Compression Neuropathy of Common Peroneal Nerve by Fabella: A Case Report of Surgery with Intraoperative Nerve Action Potential Recording
by Florian Dashi1*, Arba Cecia2, Ada Muco3, Arben Rroji4, Ridvan Alimehmeti5, Mishel Qirinxhi5
1Functional Explorations and Intraoperative Monitoring, Department of Neurosciences, University Hospital Center “Mother Teresa”, Tirana, Albania
2Stritch School of Medicine, Loyola University Chicago. Maywood, Illinois, USA
3Department of Neurology, University Hospital Center “Mother Teresa”, Tirana, Albania
4Department of Interventional Neuroradiology, University Hospital Center “Mother Teresa”, Tirana, Albania
5Department of Neurosurgery, University Hospital Center “Mother Teresa”, Tirana, Albania
*Corresponding author: Florian Dashi, Functional Explorations and Intraoperative Monitoring, Department of Neurosciences, University Hospital Center “Mother Teresa”, Rruga Kongresi i Manastirit, Tirana, Albania
Received Date: 10 December 2024
Accepted Date: 16 December 2024
Published Date: 18 December 2024
Citation: Dashi F, Cecia A, Muco A, Rroji A, Alimehmeti R, et al. (2024). Compression Neuropathy of Common Peroneal Nerve by Fabella: A Case Report of Surgery with Intraoperative Nerve Action Potential Recording. Ann Case Report. 9: 2121. https://doi.org/10.29011/2574-7754.102121
Abstract
Fabella is a small sesamoid bone located within the tendon of the lateral gastrocnemius muscle, often articulating with the lateral condyle of the femur which has become increasingly visible in people’s knees. The peroneal nerve’s proximity to the lateral gastrocnemius tendon makes it susceptible to compression by the fabella. Patients may exhibit symptoms such as sudden footdrop, pain and numbness along the dorsum of the foot. Only a few case reports have investigated the causal link between fabella and peroneal nerve palsy. We present a case where we utilized intraoperative nerve action potential recordings to elucidate this causal relationship during a practical surgical decision-making process.
Keywords: Peroneal nerve entrapment, Footdrop, Fabella, Nerve action potential, Intraoperative monitoring.
Introduction
Fabella is a small sesamoid bone located within the tendon of the lateral gastrocnemius muscle, often articulating with the lateral condyle of the femur [1]. Although it is primarily found in the far eastern population, its prevalence among all populations is 10% - 30% [2,3]. It was once lost in humans over the course of evolution,
but is now experiencing a resurgence. Millions of years ago, the bone disappeared from our ancestry, but in the past century, it has become increasingly visible in people’s knees. Back In 1918, only 11% of the global population had a fabella, but the number now has risen to 39% [4]. Similar to the patella, it functions as a stabilizer for the posterior knee ligaments and forms due to the mechanical stress exerted by the calf muscles, leading to ossification of the tendon. It is most often bilateral [2,5]. The peroneal nerve’s proximity to the lateral gastrocnemius tendon makes it susceptible to compression by the fabella or inflammation of surrounding tissue. This compression can result in a variety of abnormalities, ranging from focal demyelination to potentially severe secondary axonal loss if left untreated. Patients may exhibit symptoms such as sudden foot drop and numbness along the dorsum of the foot. Only a few case reports have investigated the causal link between fabella and peroneal nerve palsy [2,5-8]. We present a case where we utilized intraoperative near-nerve recordings to elucidate this causal relationship during a practical surgical decision-making process.
Case Presentation
The patient, a 23-year-old, 172 cm. tall, man, reported a sudden foot drop on the left side that persisted for one month. Upon neurological examination, there was a notable loss of dorsiflexion and eversion of the left foot, with intact inversion and plantar flexion (Figure 1). Numbness was reported on the top of the foot and the outer part of the lower leg. In other areas, strength and sensibility remained intact, and osteotendinous reflexes were normal. Nerve conduction studies (NCS) of the left peroneal nerve recorded over the extensor digitorum brevis muscle (EDB) showed a normal distal latency and compound motor action potential (CMAP) after stimulation at both the ankle and under the fibular head and at 8 cm above the fibular head. However, at a more proximal location than expected - 17.5 cm proximal to the fibular head - between the biceps femoris muscle and the lateral gastrocnemius tendon a significant reduction of CMAP and temporal dispersion was observed, indicating an almost complete conduction block (Figure 2). The left superficial peroneal nerve’s sensory amplitude was normal. Concentric needle electromyography (EMG) showed a lack of voluntary contractions in the left tibialis anterior muscle (TA), left extensor hallucis longus muscle (EHL), and left extensor digitorum brevis muscle (EDB). These muscles exhibited no spontaneous denervation activity. The EMG was normal in the short head of the left biceps femoris muscle (BF), left tibialis posterior muscle (TP), and left adductor hallucis muscle (AH). This electrophysiological pattern suggested a demyelination of the left common peroneal nerve in the popliteal fossa rather than in the fibular neck. Palpation at the popliteal fossa, at the level of the lateral gastrocnemius tendon, revealed the presence of a small, firm, round, fixed, and non-painful structure suggestive of a fabella complex. A positive Tinel sign was elicited at this level, while no Tinel sign was present at the level of the fibular head or slightly above it. Magnetic resonance imaging (MRI) of the left knee confirmed the presence of fabella (Figure 3). After a month of no spontaneous improvement in the patient’s condition, we recommended surgery. The neurosurgeon, before determining the surgical approach, sought to confirm whether the nerve’s functional impairment occurred at the segment of the nerve at the fabella rather than the more typical location at the fibular neck. For this purpose, we suggested intraoperative recording of nerve action potentials (NAP) to identify the site of demyelination that would undergo nerve release. Exposing the fabella bone and a long segment of the peroneal nerve would necessitate longer incisions as opposed to the standard procedure of peroneal nerve release at the fibular head, which requires shorter incisions [9]. The surgeon performed an S-shaped incision at the popliteal fossa, exposing a long segment of the common peroneal nerve to assess the extent of adherences and facilitate intraoperative recordings. A fabella bone was found beneath a segment of the nerve that appeared upwardly deviated. This segment of the nerve appeared pale and flattened at the level of fabella and was encircled by inflammatory adhesions (Figure 4). To assess the conduction block, nerve action potentials (NAP) were obtained by stimulating the nerve with a tripolar hook electrode and recording it in a different section of the nerve with a bipolar hook electrode (Figure 5). We used square wave stimulations with an intensity of 0.5-1 mA, a duration of 0.05 ms, and a frequency of 1-2 Hz. The signal was then recorded with NIM E4 Axon Eclipse IOM equipment with a low-frequency (LF) at 10 Hz and high-frequency (HF) of 2.5 KHz, utilizing a time base of 0.5 ms/div and 200 uV/div and without applying a notch filter [10]. NAP is a mixed nerve potential that reflects the conduction velocity of large-myelinated nerve fibers. The recording technique can be performed both orthodromically and antidromically, yielding the same results in near-nerve recordings. Given the absence of axonal loss indicated in preoperative assessment, we started the NAP recordings by stimulating the nerve distal to the fabella and recording the response distal to the stimulation site (antidromically). Subsequently, the stimulation electrode was moved proximally in 1 cm increments in the proximal direction until positioned 2 cm above the fabella. Notably, NAP was not recorded at or above the level of fabella, indicating a complete conduction block at this specific site (Figure 6). Following this observation, adherentiolysis of five centimeters above and below the fabellar segment of the nerve was performed followed by epineurotomy of the small segment above fabella. Subsequently, revascularization of this segment was observed. The released nerve shifted tension-free to a more medial position relative to the fabella that was left in place (Figure 7). The surgery was uneventful, and one month after the surgery, the patient fully regained the normal strength of the left foot (Figure 8).

Figure 1: Preoperative picture showing left foot drop following common peroneal nerve injury.
Motor NCS of left common peroneal nerve.
|
Stim. site |
Latency ms |
Amplitude mV |
Duration ms |
Distance mm |
Velocity m/s |
|
ankle |
3.7 |
5.1 |
6.5 |
50 |
|
|
Below cap. fibulae |
9.3 |
5.1 |
7.29 |
311 |
55.3 |
|
Above cap. fibulae |
13.4 |
0.3 |
10.8 |
175 |
42.7 |
Sensory NCS of left superficial peroneal nerve.
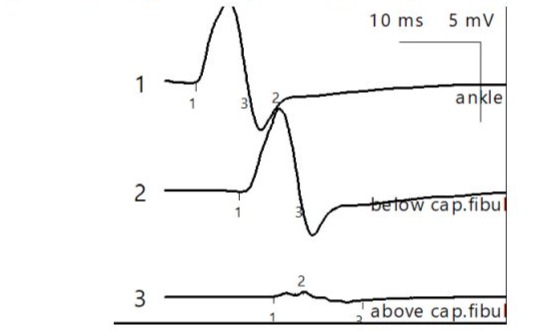
Figure 2: NCS demonstrate a conduction block and a temporal dispersion of the CMAP after stimulating at 175 cm above the fibular head.
|
Site |
Latency ms |
Amplitude µV |
Distance mm |
Velocity m/s |
|
Middle third of leg |
1.7 |
14.0 |
100 |
58.8 |
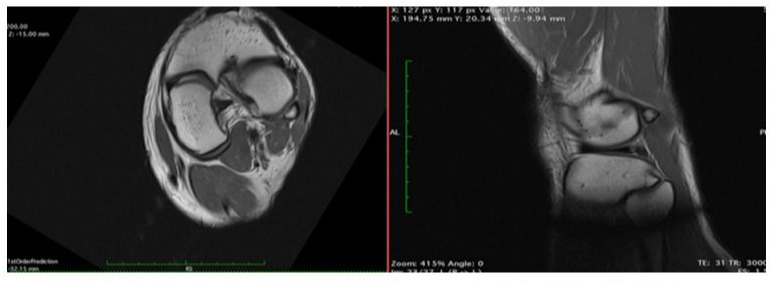
Figure 3: Left: axial and sagittal MRI of the left knee showing the fabella bone (blue arrow).

Figure 4: The peroneal nerve appears pale, showing fibrous adherences and deviating upward due to the underlying fabella.
takes a more medial position.

Figure 5: Stimulating and recording technique for nerve action potentials (NAPs).
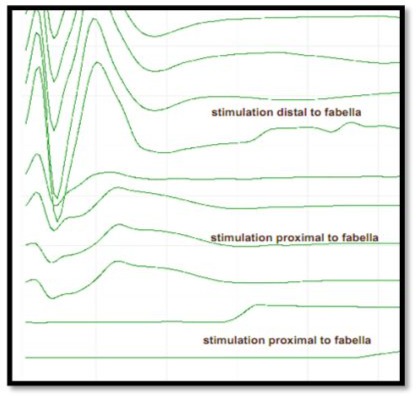
Figure 6: Stimulation of the peroneal nerve segment distal to the fabella and distal to the stimulation electrode results in a clear NAP due to the absence of Wallerian degeneration distal to the site of compression. Progressively moving the stimulation electrode proximal to fabella confirms the site of conduction block at the fabellar segment of the peroneal nerve.

Figure 7: The peroneal nerve is released by the adhesions and takes a more medial position.

Figure 8: Follow-up at 1 month showing full recovery of left foot dorsiflexion.
Discussion
Common peroneal nerve entrapment is a frequent occurrence in the practice of diagnostic neurophysiology and neurosurgical departments with special expertise in peripheral nerve surgery. It is widely recognized that entrapment typically occurs at the point where the nerve wraps around the fibular neck. Generally, NCS show that stimulation at a location 8-10 cm above the fibular head can reveal conduction block, temporal dispersion, or a significant decrease in conduction velocity in this nerve segment. Our patient had a typical clinical presentation of this condition, but interestingly, we had to stimulate 17.5 cm above the fibular neck, deep between the biceps femoris muscle and lateral gastrocnemius tendon to detect the conduction block. Palpation of the gastrocnemius tendon and MRI of the knee revealed the presence of the fabella bone and during surgery it was seen impinging on the peroneal nerve’s path. Intraoperative NAP suggested that the conduction block was limited to this impinged segment of the nerve. Performing adherentiolysis without excising the fabella bone proved to be sufficient in improving the patient’s symptoms.
Conclusion
If the standard stimulation site at the popliteal crease does not show a primary demyelinating abnormality in the typical weakness pattern suggestive of common peroneal nerve entrapment, diagnostic NCS should, whenever possible, include a further proximal stimulation between biceps femoris muscle and gastrocnemius tendon, though higher stimulation intensities may be required. It is advisable to suspect higher proximal causes of compression, and, given the increasing incidence of fabella over the past century, always investigate its presence through palpation or MR imaging. Previous case reports have suggested a potential link between fabella and peroneal nerve compression neuropathy. Our study, utilizing intraoperative nerve action potential recordings, is the first to provide functional evidence supporting this causal link. Incorporating nerve action potential assessment during surgery may prove beneficial in surgical decision-making.
Declarations
Contributors: All authors contributed to planning, literature review and conduct of the review article. All authors have reviewed and agreed on the final manuscript.
Competing interests: None
Patient consent for publication: Informed consent was obtained from the patient, consent form available upon request
Ethics approval and consent to participate: Not applicable
Availability of data and materials: Not applicable
Funding: No Funding.
References
- Dalip D, Iwanaga J, Oskouian RJ, Tubbs RS. (2012). “A Comprehensive Review of the Fabella Bone,” Cureus. 10: e2736.
- Zeng SX, Dong XL, Dang RS, Wu GS, Wang JF, et al. (2012). “Anatomic study of fabella and its surrounding structures in a Chinese population,” Surg Radiol Anat. 34: 65-71.
- Duncan W, Dahm DL. (2003). “Clinical anatomy of the fabella,” Clinical Anatomy. 16: 448-449.
- Berthaume MA, Di Federico E, Bull AMJ. (2019). “Fabella prevalence rate increases over 150 years, and rates of other sesamoid bones remain constant: a systematic review,” J. Anat. P: 12994.
- Cesmebasi A, Spinner RJ, Smith J, Bannar SM, Finnoff JT. (2016). “Role of Sonography in the Diagnosis and Treatment of Common Peroneal Neuropathy Secondary to Fabellae,” J Ultrasound Med. 35: 441-447.
- Patel A, Singh R, Johnson B, Smith A. (2013). “Compression neuropathy of the common peroneal nerve by the fabella,” BMJ Case Reports. 2013: bcr2013202154.
- Décard BF, Nagy S, Garcia M, Fuhr P. (2017). “An unusual case of bilateral peroneal palsies due to fabellae,” Neurology. 88: 918.
- Hauser NH, Hoechel S, Toranelli M, Klaws J, Müller-Gerbl M. (2015). “Functional and Structural Details about the Fabella: What the Important Stabilizer Looks Like in the Central European Population,” BioMed Res Int. 2015: 343728.
- Wilson TJ, Spinner RJ. (2018). Peroneal Neuropathy-Fibular Tunnel Syndrome. Oxford University Press. P: 1.
- Robert EG, Happel LT, Kline DG. (2009). “Intraoperative Nerve Action Potential Recordings: Technical Considerations, Problems, and Pitfalls. Neurosurgery. 65: A97-A104.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.