’s did not dramatically diverge from its usual (albeit high) levels. These differences mean fewer life disruptions. On the flip side, those countries that did “everything” to suppress COVID ended up still having similar total deaths (since once they reopened, the virus often came roaring back), plus economic scars. Viewing the concept of maximising health broadly, maintaining economic stability should have been a key criterion as well. Not just morally (to avoid hardship) but pragmatically for health (as economic distress translates directly to ill health).
Education and children’s welfare: This criterion was shockingly absent from many early pandemic decision processes. Schools were often closed with little consideration of their essential role beyond academics (food security for children, social development, safe havens from abusive homes, etc.). The assumption was that children are resilient or that remote learning could substitute. Only later did the magnitude of learning loss and psychosocial harm to children become clear. Students in the U.S. for example are estimated to be months behind in math and reading, with disadvantaged students suffering most. Some countries essentially lost an entire year of normal schooling. From a multicriteria perspective, protecting the younger generation’s development and future should have weighed heavily. Sweden implicitly gave this criterion more weight by keeping schools open (up to 9th grade) throughout 2020. The result, as discussed, was no measurable learning loss in primary school reading, versus severe losses elsewhere. The long-run health and prosperity of today’s children is a criterion that arguably was comparable to the shortrun survival of the elderly, but it was not framed that way in the heat of the crisis. Society faced a trade-off between the immediate risk to older people and the long-term well-being of the young. A multicriteria approach would have sought a balance.
Mental health and social fabric: We have already cited evidence that lockdowns increased mental health service needs and stress disorders. Social isolation, loss of community activities, and the general climate of fear all took a toll. In some countries, funerals, weddings, and religious gatherings were banned or severely limited, yielding an irreparable loss to social cohesion and human dignity. The fabric of society was stretched. A multicriteria approach would formally register these as costs to weigh: how many cases of depression is too high a price to pay for preventing one case of COVID? It is a difficult comparison, but neglecting it entirely means those depression cases were effectively ignored. Sweden did impose some limits (e.g., at times limiting gatherings to 50 or even 8 people in late 2020), so it was not fully spared the social restrictions. But because there was no blanket stay-home order, the ability to maintain some social contact (in a safe manner) likely alleviated the worst loneliness. The difference is qualitative: being legally forbidden to visit a friend or relative (as in lockdowns) versus being advised to use caution but ultimately allowed. The latter respects mental well-being and personal judgement, whereas the former prioritises infection control at any psychological cost.
Non-COVID healthcare: One particularly important criterion is maintaining healthcare for all conditions. Lockdowns and the overwhelming focus on COVID led to the cancellation of many non-urgent medical appointments. However, untreated chronic conditions or undiagnosed cancers can become lethal. Data from various health systems showed drops of 20–40% in new cancer diagnoses in 2020, implying many cancers went undetected until later stages. Heart attack and stroke admissions also dropped, implying people were either not reaching the hospital or not going in time. These will translate to higher mortality outside COVID. Indeed, some analyses of excess mortality in late 2021 and early 2022 in Europe noted a portion of excess deaths that were not COVID-related, potentially reflecting such deferred care. If decision-makers had explicitly considered all-cause long-term mortality as their criterion, rather than just short-term COVID mortality, they might have adopted less disruptive measures. Sweden’s all-cause excess was low, suggesting they did not see a big spike in non-COVID deaths due to their approach (though Sweden did struggle in spring 2020 with acute care load, they never formally rationed care to our knowledge, whereas some places effectively had to at peak moments).
In countries with a single-criterion focus, fear and worst-case projections often dominated the decision making, sidelining normal policy analysis. While it is natural for standard procedures to be initially short-circuited in COVID circumstances, it is not a time for single-criterion analyses. On the contrary, it is the time for formal multicriteria analyses to shine. Narratives such as “if it saves even one life, it is worth it” were politically popular but practically grossly misleading. No policy can be evaluated by that standard. If literally saving one life justified infinite cost, we would set speed limits at 5 mph (to save accident victims) or ban alcohol outright (to prevent any drunk-driving deaths), which we do not because society balances trade-offs. In COVID, however, this balancing logic broke down initially. Media contributed by extensively reporting COVID deaths and stories, while largely ignoring the voices of those harmed by restrictions (who were less visible). This asymmetry made the criterion of COVID suppression hyper-salient.
It appears that Sweden, if not by formal process then by culturalpolitical ethos, applied somewhat more of a multicriteria perspective. The Swedish authorities repeatedly mentioned that public health is holistic. It encompasses mental health, economic stability, and other medical outcomes, not just the virus. They recognised early that trying to completely suppress COVID at the expense of everything else might cause a public health disaster. This can be seen as a kind of multicriteria decision analysis (MCDA) approach, even if they did not use that terminology. Essentially, they tried to optimise a vector of objectives: minimise COVID harm plus minimise societal disruption plus maintain trust and compliance, plus keep the economy and schools running as normally as possible. Of course, they could not achieve all objectives perfectly (COVID still caused harm, and they did implement some restrictions), but their balanced approach arguably found a better trade-off than many other strategies did.
The final outcomes that we have reviewed (low excess mortality, preserved economy, preserved education, etc.) indicate that Sweden’s de facto multicriteria strategy was successful in optimising overall well-being through the crisis. On the contrary, the single-criterion approach of others may have reduced their COVID death count marginally in the very short term, but not enough to outweigh the damage when looking at the big picture by mid-2022. The fact that by mid-2022 those countries often had higher total mortality suggests that even the singular goal (fewer deaths) was not optimised in the long run, making their extra sacrifices even harder to justify.
To avoid misunderstanding, it is not that lockdowns and strict measures had zero effect. They did slow down transmission temporarily (3.2% fewer deaths in the first wave on average), and more in some cases. In certain contexts, initial lockdowns might have prevented hospitals from collapsing, which is a legitimate short-term goal, although Sweden’s healthcare system did not fold. Again, the one critical mistake in Sweden was the bad state the elderly care homes were in: management, staffing and emergency planning were all subpar. The elderly care was not resilient to community transmission. Yet there were no regulations on respiratory protection or rules that staff with sick people in their household should stay home. However, after that immediate crisis, the continuation or reinstatement of broad lockdowns became increasingly hard to justify as more data emerged about the virus’s true fatality rates: substantially lower than initially feared for the general population, though still severe for the elderly, and as the collateral harms mounted. Many countries, however, found it politically difficult to change course. They were in a sense locked into lockdowns by the precedent set and the public expectation that any surge must be met with the same response. This is another pitfall of single-criterion thinking: it can lead to policy inertia where one keeps doubling down on the same approach because the framework does not allow considering alternatives.
In summary, single-criterion thinking in the pandemic led to disproportionate responses: measures that were extreme relative to their diminishing benefit. This captures the self-defeating nature of an overly narrow strategy. By focusing only on shortterm fatalities as the only criterion considered, one might cause long-term fatalities through other pathways, thereby defeating the broader goal of saving lives. The challenge, then, is how to restructure decision making toward a multicriteria paradigm, which the final section will discuss.
Toward Multicriteria Thinking in Future Crises
The lessons from the Swedish experience and other countries’ missteps point to a clear recommendation: future pandemic responses (and crisis responses in general) should adopt a multicriteria decision making framework as standard. This means that instead of one single metric guiding policy (like daily or weekly infections or deaths), a set of relevant criteria is jointly considered and weighed when choosing interventions. Such criteria should reflect the diverse domains of impact, including direct health outcomes both from the disease in question and other health issues, economic conditions, education, mental health, civil liberties, and social equity. Decision-makers should employ tools from decision science, such as MCDA, to evaluate policy options on multiple fronts.
MCDA is since long being used in various fields, not least in policymaking such as environmental policy (balancing economic development vs. environmental protection vs. social impact) and healthcare resource allocation (e.g., weighing cost, efficacy, and equity of treatments). Applying it to pandemic policy would have involved steps such as identifying all major objectives, developing metrics or indicators for each, assessing how different interventions score on each objective, and possibly assigning weights to reflect priorities or societal values. Importantly, it also involves engaging diverse experts and stakeholders so that all perspectives (medical, psychological, economic, ethical, etc.) inform the deliberation.
In practice, how might this look? One approach is to establish a pandemic task force that is inherently multidisciplinary. Instead of just virologists and epidemiologists, it would include economists, sociologists, child development specialists, mental health professionals, ethicists, and representatives of vulnerable groups. This broader committee would issue recommendations that explicitly discuss trade-offs. For example, if considering closing schools to curb viral spread, the committee’s analysis would include not just the estimated reduction in COVID cases, but also the projected loss in educational attainment and mental health outcomes for children, and perhaps even quantify expected future life expectancy loss due to educational setbacks (since education level correlates with long-term health and longevity). A multicriteria scorecard might show that closing schools scores well on infection control but very poorly on education and mental health, whereas keeping schools open with precautions scores moderately on both infection control and education. Policymakers could then choose the option that yields a better overall balance, likely the latter. This systematic approach contrasts with the ad-hoc way in which many policy decisions were made, under pressure, during COVID-19. But being under pressure is not an excuse, it is a reason for bringing in ever-stronger decision-analytic tools.
There are already some proposals for formal frameworks. The author has, together with colleagues, participated in several projects aiming at multi-dimensional COVID-related decision making at the national policy level. One project proposed an MCDA model for evaluating mitigation measures, highlighting the need to consider criteria like healthcare capacity, public compliance, economic cost, and social well-being at the same time (Ekenberg et al., 2021). Another study discussed a riskbased decision framework for pandemics that includes societal and economic dimensions, not just epidemiological ones (Ekenberg et al., 2021). A third project suggested a policy for Jordan (Ekenberg et al., 2022). The same team wrote the national policy for Botswana (unpublished), which unfortunately was not followed through, as single-criterion political reasoning took over. Comparative studies of Sweden, Romania, Jordan and Botswana (Danielson et al., 2022b; Ekenberg, 2021) confirm the need for a more formal policy-analytic approach, which was then developed in a European Union project under the COSC Fast Track Funding and subsequently recommended as best practice in the EU by the European Open Science Cloud (Danielson et al., 2022). The framework uses scenarios and weighting to handle the uncertainty and value judgements inherent in such decisions. A multicriteria approach is also consistent with the principle of proportionality in public health. It means that the intrusiveness of a measure should be justified by the scale of the threat and balanced against the measure’s expected benefits. If an intervention causes more harm than the harm it seeks to prevent, it fails the proportionality test. Ensuring proportionality naturally requires considering multiple harms and benefits, not just one. Many critics of strict COVID measures argued they were disproportionate. For instance, banning outdoor activities might only marginally reduce the spread since outdoor transmission is minimal, yet it has a major cost to wellbeing, thus not being proportionate. Wearing masks outdoors was more of a political invention than a transmission-reducing one since the virus, even in the form of aerosol drops, is quickly dispersed in outdoor environments. A multicriteria analysis would catch this imbalance because the cost in one criterion (wellbeing) would significantly outweigh the marginal gain in another (infection control).
Institutionalising Multicriteria Thinking
It is not enough to know in hindsight; structures must be in place beforehand. One idea is that national pandemic plans and the WHO’s guidance should explicitly incorporate multicriteria objectives. Currently, pandemic preparedness plans often focus on how to ensure healthcare can cope and how to contain the pathogen. These plans should be broadened to ensure the continuity of essential services (like schooling), safeguarding of mental health, and maintenance of civil liberties to a reasonable extent. If such goals are built into plans, then when a crisis hits, officials are reminded that their job is not only to minimise infections but also to keep society functioning in a broader sense.
Another mechanism is requiring impact assessments for any major public health order. Just as big construction projects require environmental impact assessments, one could mandate that before, say, ordering a lockdown or closing schools, the government must publish an assessment of the likely economic, social, and health impacts of doing so, as well as of not doing so. This forces a comparison on multiple grounds. During COVID, decisions were often rushed, but even a rapid assessment noting “This measure may prevent X deaths over Y months but will likely cost Z jobs and disrupt education for W million children” would have provided more context for policymakers and the public.
Public Communication and Narratives
Multicriteria decision making could also extend to how leaders communicate in crises. Instead of one-dimensional slogans (such as “zero COVID” or “whatever it takes”), messaging could transparently acknowledge trade-offs and rationale. One reason Sweden maintained public trust is arguably because their officials spoke to citizens as adults, acknowledging uncertainties and asking for compliance in a voluntary manner. In some other countries, leaders resorted to fear-based messaging to ensure compliance, which heightened the sense of singular focus on the virus. A more measured communication could say: Our goal is to protect health in the broadest sense. We must shield those at risk from the virus while also protecting our children’s education and mental health. Thus, we will take these steps and avoid those steps, because we judge this course best for overall well-being. Such honesty can earn trust and also manage expectations, while it is of course not easy to convey. But if people understand the multifaceted goals, they may better appreciate why certain sacrifices are or are not asked of them.
Global and Equity Considerations
It is also important to consider that single-minded policies had different impacts across different groups. For example, lockdowns were a luxury of the affluent (who could work from home) while many lower-income workers lost jobs or had to expose themselves anyway as essential workers. School closures hurt disadvantaged children far more than well-off children who had better remote learning resources. So, a multicriteria approach is inherently more equitable because it does not sacrifice one group (e.g., children or the poor) for the benefit of another exclusively. It treats societal well-being as a whole. This is aligned with the principle of distributive justice in health policy: burdens of policies should not fall unnecessarily unfairly on certain groups. In retrospect, one could argue that the burdens of aggressive COVID suppression were not equitably distributed. Sweden’s milder approach, by keeping society largely open, possibly avoided some of those inequities (though Sweden did suffer higher early nursing home deaths, an inequity in itself, hitting the frail elderly).
Flexibility and Iteration
A multicriteria framework is not static; it should be dynamic and updated as new information comes in. Early in COVID, one justification for lockdowns was to buy time to learn about the virus. By the summer of 2020, we knew more. For in-stance, that outdoor spread was rare, that masks might help indoors and that the elderly were at high risk while children were at very low risk for severe outcomes. A multicriteria approach would iterate: perhaps initially you weigh infection control highly because of worst-case fears, but as you learn the infection fatality rate is lower than feared for most people, you might reduce the weight on that and increase the weight on restoring normal life. It appears some countries did not effectively rebalance their strategy as knowledge improved; they got stuck in one mode. Sweden’s approach, interestingly, did adjust in some ways. When evidence emerged in late 2020 that masks could actually have some limited benefit in crowded indoor settings, Sweden updated its guidelines to recommend masks on public transport during rush hours (though late and not strongly enforced, it showed flexibility). In many countries, though, the concept of masks was misused as a political sign of efficacy. It is well documented that properly constructed and tightly fitted masks provide protection for individuals who are regularly exposed to newly infected people emitting virus-laden droplets. These droplets, typically larger than 5 micrometres in diameter and transmitted over short distances (less than 1.5 metres), can be effectively blocked by high-quality masks. In contrast, low-cost generic masks with loose or inconsistent fit offer minimal protection against viral spread, though they may carry symbolic or political significance. Importantly, such masks are largely ineffective against aerosol transmission, which involves smaller particles (less than 5 micrometres) that can travel beyond 1.5 metres. This distinction guided Sweden’s public rules of thumb, which targeted maintaining distance in indoor public spaces rather than unreflective universal masking. Even so, there were exceptions. On domestic flights, for instance, masks were required, reflecting the authority of airlines to enforce their own regulations. However, this requirement had limited practical impact, as the droplet-sized particles that masks are designed to block were already being caught by the standard HEPA filter systems used in aircraft ventilation. When vaccines arrived, Sweden moved quickly to vaccinate the elderly (achieving high uptake) and then gradually phased out even its mild restrictions by mid-2021, albeit to reinstate some restrictions in December 2021 when facing the fast spread of the Omicron variant. Those were phased out when COVID-19 was downgraded from a pandemic in March 2022. However, other countries more frequently and with less deliberation oscillated between extreme lockdowns and then sudden liftings, rather than deliberated transitions guided by multiperspective analyses.
The Next Disaster
While this article focuses on pandemics, the argument extends to any large-scale crisis. Whether it is a pandemic, a climaterelated disaster, or a security threat, policymakers face multiple objectives and uncertainties. The experience of COVID-19 is a case study of the importance of maintaining breadth of perspective. Governments and international bodies should welcome the lesson.
Some are starting to acknowledge it. For instance, some public health leaders cautioned against repeating school closures given the harm done previously. The phrase “we must learn to live with the virus” began to replace “crush the virus now at all costs,” implicitly moving towards multicriteria thinking since living with the virus means balancing normal life with disease control. The key is to institutionalise these lessons so that initial responses to the next crisis are more measured and well-prepared.
Sweden’s outcome supports the idea that a well-considered, moderate approach can outperform more heavy-handed ones. It demonstrates that multiple goals can be pursued simultaneously. It is possible to keep society reasonably open and protect the most vulnerable lives, rather than viewing it as an either/or situation. However, it is important to avoid the simplistic takeaway that lockdowns never work or do nothing, and all will be fine. That is not what research shows or MCDA approaches preach. The real lesson is about balance and wisdom in policy. Partial lockdowns and restrictive measures were an understandable first reaction to a dire situation, but they overshot because they were not continually evaluated against all harms. The lesson is to continuously evaluate policies. Use multiple criteria to decide, and aim for strategies that are robust across many goals, not just excellent at one goal and disastrous at others. One concrete step could be developing an index of pandemic response that incorporates health, economic, and social indicators, something like a pandemic resilience index. Governments could track their performance on this composite index, not just on virus case counts. That would help keep a balance. For instance, if closing businesses improves one part of the index but crashes another, the net index might show it is not beneficial.
In conclusion, the Swedish example during COVID-19 makes a compelling case that multicriteria frameworks should become a standard tool in managing public health crises. Had such frameworks been in place globally in 2020, we might have seen much more nuanced policies: targeted protections for the vulnerable, moderate social distancing, voluntary measures, and keeping low-risk sectors running. And also, potentially a better overall outc ome in terms of lives saved and lives lived. Going forward, institutionalising this approach is not just an academic ideal but a practical necessity. It can help ensure that in the face of the next pandemic, or any comparable crisis, we remember to ask not only “How do we stop this virus?” but also “What do our actions mean for society as a whole, and how do we choose a path that safeguards our collective well-being in the broadest sense?” By having the courage to consider multiple criteria, policymakers can avoid the tunnel vision that leads to unintended harm, making responses both more effective and humane.
Conclusion
The COVID-19 pandemic has been a monumental test of governance and public policy under uncertainty and stress. Sweden’s journey through this crisis, marked by an atypically light-touch response and culminating in Europe’s lowest excess mortality rate, provides a valuable case study in the importance of broad-based decision making. Initially condemned by many, Sweden’s strategy ultimately achieved results that force us to question many assumptions about pandemic management. This article’s analysis shows that Sweden’s outcomes (low overall mortality under reasonably preserved societal functions) were not miraculous or purely luck, but tied to conscious choices embedded in its policymaking structures. By relying on expert agencies and adhering to a holistic view of public health, Sweden implicitly prioritised multiple criteria: protecting life and maintaining quality of life. In contrast, many countries adopted a one-dimensional focus on the virus, implementing draconian restrictions that, while well-intentioned, often overshot the mark and inflicted collateral damage that in some respects rivalled the harm of the virus itself.
The evidence from our six papers spans epidemiological data, economic indicators, educational research, and mental health studies. It consistently supports the notion that an exclusive concentration on minimising COVID-19 transmission, contraction and deaths without equal regard for other aspects of well-being led to suboptimal policy outcomes. Countries that imposed the harshest measures often did not significantly outperform others in terms of saving lives when looking at the full timeline, and they paid a steep price in other domains. Meanwhile, Sweden’s more balanced approach did not result in the mass casualties that critics predicted. Instead, Sweden ended the pandemic period with fewer excess deaths per capita than almost any peer (Norway is a nonEU exception), an outcome that seemed almost inconceivable to many observers back in 2020. This does not mean Sweden did everything perfectly, far from it. There were acknowledged major failures, particularly in elder care in the first wave where the elderly as a group were severely let down, but the overall strategy proved reasonably sound in mitigating total harm.
A key argument emerging from this analysis is the need to revamp how we approach crisis decision making. MCDA is not just a theoretical ideal but a practical framework that would have led to better policy decisions in this pandemic, and if adopted, can lead to better decisions in the future. By systematically evaluating trade-offs such as weighing lives saved from the virus against life years lost elsewhere and balancing disease control against societal function, leaders can aim for policies that are proportionate and sustainable. The pandemic has vividly illustrated that society’s wellbeing is a tightly coupled system: health, economy, education, and freedom are very interconnected. Neglecting any one dimension can cause harm to others. Thus, the only rational way to govern in a crisis is to consider all these dimensions together.
Honouring a multicriteria approach will require changes: institutional (bringing more diverse expertise to the table), cultural (resisting panic and simplistic narratives), and procedural (mandating impact assessments and transparent deliberation about trade-offs). It also requires humility and political courage, acknowledging that no single metric, however important, captures all that matters, not even on election day. The COVID-era mindset of tracking the daily death toll like a scoreboard, while understandable in a deadly pandemic, should be exchanged the next time for a multi-faceted view on public health and well-being. Excess mortality, ironically, is one such wider metric and it told a very different story than the daily COVID death counts did. Excess mortality revealed that the countries that seemed to be losers by COVID deaths in 2020 (like Sweden) had, by mid-2022, not lost more lives. Countries that “won” early by quenching the curve had those deaths occur later, together with several other unintended consequences.
As a conclusion, it is perhaps fitting to recall an essential insight of policy analysis: correlation is not causation, and intentions do not equal outcomes. Many nations intended only to save as many lives as possible the next day and were willing to impose severe measures to do so. Sweden intended to play the longer game by safeguarding public health in a broader sense by avoiding severe measures. In the end, Sweden’s approach may have saved more lives (when considering overall excess deaths) precisely because it averted some of the unintended health consequences of strict lockdowns, while still managing to protect most of those at risk from COVID after the initial wave. This suggests that a rational, measured response might outperform a single-criterion maximalist response. It also highlights the importance of learning from empirical outcomes rather than judging policies solely on their intent or initial appeal.
No doubt, debates will continue for years about the efficacy and ethics of various pandemic interventions. There will be national commissions in every country, trying to find out what actually happened and who to blame. In Sweden, the Royal Academy of Sciences published its final report already in November 2021 (KVA, 2021) after having published six intermediate reports during the ongoing pandemic. Ironically, ten days later, the Swedish government proposed new restrictions amidst the threat from the Omicron BA.2 strain (Danielson, 2022b). A month and a half earlier, in October 2021, the Swedish corona commission evaluated the measures taken by the government, administrative authorities, county regions and municipalities to limit the spread of the virus and the effects of the spread (Corona kommissionen, 2021). So, from a Swedish perspective, the society collected the information that was to be collected and drew the conclusions that were to be drawn, at least from a governmental point of view. While many other countries’ aftermath documents will surely follow, the Swedish perspective has, at the time of writing in August 2022, already been officially investigated and its conclusions documented.
This article does not claim that there was an easy policy process standing by that everyone missed. Every country faced difficult decisions with limited information. Rather, the aim here has been to synthesise available information to argue that, on balance, a more nuanced, multi-faceted approach was superior to an extreme, single-minded one. Sweden’s case is evidence of that. But even beyond Sweden, a few studies and some experts have started to discuss the view that full lockdowns and similar measures should be a last resort in the future, not a first response, given their broad societal costs. The ultimate goal should be to refine our crisis response preparations to be smarter and more balanced the next time.
In closing, the COVID-19 pandemic taught humanity a great deal about virology and science processes in general, about the interconnected world, and about values. If we narrow our vision to one dimension of a problem, we risk solving that one aspect but creating a host of new problems. A multiple-criteria framework helps keep our eyes on all the things that matter. Sweden’s pandemic experience, culminating in both low excess mortality and lesser societal disruption, illuminates the potential benefits of such an approach. This is not to say that Sweden had such an explicit policymaking process or that it was optimal. Far from it, the multiple perspective process is in the Swedish culture but could have been used to a much larger extent, had a more formal decision-analytic process been followed, as recommended by the European Union (Danielson, 2022). As uncomfortable as it may be for governments that poured all efforts into one-dimensional strategies, the global community must assess and learn from these outcomes. Doing so will not downgrade the efforts and sacrifices made; rather, it will honour them by ensuring we do much better the next time.
By adopting multicriteria decision analysis as a standard process for future public health (or other) crises, we can aim to protect lives effectively while also maintaining society. The next time we face a novel virus or similar threat, let us remember the Swedish example and the conclusion that a balanced approach can achieve the best overall results. Our goal should be to minimise total harm, not just the harm from the most obvious source. In effect, the lesson should be to keep the big picture in view, an approach that might well save both lives and livelihoods when it matters most.
Acknowledgement
This work was funded by the European Open Science Cloud, Covid-19 Fast Track Funding, grant agreement number 831644.
References
- Allen DW (2021) Covid Lockdown Cost/Benefits: A Critical Assessment of the Literature.
- Amanat F, Krammer F (2020) SARS-CoV-2 vaccines: Status report. Immunity 52: 583-589.
- Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF (2020) The proximal origin of SARS-CoV-2. Nat Med 26: 450-452.
- Betthäuser BA, Bach-Mortensen AM, Engzell P (2022) A systematic review and meta-analysis of the evidence on learning during the COVID-19 pandemic. Nat Hum Behav 7: 375–385.
- CDC (2022) CDC Media Telebriefing: New CDC data illuminate youth mental health threats During the COVID-19 pandemic.
- Coronakommissionen (2021) Sverige under pandemin: Volym 1 och 2 (SOU 2021:89). Statens offentliga utredningar. [in Swedish].
- Danielson M, Ekenberg L, Komendantova N, Mihai A (2022) Evidencebased methods for the development of computationally supported epidemic-combating policies. In H. Fujita, & A. Selamat (Eds.), New trends in intelligent software methodologies, tools and techniques 355: 363–373.
- Danielson M, Ekenberg L, Komendantova N, Mihai A (2022b) A riskbased decision framework for policy analysis of societal pandemic effects. Front Public Health 11: 1064554.
- DN (2020, March 26). Forskare i upprop till regeringen. Dagens Nyheter. [Researchers appeal to the government, in the largest Swedish newspaper]. [in Swedish].
- Ekenberg L, Mihai A, Fasth T, Komendantova N, Danielson M (2021) A multicriteria framework for pandemic response measures. Front Public Health 9: 583706.
- Ekenberg L, Mihai A, Fasth T, Komendantova N, Danielson M, et al. (2022) A Multicriteria Approach to Modelling Pandemic Response under Strong Uncertainty: A Case Study in Jordan. Sustainability 14: 81.
- Ekenberg L, Mihai A, Fasth T, Komendantova N, Danielson M, et al. (2021b) Mitigating cognitive and behavioural biases during pandemics responses. In D. C. Morais, L. Fang, & M. Horita (Eds.), Contemporary issues in group decision and negotiation: GDN 2021 (Lecture Notes in Business Information Processing, Vol. 420, pp. 45–56). Springer.
- Ekenberg L, Fasth T, Komendantova N, Koulolias V, Larsson A, et al. (2022b) A framework for COVID-19 pandemic intervention modeling and analysis for policy formation support in Botswana. International Journal on Advances in ICT for Emerging Regions, 15: 3–20.
- Ferguson NM, Laydon D, Nedjati-Gilani G, Imai N, Ainslie K, et al. (2020) Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and health¬care demand (Imperial College COVID-19 Response Team Report No. 9). Imperial College London.
- Hale T, Webster S, Petherick A, Phillips T, Kira B (2020) Oxford COVID-19 government response tracker. Blavatnik School of Government, University of Oxford.
- Hallin AE, Danielsson H, Nordström T, Fälth L (2022) No learning loss in Sweden during the pandemic: Evidence from primary school reading assessments. Int J Educ Res 114: 102011.
- Kavaliunas A, Ocaya P, Mumper J, Lindfeldt I, Kyhlstedt M (2020) Swedish policy analysis for COVID-19. Health Policy Technol 9: 598– 612.
- Kungliga Vetenskapsakademien (KVA) (2021) Vad kan vi lära av pandemin? Kunskapsöversikter från Kungl. Vetenskapsakademiens expertgrupp om Covid-19 (30 november 2021). Kungliga Vetenskapsakademien. [in Swedish].
- Nussbaumer-Streit B, Mayr V, Dobrescu AI, Chapman A, Persad E, et al. (2020) Quarantine alone or in combination with other public health measures to control COVID-19: A rapid review. Cochrane Database Syst Rev 2020: CD013574.
- Walker PGT, Whittaker C, Watson OJ, Baguelin M, Ainslie KEC, et al. (2020). The global impact of COVID-19 and strategies for mitigation and suppression (Imperial College COVID-19 Response Team, Report No. 12). Imperial College London.
- Business Insider (2020) Taiwan has only 77 coronavirus cases.
- Global Health Security Index (2020).
- Muttarak R (2020) Explaining the COVID-19 outbreak and mitigation measures.
- The New York Times (2020) Embracing the Uncertainties.
- Time (2020) The National Divide Over COVID-19 Testing Threatens Our Progress.
- UNESCO. (2020). Adverse consequences of school closures.
- WHO (2022) COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.