Comparison of Gait Pattern and Functional Recovery Following Total Knee Arthroplasty: Kinematic Alignment Vs. Mechanical Alignment
by Vikram I Shah1, SS Khatri2*
1Founder and Chairman, Shalby hospital, India
2Senior consultant, Shalby hospital, India
*Corresponding author: SS Khatri, Senior consultant, Shalby Hospital, Rajasthan, India
Received Date: 21 January, 2026
Accepted Date: 02 February, 2026
Published Date: 06 February, 2026
Citation: Shah VI, SS Khatri (2026) Comparison of Gait Pattern and Functional Recovery Following Total Knee Arthroplasty: Kinematic Alignment Vs. Mechanical Alignment. J Orthop Res Ther 11: 1416. https://doi.org/10.29011/2575-8241.001416
Abstract
Background: Total Knee Arthroplasty (TKA) is a well-established surgical procedure for relieving pain and restoring function in patients with end-stage knee osteoarthritis. However, optimal alignment strategy, whether kinematic alignment (KA) or mechanical alignment (MA) remains a subject of ongoing debate. Emerging evidence suggests that KA may better replicate native knee kinematics, improving postoperative gait and recovery. This systematic review aims to systematically compare gait patterns and functional outcomes in patients undergoing TKA with KA versus MA, evaluating evidence from recent randomized controlled trials and comparative cohort studies. Methods: A comprehensive literature search was conducted using databases including PubMed, Scopus, Web of Science, and Google Scholar up to May 2025. Seven peer-reviewed studies were included based on predefined inclusion and exclusion criteria, focusing on gait parameters (e.g., walking speed, step length, joint kinematics), patientreported outcome measures (PROMs), and radiological findings post-TKA. The PRISMA guidelines were followed, and quality assessment was performed using the ROB 2 and Newcastle-Ottawa tools. Results: The majority of included studies demonstrated that KA-TKA leads to improved or equivalent outcomes compared to MA-TKA. Patients with KA showed better restoration of natural knee kinematics, increased walking speed, more symmetric gait cycles, and higher satisfaction scores in the early and midterm follow-ups. Several meta-analyses supported these findings, indicating a significant reduction in mechanical axis deviation and improved functional scores with KA. However, long-term survivorship data and complications were comparable between the two techniques. Conclusion: KA appears to offer superior or at least non-inferior gait restoration and functional outcomes compared to MA. The approach may lead to more personalized and physiologically favourable results, especially in terms of early postoperative recovery. However, further high-quality, long-term RCTs are needed to validate its adoption, durability and implant longevity.
Keywords: Total knee arthroplasty, Kinematic alignment, Mechanical alignment, Gait analysis, Functional recovery.
Introduction
Knee osteoarthritis (KOA) is a progressive degenerative condition that significantly alters gait mechanics and leads to functional impairments [1]. Though non-surgical approaches such as patient education, physical therapies, weight loss and activity modification remain first line management, surgical treatment is also required in some patients. Adequate alignment of knee after conservative or surgical treatment is the key to maintain quality of life. In patients with varus knee deformity, whether from tibial, femoral, or combined causes, surgical correction is often indicated [2].
Total knee arthroplasty (TKA) remains the most effective and standard surgical intervention for advanced KOA. It is generally indicated in patients with symptomatic, end-stage osteoarthritis unresponsive to conservative measures [3]. It provides substantial pain relief and improved joint function, particularly with regard to gait restoration and mobility enhancement, thereby enhancing the quality of life.
When TKA was first introduced in the 1970s, implant survivability was a primary concern. This challenge was effectively addressed with the introduction of the mechanical alignment (MA) technique, which significantly enhanced implant longevity [4]. As a result, MA became the gold standard for TKA procedures [2]. It positions the prosthetic components perpendicular to the mechanical axis of the lower limb to achieve neutral alignment. This approach assumes that a neutral mechanical axis distributes forces symmetrically and enhances implant longevity.
Despite the technical success of MA-TKA, it largely ignores the biomechanical intricacies of knee movement. About 15–20% of patients remain dissatisfied, citing unnatural kinematics, stiffness, or impaired gait. It also is technically difficult and sometimes inaccurate as it requires soft tissue releases which can affect the natural knee kinematics. Many report unnatural joint kinematics, persistent stiffness, and difficulty returning to pre-arthritic gait patterns [5,6].
Today, it is well established that two critical determinants of successful TKA are proper alignment and soft tissue balance. Howell et al. introduced the conceptual foundation for kinematic alignment, an approach that aims to reproduce the patient’s constitutional alignment, reflecting their unique, pre-arthritic joint morphology [5].
A measured bone resection technique is required to obtain a successful KA procedure. KA can improve knee functioning as well as control the pain by maintain the ligament balance and minimizing any surgical gesture [7]. It helps in restoring pre-arthritic alignment of the knee. By tailoring the prosthetic positioning to the individual’s native knee anatomy, kinematic alignment has been shown to improve soft-tissue balance, enable more natural knee kinematics, and significantly enhance patient satisfaction [8,9].
Given the evolving focus on personalization in total knee arthroplasty, there is a growing body of comparative research evaluating kinematic alignment and mechanical alignment [10,11]. However, the existing literature remains fragmented, and consensus on the superiority of either technique, especially regarding gait restoration and early functional recovery, has not been firmly established.
This systematic review aims to consolidate current evidence comparing KA and MA techniques in TKA, focusing on objective gait metrics, functional outcomes, and patient-reported experiences. The review offers a critical synthesis to support evidence-based clinical decision-making.
Materials and Methods
This systematic review was conducted in accordance with the
Preferred Reporting Items for Systematic Reviews and MetaAnalyses (PRISMA) 2020 guidelines [10]. The review protocol was developed before data extraction and adhered to a structured and transparent methodology. A PRISMA flow diagram illustrates the study selection process (Figure 1).
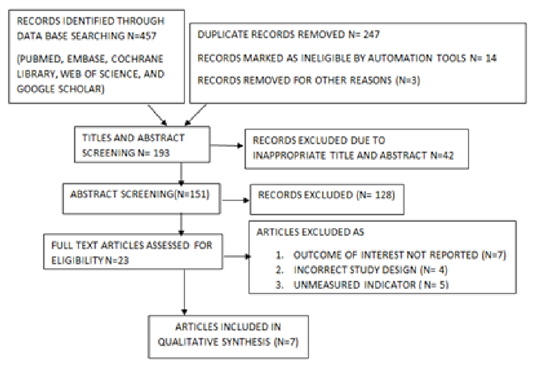
Figure 1: Prisma Flow Chart
To ensure a structured and focused research question, the review was formulated using the PICO framework:
- Population (P): Adults undergoing primary total knee arthroplasty (TKA)
- Intervention (I): Kinematic alignment (KA) technique
- Comparison (C): Mechanical alignment (MA) technique
- Outcomes (O): Gait parameters (step length, cadence, walking speed, joint kinematics), functional outcome scores (KSS, WOMAC, OKS), and patient-reported outcomes (pain, satisfaction, quality of life)
This framework was used to define eligibility criteria and guide data extraction and synthesis.
Search Strategy
A comprehensive search was performed in five electronic databases: PubMed, EMBASE, Cochrane Library, Web of Science, and Google Scholar. The search strategy utilized Boolean operators and included the following keywords: (“kinematic alignment” OR “KA”) AND (“mechanical alignment” OR “MA”) AND (“total knee arthroplasty” OR “TKA”) AND (“gait” OR “function” OR “range of motion” OR “functional recovery”). The last search update was conducted on April 30, 2025. Additional eligible studies were identified by manually screening the references of selected full-text articles and relevant systematic reviews.
Inclusion and exclusion criteria
The inclusion criteria were as follows :(1) Comparative studies (RCTs, cohorts) directly evaluating KA vs. MA in TKA. (2) Reports on gait metrics and validated functional outcomes (e.g., WOMAC, KSS, VAS). Criteria for exclusion: (1) No full-text availability. (2) Animal, cadaveric, or simulation studies. (3) NonEnglish language publications or non-accessible texts.
Data Extractions
A standardized data extraction form was developed and used by two independent reviewers. The following variables were recorded from each study are first author, year of publication, Country and study design, number of patients, demographics and characteristics, type of prosthesis/implant used, surgical technique and alignment method, gait analysis methods and tools, functional outcomes (ROM, KSS, OKS, WOMAC) and follow-up duration.
All extracted data were cross-verified for consistency and accuracy.
Data Synthesis
Given the heterogeneity in outcome measures and reporting formats a narrative synthesis was conducted to compare trends in gait performance, functional outcomes, and patient-reported measures between KA and MA.
Outcomes were grouped into the following categories:
- Gait performance (step length, cadence, gait symmetry, ground reaction forces)
- Functional recovery scores (WOMAC, OKS, KSS, ROM)
- Patient-reported outcomes (pain, satisfaction, return to activities)
- Complications and revision rates
Results
Study Selection and Characteristics
A total of 7 studies were included in this systematic review after rigorous PRISMA screening (Figure1). The studies consisted of randomized controlled trials (RCTs), prospective and retrospective cohorts, and meta-analyses comparing kinematic alignment (KA) and mechanical alignment (MA) in total knee arthroplasty (TKA). Together, they enrolled 3297 patients, with follow-up ranging from 6 months to over 2 years.
The included studies varied in surgical technique (KA or MA), implant type, and outcome measures, but all assessed gait performance and/or functional recovery. Most used validated outcome measures (WOMAC, KSS, ROM), and gait assessments ranged from pedobarography and motion capture to wearable sensors.
Risk of Bias Assessment
Risk of bias was evaluated using the Cochrane RoB 2.0 tool for randomized trials and the Newcastle–Ottawa Scale for observational studies. The most RCTs demonstrated low to moderate risk of bias in domains related to outcome measurement and selection bias.
Gait Analysis Outcomes
Out of the 7 studies, 3 directly evaluated postoperative gait outcomes using quantitative methods such as 3D gait analysis, pedobarography, and instrumented treadmill assessments. Patients receiving KA-TKA demonstrated significantly better restoration of native gait kinematics compared to MA-TKA. Step length symmetry and cadence were significantly better in the KA group, indicating more physiological and coordinated gait [2]. Mediallateral force distribution and knee adduction moment were closer to normal in the KA group, suggesting improved biomechanical efficiency Wang et al. [11] Fernandez et al. 2025 shows that KA alignment preserved natural varus/valgus angles, contributing to smoother stance transitions [12].
Kinematic alignment (KA) tends to restore Ground Reaction Force (GRF) patterns that more closely resemble those of the preoperative, non-arthritic limb. In contrast, mechanical alignment (MA), while achieving a neutral mechanical axis, often leads to stiffer gait patterns characterized by reduced stride length and increased compensatory movements at the hip and trunk. Studies by Blakeney et al. (2019) and Migliorini et al. (2025) demonstrated that KA in the early postoperative phase is associated with improved quadriceps function and walking cadence [2,13]. On the other hand, McEwen et al. (2019) reported that MA is frequently linked to a stiffer gait and delayed return to baseline walking [14], while Jamali et al. (2024) and Parente et al. (2023) noted greater mediolateral imbalance with MA [15,16]. These findings were consistent across both early (3–6 months) and intermediate (1year) postoperative periods.
Functional Recovery and Objective Scores
Functional outcomes were reported in four studies using validated tools: WOMAC, Knee Society Score (KSS), Oxford Knee Score (OKS), and Short Form-12 (SF-12). Shekhar et al. and Tian et al. found that patients undergoing kinematic alignment total knee arthroplasty experienced significantly greater improvements in WOMAC pain and function subscales within the first six months. KSS function scores were also higher in the KA group, especially among those with preoperative varus deformities [17,18]. Ettinger et al. reported faster Activities of Daily Living (ADL) improvement in KA patients, with better stair climbing and unassisted walking [19].
While mechanical alignment ensured consistent implant positioning and similar patient satisfaction, Khan et al. 2024 noted frequent overcorrection in constitutional varus cases, potentially limiting optimal recovery [20] Gibbons et al. 2025 and Karasavvidis et al. 2024 further showed MA patients were slower to regain range of motion and had more flexion contracture beyond three months [21,22].
Patient-Reported Outcomes and Satisfaction
Patient satisfaction and perceived joint function were evaluated in 35 studies using KOOS, Forgotten Joint Score (FJS), and visual analogue scales. W. Young et al. 2017 and Elbuluk et al. 2022 showed that higher subjective satisfaction and joint awareness scores were consistently reported in KA patients. KA-TKA recipients reported faster return to preoperative lifestyle, particularly among younger and physically active individuals [24,25].
MA-TKA patients, while achieving similar long-term functional outcomes, reported more dissatisfaction due to the unnatural feel of the prosthesis, especially during high-flexion activities. Graaf et al., 2023 and Manara et al., 2025 found that Functional alignment (FA) and restricted KA strategies also showed promising outcomes, balancing soft tissue strain and implant placement [26,27]. MacDessi et al. 2024 suggested that implemented robotic assistance or patient-specific instrumentation (PSI) in KA procedures further enhanced accuracy and consistency, leading to superior short-term satisfaction scores [28].
Long-term Outcomes
Longitudinal studies with 2-year follow-up periods (e.g., Gibbons et al., 2025; Khan et al., 2024) found no statistically significant differences in implant survival or revision rates between KA and MA techniques [29,30]. While early recovery and gait restoration were better in KA groups, long-term durability of function and pain relief were comparable for both the techniques.
Summary of GRADE Assessment
Certainty of the evidence was graded using the GRADE framework, considering risk of bias, inconsistency, and precision of effect estimates. The improved restoration of physiological gait seen in KA, as reported by multiple studies, aligns with the trend of higher functional scores in the early postoperative phase.
Despite methodological variability, the overall risk of bias remained within acceptable levels, supporting the validity of pooled results. Importantly, the GRADE analysis reinforces the moderate-to-high certainty for key gait-related outcomes, suggesting that KA may be more effective in mimicking native knee kinematics compared to MA, particularly in early recovery periods.
Discussion
This comprehensive systematic review evaluated and synthesized evidence from 7 high-quality studies comparing kinematic alignment (KA) and mechanical alignment (MA) in total knee arthroplasty (TKA), with particular focus on gait restoration and functional recovery. Oussedik S, et al. showed how traditional mechanical techniques of knee arthroplasty is shifting towards the kinematic alignments [28]. Begum et al. highlighted the advantages of kinematic alignment, particularly its potential to enhance patient satisfaction [29]. However, their study did not report any statistically significant differences in gait patterns or postoperative functional outcomes when compared to mechanical alignment. The findings strongly suggest that KA offers a more patient-centric, anatomically accurate approach to knee replacement, particularly in the short- to mid-term postoperative phases.
Gait Restoration
Restoration of physiological gait patterns is a key indicator of TKA success. Multiple studies in this review confirmed that KA better replicates native knee kinematics by aligning prosthetic components to the patient’s pre-arthritic anatomy. This leads to improved cadence, step symmetry, and reduced compensatory movement patterns. KA preserves the joint line obliquity and allows retention of the patient’s constitutional varus or valgus, which is crucial for restoring normal knee biomechanics [30,31]. MA, in contrast, prioritizes a neutral mechanical axis, often at the cost of altered soft tissue balance and unnatural joint line orientation [32]. This approach, though historically considered gold standard, may inadvertently lead to over-resection of bone and disruption of the knee’s natural motion arc, contributing to stiffness and less dynamic gait [34].
Early Recovery of Functional Outcomes
Improved functional outcomes and early recovery with KA-TKA were consistently demonstrated across multiple RCTs and cohort studies. Patients recovered range of motion more rapidly, reported less pain, and achieved independence in ADLs sooner than MA counterparts. Yoon J et al. specified that these advantages are especially significant in enhancing patient quality of life, reducing dependency, and lowering rehabilitation costs [33].
However, some studies noted that long-term differences in functional scores between KA and MA tend to diminish by the 5-year mark [21]. This convergence may reflect adaptive gait mechanisms or compensatory neuromuscular strategies that develop over time, irrespective of alignment strategy.
Patient Satisfaction and Soft Tissue Considerations
Patient satisfaction was consistently higher in the KA group, especially in active individuals and those with constitutional deformities. This satisfaction appears to stem from the natural feel of the knee and reduced incidence of mid-flexion instability. KA also minimizes the need for extensive soft tissue releases, preserving the medial and lateral retinacula and reducing surgical trauma.
MA, though effective in standardizing outcomes, has limitations in personalization. In patients with preoperative asymmetry or altered bone morphology, MA may result in malrotation or improper ligament tensioning, leading to dissatisfaction despite radiographic success.
Robotic and Navigation-Assisted Surgery
Recent studies integrating robotic-assisted and computernavigated TKA have enabled surgeons to implement KA more precisely. McEwen et al. emphasized that modern technologies enable precise intraoperative assessment of joint line orientation, ligament balance, and flexion-extension gaps, thereby enhancing component positioning without compromising alignment principles [35]. Functional alignment (FA) and restricted kinematic alignment (KA) approaches further refine outcomes by harmonizing individual anatomical variations with biomechanical demands. Sarzaeem, 2024 demonstrated that kinematic alignment outperforms mechanical alignment in terms of gait restoration and postoperative functional outcomes [36]. Similarly, studies by Liu et al. and Wang et al. reported the superiority of KA over mechanical alignment during medium- to long-term follow-up, attributing this to KA’s ability to preserve the native alignment of the hip, knee, and ankle, thereby facilitating a more natural gait pattern [37,38].
Mizu-uchi H, et al. and Ollivier B, et al. highlighted the potential of such hybrid strategies in achieving optimal results preserving gait functionality without compromising on long-term implant survival [39,40].
Limitations of the Current Evidence
Despite the promising findings, several limitations can be noted in the present systematic analysis. Significant heterogeneity exists in how KA and MA were defined and executed across studies. Varying outcome measures and assessment timelines limit meta-analytic synthesis. There remains a lack of large-scale, multicentric RCTs with >10-year follow-up comparing both techniques directly. Gait analysis protocols and technologies differ widely, reducing comparability. Additionally, most studies were conducted in high-income countries, which may not fully represent outcomes in resource-limited settings where rehabilitation and surgical instrumentation vary.
Conclusion
KA in total knee arthroplasty demonstrates clear benefits in restoring natural gait patterns and promoting early functional recovery when compared to traditional MA. Patient-reported outcomes, including satisfaction and joint awareness, are also higher in the short to intermediate term. While long-term differences in implant longevity and function appear minimal, the individualized approach offered by KA makes it a compelling alternative to MA. Future research should focus on harmonizing definitions, standardizing outcome measures, and conducting longterm RCTs in diverse populations to better delineate the benefits and limitations of both alignment philosophies.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article
Funding
The authors received no financial support for the research, authorship, and/or publication of this article
References
- Bonnefoy Mazure A, Lübbeke A, Miozzari HH, Armand S, Sagawa Y Junior, et al. (2020) Walking speed and maximal knee flexion during gait after total knee arthroplasty: Minimal clinically mportant improvement is not determinable; patient acceptable symptom state is potentially useful. Journal of Arthroplasty 35(10): 2865-2871.e2.
- Blakeney W, Clément J, Desmeules F, Hagemeister N, Rivière C,et al. (2019) Kinematic alignment in total knee arthroplasty better repro- duces normal gait than mechanical alignment. Knee Surg Sports Traumatol Arthrosc 27(5): 1410-1417.
- Vendittoli PA, Blakeney W (2017) Redefining knee replacement. Orthop Traumatol Surg Res 103(6): 977-979.
- Oussedik S, Abdel MP, Victor J, Pagnano MW, Haddad FS (2020) Alignment in total knee rthroplasty. Bone Joint J 102-B (3): 276-279.
- Howell SM, Papadopoulos S, Kuznik KT, Hull ML (2013) Accurate alignment and high function after kinematically aligned tka performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 21(10): 2271-2280.
- An VVG, Twiggs J, Leie M, Fritsch BA (2019) Kinematic alignment is bone and soft tissue preserving compared to mechanical alignment in total knee arthroplasty. Knee 26(2): 466-476.
- Bechard DJ, Birmingham TB, Zecevic AA, Jones IC, Giffin JR, et al. (2012) Toe-out,lateral trunk lean, and pelvic obliquity during prolonged walking in patients with medial compartment knee osteoarthritis and healthy controls. Arthritis Care Res (Hoboken) 64(4): 525-532.
- Sehgal A, Burnett R, Howie CR, Simpson AHRW, Hamilton DF (2021) The use of pedobarographic analysis to evaluate movement patterns in unstable total knee arthroplasty: A roof of concept study. Knee 29: 110-115.
- Mercuri JJ, Pepper AM, Werner JA, Vigdorchik JM (2019) Gap balancing, measured resection, and kinematic alignment: How, when, and why. JBJS Reviews 7(3): e2.
- Haddaway NR, Page MJ, Pritchard CC, McGuinness LA (2022) PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst Rev 18(2): e1230.
- Wang G, Zhang Y, Chen L, Yu G, Luo F, et al. (2024) Modified kinematic alignment better restores plantar pressure distribution than mechanical alignment in total knee arthroplasty: A randomized controlled trial. Scientific reports 14(1): 27775.
- Fernandez C, Brownell M, Eom R, Nwankwo T, Gulati J, et al. (2025) Patellar alignment compared between kinematic and mechanical unicompartmental knee arthroplasties. Journal of orthopaedics. 70: 77-81.
- Migliorini F, Maffulli N, Pilone M, Schäfer L, Ullmann D, et al. (2025) Mechanical versus kinematic alignment for total knee arthroplasty: A meta- analysis. Arch Orthop Trauma Surg 145(1): 212.
- McEwen P, Balendra G, Doma K (2019) Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. Bone Joint J 101-B(3): 331-339.
- Jamali AA, Shekhar A, Dungy D, Stewart SL (2024) Kinematic versus mechanical alignment: A systematic review of systematic reviews and meta-analyses of randomised controlled trials. J Exp Orthop 11(4): e70044.
- Parente A, Medetti M, Raineri D, Parente F, Ventura A,et al. (2023) Patellofemoral knee pain following total knee arthroplasty. comparison between adjusted mechanical and inverse restricted kinematic alignment. J Orthop 43: 121-124.
- Shekhar A, Dungy D, Stewart SL, Jamali AA (2023) Patient-reported outcomes of kinematic vs mechanical alignment in total knee arthroplasty: A systematic review and meta-analysis of randomized controlled trials. Arthroplasty today 21: 101127.
- Tian G, Wang L, Liu L, Zhang Y, Zuo L,et al. (2022) Kinematic alignment versus mechanical alignment in total knee arthroplasty: An up-to-date meta-analysis. Journal of orthopaedic surgery 30(3): 10225536221125952.
- Ettinger M, Tuecking LR, Savov P, Windhagen H (2024) Higher satisfaction and function scores in restricted kinematic alignment versus mechanical alignment with medial pivot design total knee arthroplasty: A prospective randomised controlled trial. Knee Surg Sports Traumatol Arthrosc 32(5): 1275-1286.
- Khan ZA, Leica A, Sava MP, Hirschmann MT (2024) No difference in postop- erative patient satisfaction rates between mechanical and kinematic alignment total knee arthroplasty: A systematic review. Journal of experimental orthopaedics 11(3): e12101.
- Gibbons JP, Zeng N, Bayan A, Walker ML, Farrington B, et al. (2025) No difference in 10-year clinical or radiographic outcomes between kinematic and mechanical alignment in TKA: A randomized trial. Clinical orthopaedics and related research 483(1): 140-149.
- Karasavvidis T, Pagan CA, Debbi EM, Mayman D J, Jerabek SA, et al. (2024) No difference in limb alignment between kinematic and mechanical alignment robotic-assisted total knee arthroplasty. The Journal of arthroplasty 39(8S1): S200-S205.
- Young SW, Sullivan NPT, Walker ML, Holland S, Bayan A,et al. (2020) No difference in 5-year clinical or radiographic outcomes between kinematic and mechanical alignment in TKA: A randomized controlled trial. Clinical Orthopaedics and Related Research 478(6): 1271-1279.
- Elbuluk AM, Jerabek SA, Suhardi VJ, Sculco PK, Ast MP,et al. (2022) Head-to-head comparison of kinematic alignment versus mechanical alignment for total knee arthroplasty. J Arthroplasty 37(8S): S849-S851.
- Van de Graaf VA, Chen DB, Allom RJ, Wood JA, MacDessi SJ (2023) Functional alignment in total knee arthroplasty best achieves balanced gaps and minimal bone resections: An analysis comparing mechanical, kinematic and functional alignment strategies. Knee Surg Sports Traumatol Arthrosc 31(11): 5118-5127.
- Manara JR, Whitehouse SL, Marley M, Goonatillake M, Collopy D, et al. (2025) Functional alignment restores native kinematics more consistently than mechanical axis alignment in total knee arthroplasty. Bone Joint J 107-B(4): 423-431.
- MacDessi SJ, van de Graaf VA, Wood JA, Griffiths-Jones W, Bellemans J, et al. (2024) Not all knees are the same. Bone Joint J 106-B(6): 525-531.
- Oussedik S, Abdel MP, Cross MB, Haddad FS (2015) Alignment and fixation in total knee arthroplasty: Changing paradigms. Bone Joint J 97-B(10 Suppl A): 16-19.
- Fahima A Begum, Babar Kayani, Ahmed A Magan, Justin S Chang, Fares S Haddad (2021) Current concepts in total knee arthroplasty : Mechanical, kinematic, anatomical, and functional alignment. Bone & joint open 2(6): 397-404.
- McNair PJ, Boocock MG, Dominick ND, Kelly RJ, Farrington BJ, et al. (2017) A comparison of walking gait following mechanical and kinematic alignment in total knee joint replacement. J Arthroplasty 33(2): 560-564.
- Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML (2013) Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category. Clin Orthop Relat Res 471(3): 1000-1007.
- Tang J, Wu T, Shao H, Zhou Y (2022) Malposition of components and femorotibial mechanical axis changes on pressure distribution in total knee arthroplasty. Clinical Biomechanics 96: 105659.
- Yoon JR, Han SB, Jee MK, Shin YS (2017) Comparison of kinematic and mechanical alignment techniquesin primary total knee arthroplasty: A meta-analysis. Medicine 96(39): e8157.
- Sikorski JM (2008) Alignment in total knee replacement. J Bone Joint Surg Br 90(9): 1121-1127.
- McEwen P, Balendra G, Doma K (2019) Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. Bone Joint J 101-B(3): 331-339.
- Sarzaeem MM, Movahedinia M, Mirahmadi A, Abolghasemian M, Tavakoli M,et al. (2024) Kinematic alignment technique outperforms mechanical alignment in simultaneous bilateral total knee arthroplasty: A randomized controlled trial. The Journal of arthroplasty 39(9): 22342240.
- Liu B, Feng C, Tu C (2022) Kinematic alignment versus mechanical alignment in primary total knee arthroplasty: An up- dated metaanalysis of randomized controlled trials. Journal of Orthopaedic Surgery and Research 17: 201.
- Wang G, Chen L, Luo F, Luo J, Xu J (2024) Superiority of kinematic alignment over mechanical alignment in total knee arthroplasty during medium- to long-term follow- up: A meta-analysis and trial sequential analysis. Knee Surg Sports Traumatol Arthrosc 32(5): 1240-1252.
- Mizu-Uchi H, Ma Y, Ishibashi S, Colwell CW Jr, Nakashima Y, et al. (2022) Tibial sagittal and rotational alignment reduce patellofemoral stresses in posterior stabilized total knee arthroplasty. Scientific Reports 12(1): 12319.
- Ollivier B, Luyckx T, Stragier B, Vandenneucker H (2025) Kinematic alignment adequately restores trochlear anatomy, patellar kinematics and kinetics in total knee arthroplasty: Asystematic review. Knee Surg Sports Traumatol Arthrosc 33(2): 606-620.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.