CORHD Lesions: A New Pediatric Terrible Triad of the Elbow. A Case Report and Literature Review
STUDY AND RESEARCH GROUP IN TRAUMA AND PEDIATRIC ORTHOPAEDICS – CONSTANȚA 2021
Gheorghe Burnei1*, Mioara Georgescu2, Florin-Daniel Enache3
1Professor of Pediatric Orthopedics, Macta Clinic Constanta, Tinos Clinic Bucharest, Romania
2“Sf. Apostol Andrei” Constanta Emergency County Hospital, Romania
3“Ovidius” University of Constanta, Faculty of Medicine; “Sf. Apostol Andrei” Constanta Emergency County Hospital, Romania
*Corresponding author: Gheorghe Burnei, Professor of Pediatric Orthopedics, Macta Clinic Constanta, Tinos Clinic Bucharest, Romania
Received Date: 20 September 2022
Accepted Date: 23 September 2022
Published Date: 26 September 2022
Citation: Burnei G, Georgescu M, Enache FD (2022) CORHD Lesions: A New Pediatric Terrible Triad of the Elbow. A Case Report and Literature Review. Ann Case Report 7: 962. DOI: 10.29011/2574-7754.100962
Abstract
Background context: The osteoarticular pathology of the elbow includes a number of complex lesions, the best known being the Monteggia fracture-dislocation, the anterior Trans olecranon fracture-dislocation and the terrible triad of the elbow. The diagnosis and treatment of these injuries require the medical practitioner to have solid knowledge to establish an early diagnosis and optimal treatment in order to fully recover the elbow function. When faced with a novel case involving complex lesions that cannot be included in the known pathology, the orthopaedist needs to use conceptual reasoning to make a detailed analysis of the historical data and previously-described associated lesions, and then compare them with those under study.
Purpose: To present a novel case and identify its place within the complex elbow injuries. The current case report can help orthopaedic and trauma surgeons to identify this rare and complex lesion.
Study Design/Setting: Each lesion was identified and interpreted. Analysis in the context of scientific data was performed after each investigation and for each lesion or lesion group described in the literature. The evaluation confirmed or denied each condition.
Patient Sample: A 12-year-old male patient presented to the Emergency Unit with a traumatic elbow and was immediately hospitalized. He was clinically examined and explored by radiology and imaging. Three lesions difficult to include in the known pathology were identified.
Outcome Measures: Each diagnostic stage was evaluated based on both the accumulated knowledge and literature review. The final diagnosis was established step by step, after which the patient underwent surgery.
Methods: The presence of an elbow showing obvious clinical signs of a major impact and an apparently harmless radiological aspect known as TRASH (The Radiographic Appearance Seemed Harmless) suggested possible osteochondral lesions. Special attention was paid to radiological and imaging details. The data revealed by these investigations were compared with those in the literature and it has emerged that a new terrible triad is in question.
Results: Surgical intervention ensured the firm stabilization of fractures and checked the stability of the reduced radial head in the annular ligament strap. Early mobilization allowed the recovery of flexion and extension; at the 60-day postoperative control, elbow mobility was normal.
Conclusion: There are multiple known or potential complex elbow injuries in children. All these lesions must be early diagnosed through imaging exploration and impeccably treated, and the elbow must be mobilized from the first postoperative days.
Keywords: Child; CORHD lesions; Multiple osteochondralarticular TRASH lesions; Coronoid fracture; Olecranon fracture; Distal and posterior radial head dislocation; Intact annular ligament; Typological classification of Monteggia fracture- dislocation
Introduction
Difficult and rare cases have raised special interest among medical practitioners. Complex lesions are a serious challenge and, for a correct attitude, physicians must systematically analyse their knowledge and own experience to establish the diagnosis and suitable treatment for each case. TRASH lesions are relatively rare and difficult to identify at the initial examination. The management of these fractures is not well defined in the existing literature [1]. Imaging should be used to better visualize fracture fragments, establish a more accurate diagnosis and guide surgical strategy. Computed tomography (CT) scanning has the advantage of being easily available and useful for children aged 12 years or older, as illustrated by this case. Contrast- enhanced MRI (magnetic resonance imaging) pictures are more relevant because they provide concrete data about cartilage areas.
Case Report
Diagnosis
A 12-year-old male patient presented to the Emergency Unit with a traumatic elbow. Anamnestic ally, the parents found out from those present at the scene of the accident that the patient had suffered a trauma by falling from about 1 m, leaning on the palmar face of the hand and then on the elbow. Local physical examination showed swelling, the elbow in antalgic flexion and total functional impairment. No characteristic signs of vascular or nerve damage were detected. Two radiological images are captured and both highlight posterior radial head dislocation and an elbow with a veiled joint space [Figure 1]. As a matter of urgency, posterior reduction of the radial head is performed. A control x-ray examination shows reduction of the radial head and the presence of a suspected Salter-Harris type II radial head fracture or a chondrospongious lesion of the capitellum or coronoid [Figure 2]. As such, imaging exploration is decided. Considering the imaging equipment of the local medical unit where the patient presented and the fact that all elbow ossification centres appear up to the age of 12, CT and 3D-CT are performed. Images indicate reduction of the radial head, thus confirming the presence of the olecranon fracture with several comminute particles, and identify the chondrospongious avulsion as a coronoid fracture [Figure 3]. The presence of the three lesions and the need for early mobilization of the elbow required surgical intervention with a view to perform the anatomical reduction of fractures, firmly stabilize them and check the stability of the dislocated and reduced radial head. Mobilization from the first postoperative day required either the integrity of the round ligament or its reconstruction by ligamentoplasty.
Surgical intervention
The posterior trans olecranon approach confers a major advantage in exploring the elbow joint. The presence of the olecranon fracture in this case allowed not only the anatomical reduction of fractures and their fixation (Figure 4) but also the identification of comminute particles as potential centres of heterotopic ossification, the evaluation of annular and quadrate ligaments, the testing of radial head stability through pronationsupination movements (Figure 5) and the detection of lesions caused by dislocation of the radial head. The quadrate ligament was partially torn but the annular one had no macroscopically detectable lesions. The coronoid fracture involved the chondral surface of the distal trochlear (coronoid) compartment to which a 0.1-0.5 cm cancellous layer and a metaphysical portico-cancellous fragment from the anterior surface of the metaphysis were attached. The fragment was displaced ventrally and laterally. It was anatomically reduced and stabilized with two Herbert screws placed divergently in areas with better chondrospongious thickness. The olecranon fracture was firmly reduced and fixed with a figure-of-eight wire. A small chondral defect on the common line of the two fractures was left free. A brachial-palmar plaster splint was applied, which was removed on the 5th day. The subsequent intensive recovery allowed the patient to fully regain elbow mobility within 60 days (Figure 6).
Discussions
The presence of posterior radial head dislocation that is evident on two radiological images in different incidents imposed by the antalgic attitude and generated by a traumatic elbow suggests either an isolated radial head dislocation or a Bade type IIB Monteggia fracture- dislocation. The elbow image provided by these radiographs can be included in TRASH lesions, meaning that they do not offer conclusive pictures for the presence of obvious lesions, and the elbow is apparently intact. The presence of posterior radial head dislocation required orthopaedic reduction, which was performed two hours after the accident. Both control radiographs revealed the reduction of dislocation and a lamelliform fragment on the front view x-ray, which appears to be a Salter-Harris type II radial head fracture that might have been produced because of forced reduction or a laterally displaced coronoid fracture. The radiological image taken through the cast does not allow identification of other lesions. In order to clarify the absence or presence of other lesions associated with the posterior dislocation and establish the origin of the intra-articular fragment, the imaging investigation of choice is MRI, preferably with the contrast substance. CT and 3D-CT were used, considering the equipment of the medical unit where the patient presented and the fact that all elbow ossification centres appear up to the age of 12. CT images confirm the reduction, identify the intra-articular fragment as a coronoid fracture and highlight an olecranon fracture. The predictably osteochondral coronoid fracture requires surgery even if the dislocation has been reduced and the olecranon fracture is not displaced. 3D-CT images reveal a coronoid flap fracture involving the entire distal trochlear compartment. To establish the complete diagnosis, the orthopaedic specialist goes through several stages. In a first stage, the radial head dislocation is evident, and the question is whether it is an isolated dislocation or a Monteggia fracture- dislocation.
Traumatic radial head dislocation in children
The patient was treated per primal as having a radial head dislocation. Isolated radial head dislocation in a traumatic context is exceptional [2] and has the highest incidence in children, being often associated with ulna fractures [3]. The exceptional occurrence of isolated dislocations is also revealed by their lack of description in the literature. The management of recent radial head dislocation in children is non-operative. Surgical treatment is used only for irreducible dislocations. Isolated radial head dislocation can be caused by distant trauma without apparent ulnar damage, which is why it is confused with congenital radial head dislocation. It can be an anterior, posterior or lateral dislocation either through rupture of the annular and quadrate ligaments or as a distal dislocation of the head if the quadrate ligament is intact or partially torn. Total rupture of the quadrate ligament causes anterior, posterior or lateral displacement of the head. In the studied patient, the annular ligament was intact. An isolated radial head dislocation was operated on when the patient presented for treatment 21 days after the trauma, given that the control x-ray had indicated instability of the dislocation. The intervention with rigorous dissection allowed the annular ligament individualization and repositioning in the radioulnar joint by telescoping the head [4]. The reduction manoeuvres, which were strictly addressed to the radial head displaced distally and then posteriorly, were performed early, two hours after the trauma, under general anesthesia. Closed repositioning was followed by immobilization in a brachial-palmar plaster splint with the forearm in supination and flexed at 90 degrees. After reducing the radial head dislocation, a careful exploration of the ulna was indicated to confirm or deny the presence of a Monteggia lesion. To confirm an isolated lesion, the ulna must appear intact. In this context, the dislocation would have been produced by ulnar bowing because of its flexibility [5] or would have been caused by an occult ulnar fracture [2] that had to be illustrated by a careful radiological examination. Isolated radial head dislocation was first described by Devaney in 1751 [6] and, until 2004, only 84 cases were reported in the literature [7]. The diagnosis of dislocation was established based on clinical and radiological exams performed in emergency conditions. The control radiograph after reduction was expected to rule out a Monteggia lesion or congenital dislocation. Isolated traumatic radial head dislocation may have been missed during the initial evaluation [8] if elbow positioning at 90 degrees or in maximum extension had been attempted. A traumatic elbow lesion raises the suspicion of radial head dislocation [9]. Clinical and radiological exams must be aimed at confirming or denying the presence of radial head dislocation [10]. The occurrence of an isolated traumatic radial head dislocation is controversial because it is more commonly associated with the ulna fracture, which is described as a Monteggia fracture-dislocation. The dispute regarding its isolated existence has as supporting arguments the elasticity of osteoarticular structures in children and the existence of undiagnosed or hard-to-detect occult ulnar fractures.
In the studied case, the orthopaedic treatment reduced the radial head, and the intraoperative exploration revealed that it was anatomically arranged, circumscribed by the intact annular ligament and with normal mobility when testing pronation and supination movements (Figure 7). An isolated radial head fracture was ruled out when the control radiograph, performed after orthopaedic reduction of the dislocation, highlighted an intraarticular lesion that could be a Salter-Harris type II radial head fracture or coronoid fracture, and the suspicion of an olecranon fracture (Figure 8) was confirmed by the CT examination. In isolated anterior, posterior and lateral dislocations, a complete radial head dislocation cannot occur without the complete rupture of the annular ligament, which is the main stability factor for the proximal radioulnar joint. The integrity of the annular ligament, it either is associated or not with the quasi-total or partial rupture of the quadrate ligament, shows that, in biomechanical terms, a distal “downward” dislocation of the radial head has occurred [4]. Plasticity of the ulna allows bowing and may cause the radial head dislocation [9] without the occurrence of an ulnar fracture or the detection of a periosteal reaction or an anterior, posterior or medial curvature [11]. This form of dislocation, also known as “painful
pronation”, is extremely rare in older children [12] but is common in young children aged between 1 year and 6 months and 5 years. The radial head reaches under the annular ligament by pulling the hand in pronation, and the bicipital tuberosity is hooked behind the posterior crest of the ulnar sigmoid cavity. For isolated traumatic radial head dislocation with annular ligament tear in children, surgery should be the treatment of choice by open reduction and annular ligament reconstruction. To ensure the stability of the reduced radial head, some authors have supported the use of ligamentoplasty in all cases requiring open surgery [13-15]. An isolated radial head fracture was ruled out when the control radiograph, performed after orthopedic reduction of the dislocation, revealed the sign of a possible olecranon fracture and an intra-articular lesion that could be a Salter- Harris type II radial head fracture or coronoid fracture (Figure 9).
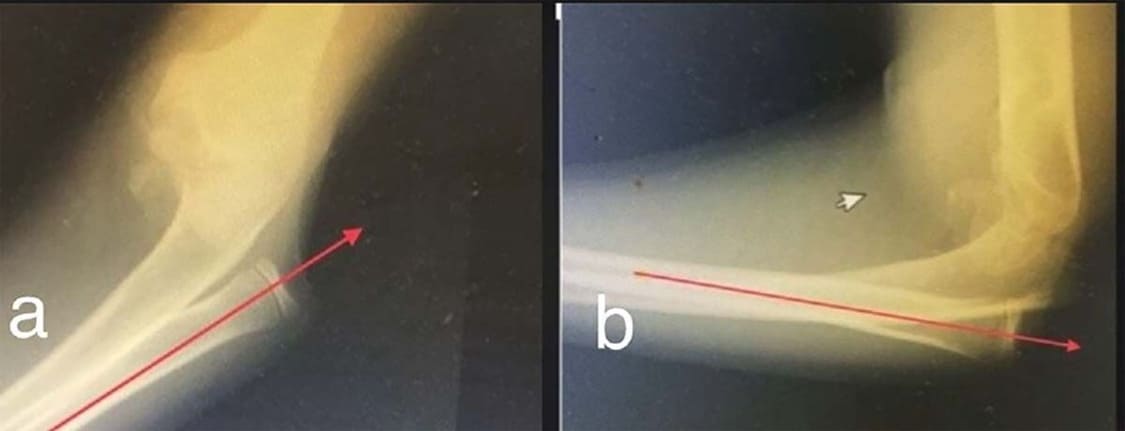
Figure 1: Elbow radiograph in two different incidents. Front and lateral standard images could not be obtained due to the patient’s antalgic attitude and agitation. In this situation, only sedation or anaesthesia allows capturing standard images. Posterior radial head dislocation is evident in both pictures. TRASH injuries are suspected at the elbow.

Figure 2: The control radiograph taken through the cast shows reduction of the radial head and suggests an ulnar fracture and three possible lesions: Salter-Harris type II radial head fracture, capitellum fracture or coronoid fracture.
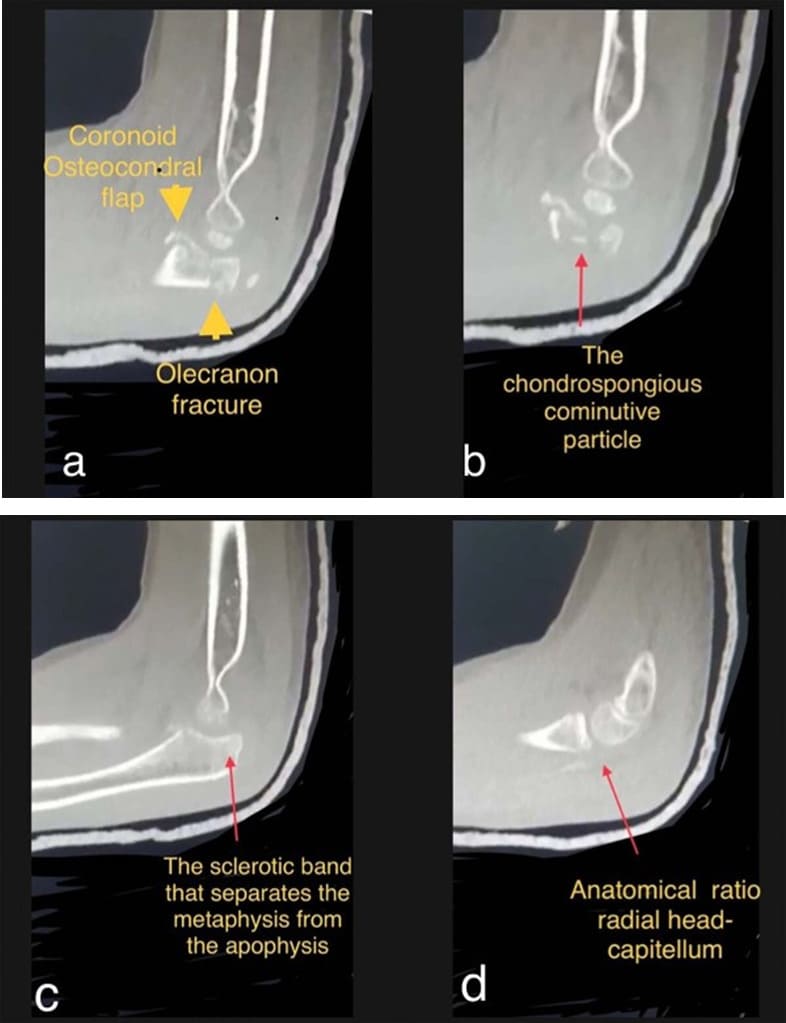
Figure 3: CT images confirm the olecranon fracture and identify a coronoid fracture. a) The characteristic appearance of the paediatric coronoid fracture; the chondral flap involves the entire distal trochlear compartment. b) The comminute particle at the junction of the two fractures. c) The sclerotic area of least resistance; the olecranon fracture crosses this area. d) Radial head dislocation was reduced.
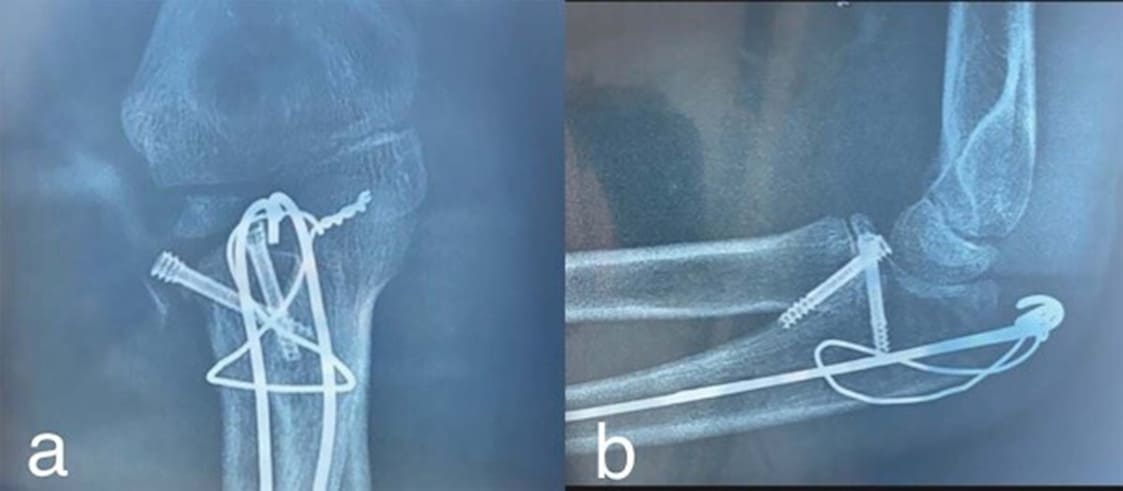
Figure 4: Anatomical reduction of fractures and fixation of the coronoid fracture with two Herbert screws and the metaphysical olecranon fracture with a figure-of-eight wire

Figure 5: Intraoperatively, the radial head stability was checked; the annular ligament was normal, and the radial head was stable in flexion-extension and pronation- supination.

Figure 6: At the 60-day postoperative control, elbow flexion and extension were fully recovered. a) extension; b) and c) flexion

Figure 7: Schematic of the archetype construction of locomotor limbs in terrestrial vertebrates

Figure 8: a) Articular compartments of the olecranon; b) Olecranon configuration responsible for the frequency of metaphysical fractures and the type of coronoid fractures

Figure 9: Comminute particles are common in metaphysical olecranon fractures. A chondrospongious particle evident on the 3D-CT image produced a 0.7/0.5 cm chondral effect recoverable through the local chondrogenesis potential.
Olecranon fracture
After the closed reduction of radial head dislocation, the control x-ray showed a possible bone discontinuity in the olecranon, which was then confirmed by CT. Fractures of the proximal end of the ulna in children and adolescents involve the metaphysis and account for 5% of all elbow fractures; the other fractures (epiphyseal and coronoid ones) are extremely rare [16]. When establishing the diagnosis, it should be taken into account that the radiographic interpretation can be confusing due to the variation in growth centres, that these fractures can often be completely missed, that the precise fracture line is difficult to determine and that the outcomes can be unsatisfactory if the displacement is not estimated. Epiphyseal fractures involve the epiphysis and growth cartilage and are extremely rare.
Growth and development are very important for a paediatric orthopaedist, who needs to integrate disparate notions into a large amount of knowledge in order to take a firm stand to establish the appropriate diagnosis and treatment. In terms of development, the proximal end of the ulna does not have a clearly defined epiphysis and metaphysis [17]. At birth, none of the articular elements of the ulna, including the coronoid and olecranon, are ossified. The secondary ossification centre appears at the olecranon around the age of 9. This ossification centre may be bipartite and eccentric, and as the proximal ulna grows, the growth plate orientation alters from transverse to oblique. These changes are determined by the transition to orthostatic and as a result of using the thoracic limbs in pretension. Thus, essential structural and functional alterations appear at the elbow, forearm and hand to amplify the exercise of human-specific pretension. The ulna has as its counterpart, at the level of pelvic limbs, the fibula. The phyllo- and ontogenetic ulnar changes from the zeugopodia to the forearm gave it a crucial role in the elbow mobility and stability through the development of the proximal end of the lateral zeugopodia of thoracic limbs in terrestrial vertebrates [18] (figure 7). The proximal configuration of the ulna confers it particular and distinct features; the articular surface of the ulna has functional connections with both the homers and radius, being the pillar around which the radius pivots during pronation-supination movements. The fibula articulates with the tibia but not with the femur. These changes occur due to the migration of the ossification centre and the physics, which leads the articular surface to come into contact not only with the epiphysis but also with the metaphysis. For more precision in surgical practice, orthopaedists nominate an articular segment in the proximal end of the ulna, which corresponds to the trochlear notch and also incorporates the radial notch. At this level, there is a more pronounced narrowing above the radial notch than at the base of the olecranon [19]. The narrowing is more difficult to identify in children due to the appearance, during growth and development, of small, non-articular and transversally arranged portions that can be detected in some people during skeletal maturation [20]. Closure of the physics begins at the articular surface and progresses toward the extensor surface of the bone. These areas are covered by narrow extensions of the synovial membrane, which contain fat particles. In a statistically unspecified group of adults, the two compartments, namely the proximal trochlear or apophyseal and distal trochlear or coronoid ones, are separated by an intercompartmental synovial recess [19] (Figure 8); in children, the two compartments have continuity. The intercompartmental limit is structurally defined by a sclerotic area that provides it with lower resistance. It is there that most paediatric olecranon fractures are located. These applied surgical anatomy data explain the frequency of certain types of olecranon fractures and the configuration of the coronoid fracture in children; a metaphysical olecranon fracture located in the sclerotic area and a predominantly cartilaginous flap involve the entire distal trochlear compartment.
Metaphysical fractures. The studied patient presented an intercompartmental metaphysical fracture in the sclerotic area. The limit between the two compartments corresponds to the ulnar metaphysis. Although the formation of the metaphysis is questionable, the ontogeny and phylogeny data show that a metaphysical segment of the ulna makes direct contact with the chondral joint. The proximal end of the fibula has no functional value. There are considerable differences in their proximal ends. The ulna, due to its apprehensibility, has developed to ensure the physical and functional support of the hand during pretension. Before the cartilage fusion, a wide sclerotic border develops in the metaphysis, which separates it from the apophasis. This sclerotic band resembles a fracture and is difficult to differentiate from it. A metaphysical fracture that involves this sclerotic area generates multiple comminute particles as potential centres of heterotopic ossification. Metaphysical fractures, although more common than epiphyseal fractures, account for only about 5% of elbow injuries. Sometimes, the recognition of a paediatric fracture requires comparative views of the opposite side. Wilkins [21] identified only 230 cases out of 4,684 paediatric fractures located in the proximal end of the ulna before 1991. The medical literature reported four large series of proximal ulnar fractures and 20% had an associated fracture. In other reports, 50% to 70% had an additional injury that most commonly affected the radial head through valgus pressure at the time of impact [16]. Trans olecranon fracture-dislocation is a complex, distinct and indissoluble lesion, which is defined as an olecranon fracture where the olecranon fragments have intangible fracture surfaces, and the elbow is dislocated anteriorly. This type of fracture- dislocation may occur in isolation or associated with other injuries. Half of the adult patients with trans olecranon fracture- dislocation also have coronoid fractures [22]. In children, the 11 cases of fracture-dislocation reported until 2020 were not associated with coronoid fractures [23-26]; one case was associated with medial epicondyle avulsion, and another case was associated with radial neck fracture. In 2020, Yamamuro [27] presents the first case with anterior trans olecranon fracture- dislocation associated with avulsion of the coronoid process in a 7-year-old boy, and in 2022, Zheng [28] presents the second case in a 7-year-old girl.
The coronoid process fracture is different in children compared to adults. In children, this fracture is an osteochondral flap. These occult fractures are rare and diagnosed late in many cases [29]. The anterior margin of the trochlear notch in children and the site of development of the coronoid apophasis have the configuration of the ulnar cortical contour. In adults, it is configured as an outgrowth of the cortical contour. The coronoid process has no secondary ossification centre. It is ossified by the metaphysis advance margin [30], which ensures the increase in thickness of the proximal end of the ulna. This helps to explain the coronoid fracture pattern observed in different age groups [16]. The fracture includes both its site of development and the metaphysis margin of advance in thickness, proximally extending with a chondrospongious flap that corresponds to the distal trochlear compartment. Distally, it invariably has a portico-cancellous bone portion that is variable in size and appears as a half-sectioned conical parallelepiped; it is actually a condor-osseous avulsion that displaces ventrally and laterally. The fragment mobilizes at elbow flexion and extension and resists a full range of flexionextension movements. This resistance, which is present at the end of the flexion-extension range of motion, is also present when flexion-extension movements are tested preoperatively, under anesthesia. This sign indicates the presence of an intra-articular foreign body that should not be insisted upon to avoid cartilage damage. We operated on four patients with coronoid fracture associated with other injuries, but we have never encountered on the site where the coronoid process is to develop, in the middle of the anterior margin of the trochlear notch, a cartilaginous or bony protuberance or excrescence in children younger than 12 years old. The radiological examination shows an injury with a seemingly harmless appearance, an image with a veiled joint space, and TRASH lesions are suspected. In reality, these lesions are well defined in imaging terms, especially on contrast-enhanced MRI, and have a grim prognosis if such fractures are associated with other osteochondral lesions and are not anatomically reduced. As a rule, the anatomical reduction of these fractures is done by open reduction and internal fixation. Similar radiologically unidentifiable TRASH lesions also occur in children, but with other chondral or osteochondral localizations at the level of the capitalism, radial head or condyles. Regan and Morrey classified coronoid fractures into three types [31] as follows: type I fractures involve the tip of the coronoid; type II fractures involve up to 50% of the coronoid process; type III fractures involve more than 50% of the coronoid process and are often accompanied by an olecranon fracture [32]. Anatomical, biomechanical and clinical studies have confirmed the usefulness of this classification in predicting outcome and determining management. Isolated coronoid fractures have no operative indication [33], but surgery is used when they are associated with other injuries [34]: elbow dislocation, radial neck or olecranon fracture, etc. In children, small fracture fragments of the coronoid process (type I and type II) are actually much larger, but their real size is not always assessed by radiography because the coronoid process contains considerable amounts of cartilage. Isolated fractures of the coronoid process in children are rare [35]. If encountered as an apparently isolated lesion, they are labelled as fractures exclusively produced by the brachial muscle avulsion or secondary to a spontaneously reduced elbow dislocation [36].
Multiple comminute particles
Metaphysical olecranon fractures with a trajectory in the sclerotic area induce bone and cartilage lacerations (Figure 9); bone lacerations form small particles of variable size. Comminute particles also generate grade III coronoid fractures. These particles are smaller in size and are disseminated when reduction and fixation are attempted. Chondral lacerations are less common and have a lamellicorn appearance. In this case, the intervention must have a distinct operative time for their detection and evacuation. In the studied patient, we extracted four bone particles and a chondral lamella. When they remain in the joints, they produce heterotopic ossifications that cause impingement with limitation of elbow mobility.
Atypical form of Monteggia type ll fracture with two atypical ulnar components?
The presence of the olecranon fracture affecting the proximal articular segment calls into question an atypical Monteggia fracture. According to Bade classification, Monteggia type ll fracture is characterized by posterior radial head dislocation and occurs in 10% of cases. In typical forms, an ulnar fracture involves the proximal diaphysis segment. Bade expands the scope and conceptualizes for the first time the “Monteggia-like lesion” phrase in practical activity. In 1967, Bade classified it into four types, according to the radial head displacement, and described the classic Monteggia lesion and equivalent or variant lesions [37]. In the original classification, Bade noted that there was no equivalent of Monteggia type II lesion other than radius dislocation after the radial head or radial neck fracture. Logically and systematically, all ulna fractures located outside the proximal diaphysis segment can constitute an atypical ulnar component in a Monteggia lesion. Similarly, radius dislocation may also include, apart from radial head dislocation as a typical Monteggia lesion, dislocation of the proximal end of the radial diaphysis secondary to a radial head or neck fracture [38] as an atypical component. Equivalent lesions are rare and occur more commonly in children. They have the same production mechanism, radiographic pattern and treatment method [38]. Jupiter classifies Monteggia type ll lesions into four subtypes, according to the level of the ulnar fracture: IIA coronoid level IIB the diaphysis metaphysical junction llC distal to coronoid llD the fracture extends into the distal half of the ulna. In the studied case, the fracture affects the joint area of the proximal end. Thus, a typical lesion is associated with an atypical one: radial head dislocation with ulnar fracture in the proximal articular segment. The two components establish an atypical Monteggia type II lesion. In 1880, Stanciulescu noted that, in the Monteggia fracture- dislocation treatment, “the reduction of dislocation is everything” [39]. Therefore, radius dislocation is the main component of the lesion, being essential not only for classification but also in establishing the diagnosis and therapeutic conduct.
Irreducible dislocation or residual subluxation can only be stabilized through meticulous surgical treatment aimed at anatomical reduction of the joint [40]. When the radiocapitellar joint was unstable, we preferred ligamentoplasty with the ligament of the extensor carpi radials longus muscle [41] or with a languet from the tendon of the biceps brachia muscle [42]. In a Monteggia fracture-dislocation, especially in atypical forms, we preferred a two-incision approach [43] to avoid heterotopic ossification or synostosis [44]. Atypical Monteggia type ll lesions are most common [45] compared to other atypical forms. Other atypical forms of Monteggia type ll fracture-dislocation in children have also been described [46]. In medical practice over time, for more than 50 years, equivalent lesions have not been clearly understood and there is no clear definition of what an equivalent Monteggia lesion would be [47]. The typological classification of Monteggia fractures- dislocations assesses the features and type of the two associated lesions: ulna fracture and dislocation of the proximal end of the radius. This classification is important for understanding equivalent lesions or the unknown additional variants that are likely to be encountered in practice and treatment. Additional lesions accompanying classic Monteggia lesions increase the complication rate [48]. Therefore, more attention is needed to recognize these types of lesions and treat them appropriately. In medical practice, the following Monteggia lesions can be identified:
1. Typical
Monteggia lesions. In type ll, the radial head is dislocated posteriorly. All
fractures-dislocations described by Monteggia and Bade are classic lesions that
have two typical components: ulna fracture in the proximal segment of the
diaphysis and radial head dislocation.
2. Atypical
Monteggia lesions
a) with
an atypical ulnar component; ulna fracture is located proximally or distally to
the proximal diaphysis segment;
b) with an atypical radial component. In these Monteggia lesions, the atypical radial component involves dislocation
of the proximal end of the radius after the radial neck or head fracture and a typical or atypical component of the ulna fracture;
c) with
both atypical components. Ulna fracture is located cranially or caudally to the
proximal segment of the ulnar diaphysis, and posterior dislocation involves the proximal radial diaphysis.
The studied case has a typical component, namely radial
head dislocation, but two atypical components are also present, more specifically,
the coronoid and metaphysical olecranon fractures.
The studied case has a typical component, namely radial head dislocation, but two atypical components are also present, more specifically, the coronoid and metaphysical olecranon fractures.
TRASH
TRASH lesions were originally described by Waters and Kasser in 2010 [49]. These lesions are generated by high- intensity trauma and are possible to be overlooked due to multiple nonossified elbow centres or the presence of small fragments where non-ossified cartilage is predominant. The studied patient was gradually explored and treated. After reduction of the dislocation, the control radiograph showed a blurred image of an osteochondral flap, which was also augmented by the plaster splint. In this context, an olecranon fracture and an additional lesion that could not be definitely identified were suspected. The radiological image indicates a TRASH lesion and suggests a group of chondral or osteochondral fractures that obscure the normal radiological appearance. Suspected lesions may be fractures of the capitalism, condyles or epicondyles, coronoid and radial head [28]. Special attention should be paid to an x-ray picture that blurs the joint space and obscures its radiological appearance. The osteochondral coronoid flap veils the configuration of the joint space. CT revealed a coronoid fracture and confirmed the olecranon fracture. Thus, it can be considered a TRASH lesion but not a trans olecranon fracture with occult osteochondral coronoid fracture and radial head dislocation. After logical reasoning and in the context of the data provided by the medical literature, not all olecranon fractures accompanied by chondral and osteochondral lesions or dislocations fall into the TRASH trans olecranon fracture- dislocation category. The olecranon fracture is associated with the coronoid fracture, but the presence of radial head dislocation rather suggests another injury. Three distinct pathological entities are associated in a complex lesion, which were analysed as isolated or partially associated lesions.
A new terrible triad of the elbow
The patient has three distinct lesions making up the terrible triad of the elbow, namely: olecranon fracture, coronoid fracture and radial head dislocation. The terrible triad was described by Hotchkiss [50], who defined it as a posterior elbow dislocation associated with a radial head or neck fracture and a coronoid fracture. He called it the “terrible triad injury” because of the poor outcomes and high complication rate [51-53]. These lesions are rare in adults and extremely rare in children. In both cases, two fractures and a dislocation are present. The terrible triad and the three lesions of the studied patient have in common the coronoid process fracture; the other injuries are the radial head or neck fracture in the terrible triad and the olecranon fracture, and dislocations concern the elbow and radial head. Both dislocations are posterior. In both cases, the lesions include the upper extremities of the forearm. The common element, which is the coronoid fracture, bears a striking resemblance. The law of serial cases gave us the opportunity to observe the spontaneous development of a lesion triad of the elbow similar to that affecting the studied patient, which was also associated with the humeral condyle fracture. At the age of 6-7 years, the patient suffered an elbow injury that he neglected, wearing a scarf with the elbow in flexion for several days. Over the course of 8 years, the patient noticed changes in the elbow function, which progressively amplified and, at the age of 14, unbearable intense pain and elbow ankyloses with limitation of extension appeared. He presented for a consultation and, on CT and 3D-CT, we found, together with the imaging physician, the sequelae of a similar triad associated with a condyle fracture. The multiple heterotopic ossifications highlighted by imaging were the consequence of comminute particles, which are commonly encountered in olecranon and coronoid fractures. Complications are redoubtable and identical to those mentioned in the terrible Hotchkiss triad: stiffness, arthritis, multiple reoperations, pain and functional limitations [54,55]. After 2004, application of the protocols proposed by Pugh [56] has made this triad no longer as terrible as before. Retrospective studies of patients with the terrible triad showed that the outcomes of established treatments were consistently poor; for this reason, it was called the terrible triad [57]. The patient did not present an anterior trans olecranon fracture-dislocation. Yamamuro [27] was the first to report a case in 2020, and then Zeng reported another case in 2022, with three identical lesions; these patients were classified with trans olecranon injuries because they had olecranon and coronoid fractures, as in this case report, but the two patients had anterior elbow dislocation instead of posterior radial head dislocation. Ulna fracture and coronoid fracture associated with posterior radial head dislocation make the studied case unique. Dalian et al. [58] present two patients with the terrible triad injury, including a 4½-year-old girl who showed, in addition to the three specific lesions, an olecranon fracture. It could have been classified as a trans olecranon fracture [59] if the patient had an anterior elbow dislocation [58]. The investigated patient’s injury was not a fracture with anterior elbow dislocation but an olecranon fracture without elbow dislocation; it involved the radius and displaced posteriorly, being a partial similarity with the terrible triad where displacement affects the radius and the ulna. Until April 2022, only 12 cases of paediatric trans olecranon fracturedislocation have been reported, of which only two concurrently presented with a coronoid fracture [28], although most dislocations had already been reduced at presentation [24,60]. Therefore, the patient presents a novel terrible triad with two fractures and a dislocation (2F + 1D), which can be reported as CO + RHD (C = coronoid, O = olecranon and RHD = radial head dislocation) that is easier to remember mnemonically by calling it CORHD. Heterotopic ossifications are the stigmata of comminute particles with an intrinsically activated bio-field or through the interference of adjacent magnetic fields [61]. Currently, the term “terrible” is no longer related to the outcomes obtained in the treatment of the triad, which were constantly unfavourable until 2010. But this term can warn the orthopaedic surgeon that these injuries may lead to dreadful, terrible complications.
Conclusion
As in the terrible triad, a dislocation associated with two osteochondral fractures of the articular end of the ulna requires treatment within the limits of the orthopaedic emergency, which aims at the anatomical reduction and firm stabilization of fractures as well as the restoration of ligaments when it is necessary to ensure early mobilization and fully recover elbow mobility.
References
- Massetti D, Marinelli M, Palmisani R, Coppa V, Gigante AP (2021) Pediatric trans-olecranon fracture dislocation of the elbow associated with fracture of the radial head and with medial collateral ligament lesion: a case report and review of the literature. Trauma Case Rep. 32: 100399.
- Vesely D (1967) Isolated Traumatic Dislocation of the Radial Hed in Clinical Orthopaedics and related Research. 50: 31-36.
- Tarallo L, Novi M, Porcellini G, Catani F (2020) Isolate and irreducible radial head dislocation in children: a rare case of capsular interposition. BMC Musculoskelet Disord. 21: 659.
- Burnei G, , Dan D, Georgescu I, Logeanu M, Zavoianu S (2005) Treatment of traumatic dislocation of radial head by ligamentoplasty with extensor carpi radialis longus. SOROT, 11th National Congress of Orthopedics and Traumatology, Palace of Parliament, 6:26-33 .
- Hume A (1957) Anterior Dislocation of the Radial Head in Children Asociated with Undisplaced Fracture of the Ulna. The Journal of Bone & Joint Surgery (British).39: 508-512.
- Boumpoutou R, Guerin B, Boroco A, Mouret G and Choulot JJ (2004) Luxation post-traumatique isolee de la tete radiale chez un enfant. 17: 79-82.
- Ayouba, G, Walla, A. and Bakriga, B (2016) Traumatic Isolated Radial Head Dislocation in Children: A Case Report. Open Journal of 6: 344-349.
- Gupta V, Kundu Z, Sangwan S, Lamba D (2013) Isolated post- traumatic radial head dislocation, a rare and easily missed injury-a case report. Malays Orthop J. 7: 74-78.
- Lincoln TL, Mubarak SJ (1994) “Isolated” traumatic radial-head dislocation. J Pediatr Orthop. 14: 454-457.
- Pesamosca A, Burnei G, Puiu S, Hahui C, Ciobanu C, et al (1994) Treatment of radial head luxation “Meeting of Orthopaedic jubilee of 1-3 June 1994: 41.
- Pesamosca A, Burnei G, Ciobanu C, Cernea I, Sălăjan S, et al (1994) Orthopedic and surgical treatment of fracture Monteggia -Stănciulescu. Meeting of Orthopedic jubilee of 1994: 46-47.
- Burnei G (2010) Proximal radio‐ulnar ligamentoplasty in radial head displacement. EPOS, 29th Annual Meeting, Zagreb, Croatia.
- Bhardwaj A, Sharma G (2018) Isolated traumatic chronic anterior dislocation of radial head. J Clin Diagn Res, 12: 4-5.
- Bhaskar A (2009) Missed Monteggia fracture in children: is annular ligament reconstruction always required? Indian J Orthop, 43: 389
- Li Z, He Y, Zhong G, Huang F (2011) Research progress in repair and reconstruction of isolated traumatic radial head dislocation with annular ligament injury in children. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 25: 1266-1268.
- Stans AA, Morrey BF (2020) Proximal Ulnar Fractures in Children. Chapterul 18.
- Takeuchi H, Ito K, Ogino T, Hasegawa T, Kitamura M, et al (2003) A case of osteocartilaginous mass involving the coronoid process of the ulna: solitary osteochondroma or dysplasia epiphysealis hemimelica? J Shoulder Elbow Surg. 12: 510-513.
- Riga Th (1969) Practical Anatomy Course Vol. l Partea l, Bucharest 1969: 106-107.
- Johnston TB, Willis J (1944) Gray’s Anatomy Descriptive and Applied Vol ll Osteology, Arthrology, Myology. Twenty-seventh edition, by Popa Gr T and Popa Gr F, Bucharest 1944: 464-469.
- Sinelnikov RD (1988) Atlas of Human Anatomy, The Science of Bones, Joints, Ligaments and Muscles, 1: 123-127.
- Waters PM, Skaggs DL, Flynn JM (2019) Rockwood and Wilkins. Fractures in Children. Ninth Edition.
- Ring D, Jupiter JB, Sanders RW, Mast J, Simpson NS (1997) Transolecranon fracture-dislocation of the elbow. J Orthop Trauma. 11: 545-550.
- Wilkerson RD (1993) anterior elbow dislocation associated with olecranon fractures--review of the literature and case report. Iowa Orthop J. 13: 223-225.
- Arain AR, Haddad S, Anderson M, Murtaza H, Rosenbaum A (2019) Isolated pediatric transolecranon fracture- dislocation of the elbow managed nonoperatively: A case report and review of literature. Clin Case Rep. 7: 1435-1438.
- Guitton T.G., Albers R.G., Ring D (2009) Anterior olecranon fracturedislocations of the elbow in children. A report of four cases. J Bone Joint Surg Am. 91: 1487-1490.
- Butler MA, Martus JE, Schoenecker JG (2012) Pediatric variants of the transolecranon fracture dislocation: recognition and tension band fixation: report of 3 cases. J Hand Surg. 37: 999-1002.
- Yamaura K, Inui A, Mifune Y, Nishimoto H, Kataoka T, et al (2021) Anterior transolecranon fracture dislocation with an associated avulsion fracture of coronoid process of ulna in a child: a case report. JSES Int. 5: 9-12.
- Zheng JL, Shah AS, Nguyen J, Baldwin KD (2) TRASH” Transolecranon Fracture-Dislocation with Occult Osteochondral Coronoid Fracture: A Case Report. 2022 JBJS Case Connector. 12.
- Valisena S, Hamitaga F, Gonzalez JG, Voumard NM, Ciritsis BD, et al (2019) Osteochondral flap fracture of the coronoid in pediatric elbow dislocation: a case report and literature review. Eur J Orthop Surg 29: 213-220.
- Chambers H, Garza JF, O’Brien E, Price CT, Stanley E, et al (1996) Fractures of the radius and ulna. Rockwood & Green’s Fractures in children (4th edition),Lipincott-Raven.
- Regan W, Morrey BF (1992) Classification and treatment of coronoid procesa fractures. Orthopedics, 15: 845-848.
- Wang D, Li J, Xu G, Zhang W, Li L, et al (2022) Classification of coronoid process fractures: A pending question. Front. Surg. 9: 890744.
- Regan W and Morrey B (1989) Fractures of the coronoid process of the ulna. J. Bone Joint Surg., 71-A: 1348-1354.
- Terada N, Yamada H, Seki T, Urabe T, Takayama S (2000) The importance of reducing small fractures of the coronoid process in the treatment of unstable elbow dislocation. J. Shoulder Elbow Surg., 9: 344-346.
- Gadgil A, R. Roach R, Neal N, Maffulli N (2002) Acta Orthopædica Belgica, 68: 396-398.
- Tanzman M., Kaufman B (1988) Fracture of the coronoid process of the ulna requiring reduction in extension. J. Hand Surg., 13-A: 741
- Bado JL (1967) The Monteggia lesion. Clin Orthop Relat Res. 50:71
- Stanley EA, Garza JFDL (2004) Fratura-luxaxca o de Monteggia. In: Beaty JH, Kasser JR, editors. Rockwood e Wilkins fraturas em 5th ed. Barueri: Editora Manole; 2004: 529-562.
- Burnei G, Raducan ID Lală CG, Klinaku I, Marti TD, et al (2020) Monteggia Fracture-Dislocation: Past and Present. Clinics of Sugery. 3: 1-8.
- Strauss EJ, Tejwani NC, Preston CF, Egol KA (2006) The posterior Monteggia lesion with associated ulnohumeral instabilitaty. J Bone Joint Surg Br. 88: 84-89.
- Ghinea CA, Gaviriliu S, Gergescu I, Vlad C, Japie E, et al (2013) Burnei’s technique in the treatment of radial head displacement; innovative surgery. Study on two cases. J Med Life. 6: 26-33.
- Dughila C, Dragoescu M, Burnei G (2015) Burnei’s Ligamentoplasty with Biceps Brachi Tendon in the Treatment of the Radial Head Dislocation-a Terapeutic Option of the ECRL Ligamentoplasty. . The Vlll-Th ARTOP Congress, 2015: 21-22.
- King RE (1984) Fractures of the shafts of the radius and ulna. In: Rockwood JCA, Wilkins KE, King RE, editors. Fractures in children. Philadelphia: Lippincott; 1984.
- Canale ST (2007) Fractures and dislocations in children. In: Canale ST, Beaty JH, editors. Campbell’s operative orthopaedics. 11th ed. Maryland Heights: Mosby; 2007: 1531-725.
- Kamudin N, Firdouse M, Han CS, M Yusof A (2015) Variants of Monteggia type injury: case reports. Malays Orthop J. 9: 23-27.
- Ribeiro T, Pinho FZ, Bellemzier L, Guerra V, Nascimento D (2013) An Atypical Tipe-ll Monteggia Fracture EquivalentLesion: A Case Report. JBJS Case Connector. 3: e 43.
- Karashi AR, Basheer SM, Alsobyani FM, et al (2021) (November 13, 2021) A Novel Variant of Type II Monteggia Equivalent FractureDislocation in Children: A Case Report. Cureus 13: e19541.
- Singh AP, Dhammi IK, Jain AK, Raman R, Modi P (2011) Monteggia fracture dislocation eqivalents analysis of eighteen cases treated by open reduction and internal fixation. Chin J Traumatol. 14:221-226.
- Waters PM, Beaty J, Kasser J (2010) Elbow “TRASH” (The Radiographic Appearance Seemed Harmless) lesions. J Pediatr 30: S77-81.
- Hotchkiss RN (1996) Fractures and dislocations of the elbow.in: Rockwood Jr, C.A. Green D.P. Bucholz R.W. Heckman J.D. 4th ed. Rockwood and Green’s Fractures in Adults. Vol 1. Lippincott-Raven, Philadelphia1996: 929-1024.
- Broberg MA, Morrey BF (1987) Results of treatment of fracturedislocations of the elbow.Clin Orthop Relat Res. 1987: 109-119.
- Ring D, Jupiter JB, Zilberfarb J (2002) Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am 84-a: 547-551.
- Terada N, Yamada H, Seki T, Urabe T, Takayama S (2000) The importance of reducing small fractures of the coronoid process in the treatment of unstable elbow dislocation. J Shoulder Elbow Surg 9: 344-334.
- Pugh DM, Wild LM, Schemitsch EH, King GJW, McKee MD (2004) Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am. 86: 1122-1130.
- Egol KA, Immerman I, Paksima N, Tejwani N, Koval KJ (2007) Fracture- dislocation of the elbow functional outcome following treatment with a standardized protocol. Bull NYU Hosp Jt Dis 65: 263-270.
- Guo W, Lu D, Wang J, Luo P, Liu M, et al (2020) Terrible Triad Injury or Complicated Triad Injury of Elbow: A Systematic Review. Journal of Surgery and Research 3: 216-229.
- Mathew PK, Athwal GS, King GJ (2009) Terrible triad injury of the elbow: current concepts. J Am Acad Orthop Surg. 17: 137-151.
- Dailiana ZH, Papatheodorou LK, Michalitsis SG, Varitimidis SE (2013) Pediatric terrible triad elbow fracture dislocations: report of 2 cases. J Hand Surg Am. 38: 1774-1778.
- Toros T, Ozaksar K (2014) Controversy in the diagnosis of pediatric terrible triad elbow fracture dislocation. J Hand Surg Am. 39: 2121
- Yang Z, Feng C, Bian Z, Lu M, Zhou D (2021) Trans- olecranon fracture–dislocation of the elbow in children. Int Orthop. 45: 2025
- Burnei G, Hodorogea D, Georgescu I, Gavriliu S, Draghici I, et al (2012) The electromagnetic bio-field: clinical experiments and interferences. J Med Life. 5: 139-144.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.