Clinical recovery of symptoms after administration of long- acting treatment with injectable aripiprazole through recovery of inflammatory processes in parts of the brain and imaging results of brain CT scan of a patient of the field of Forensic Psychiatry with serious traumatic brain injury caused by a gunshot before and after undergoing neurosurgery
by Emmanouil L Pasparakis1,2*, Erasmia I Koiliari1,2, Antonios Vakis3,4
1Laboratory of Alcohology, Department of Pathology, Medical School of the University of Crete, Greece.
2Department of Psychiatry, General Hospital of Agios Nikolaos, Greece.
3Medical School, University of Crete, Heraklion, Crete, Greece
⁴Department of Neurosurgery, Heraklion University Hospital, Greece
*Corresponding author: Emmanouil L Pasparakis, Department of Psychiatry, General Hospital of Agios Nikolaos and Laboratory of Alcohology, Department of Pathology, Medical School of the University of Crete, Greece. Email: emmanouilpasparakis@gmail.com
Received Date: October 10, 2025
Accepted Date: October 17, 2025
Published Date: October 21, 2025
Citation: Pasparakis EL, Koiliari EI, Vakis A (2025) Clinical recovery of symptoms after administration of long-acting treatment with injectable aripiprazole through recovery of inflammatory processes in parts of the brain and imaging results of brain CT scan of a patient of the field of Forensic Psychiatry with serious traumatic brain injury caused by a gunshot before and after undergoing neurosurgery. J Neurol Exp Neural Sci 7: 165. https://doi.org/10.29011/2577-1442.100065
Case Presentation
Patient with pre-existing depressive disorder, which had led to social withdrawal and which had been adequately treated with per os administration of mirtazapine 30mg/day for four months, with full recovery of the functionality before the TBI, arrived at the Emergency Department of the General Hospital on duty in the capital of Crete (Greece), after being shot in the head with a pen gun while driving. He had had an argument with the driver of the vehicle who eventually shot him. During the first clinical examination, a left frontal parasagittal injury was found. On the Glasgow Coma Scale (GCS) the result was 13/15. This was assessed due to the aphasia of speech while he retained perception and presented right hemiparesis. When the patient was asked questions, he showed the manner of injury with his left hand. A brain CT scan was performed. The examination was performed in the context of an emergency. It was found presence of a metallic foreign body (bullet) intraparenchymally in the right parietal Lobe, without being able to assess its exact location. It is recognized in the left frontal bone at the height of the convexity, a hole of maximum width at the outer edge of the doublet of 1cm and at the inner edge of 1.9 cm, accompanied by numerous bone fissures and metallic fragments that enter outside the frontal lobe in a linear arrangement, while to a small extent they cross the interhemispheric fissure and extend to the contralateral frontal lobe. It is noted that numerous metal fragments are identified both on the scalp at the height of the hole and within the hole. The above findings argue in favor of the entry portal. Acute hemorrhagic elements in the form of parenchymal contusions are identified at the entry portal and along the bony fissures and to a significant extent along the entire length of the interhemispheric fissure, in the stellate and in the peripheral subarachnoid space of the right cerebral hemisphere with complete elimination of the sulci in series. There is a significant reduction in the width of the ventricular system, especially the right lateral and 3rd ventricles. After brain CT he was taken to the operating room.
During the neurosurgical procedure, the following stages were performed: Left craniectomy, meningeal section and opening. A small puncture of the anterior part of the sagittal is found where the bleeding is successfully stopped. Wound closure in layers. He was taken under full sedation to the Intensive Care Unit (Figures 1-4, a and b).
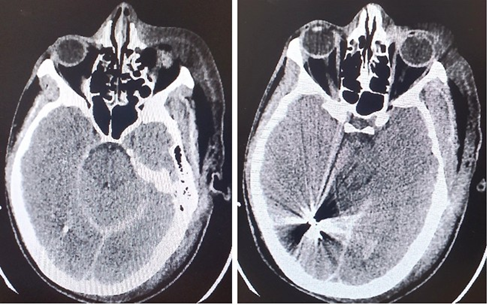
Figure 1(a and b): CT Brain scan 24 hours (1st day) after the brain injury and the neurosurgery.
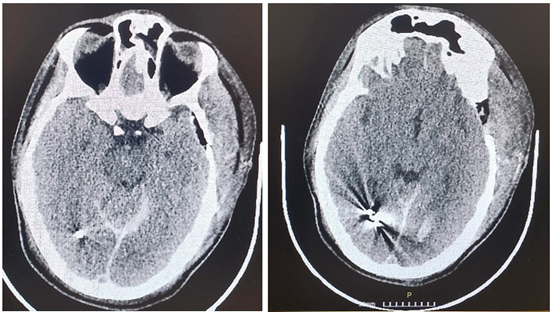
Figure 2(a and b): CT Brain scan 5 days after the brain injury and the neurosurgery.
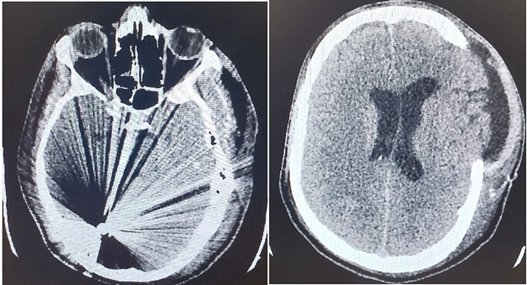
Figure 3(a and b): CT Brain scan 13 days after the brain injury and the neurosurgery.
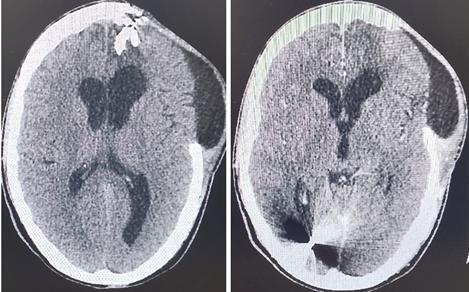
Figure 4(a and b): CT Brain scan 36 days after the brain injury and the neurosurgery.
After 36 days of hospitalization in the Intensive Care Unit and the Neurosurgery Clinic of the Hospital, the following were found: Stable and gradually evolving, a new brain CT scan (Figure 5, a and b) found movement of the object (projectile) posteriorly and on the occipital horn of the right ventricle, where its stay within it was confirmed in a CT scan five days after the neurosurgery. The patient developed neurologically very well. The GCS score was 15/15 with full capacity to speech. He was oriented to space, time, people. He had full capacity to stand and walk. The patient was discharged from the hospital with instructions to receive medication with tb Levetiracetam 500mg, 1x2. During his reintegration into the community, significant deficits in the efficiency of cognitive and executive functions, headaches, prevalence of depressive syndrome, significant decline in functionality and quality of life were observed. Exactly one year after the trauma and neurosurgery, the brain CT scan was performed again for monitoring reasons.
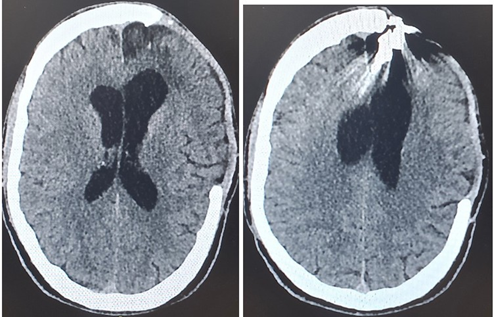
Figure 5(a and b): CT Brain scan 1 year after the brain injury and the neurosurgery.
After 13 months and 26 days from the day of the TBI, the patient underwent a treatment regimen with monthly administration of injectable aripiprazole with simultaneous intake of mirtazapine 30 mg/day, maintaining his Levetiracetam intake exactly as he was taking it. Gradual and satisfactory improvement in the patient’s cognitive and executive functions, emotion and functionality was observed, after the 3rd administration of depot treatment.
After 21 months and 19 days from the day of the TBI due to the gunshot and from the surgery and after 7 months approximatively from the beginning of the combination of Depot aripiprazole therapy and per os mirtazapine intake, a brain CT scan was performed. Based on the result of the examination: Craniotomy findings, left frontal. A hypodense area and calcified formations are identified in the left frontal with accompanying gliosis - parenchymal loss, with accompanying enlargement of the frontal horn of the left lateral ventricle. Metallic elements are identified in the right occipital, which cause significant false registrations (bullets). Without other foci of pathological density or pathological uptake of the contrast agent. The midline structures are checked without displacement. The width of the ventral system and the peripheral subarachnoid space are otherwise considered normal. Four months after the brain CT scan, the oral treatment was modified. Depot aripiprazole therapy has been maintained. Mirtazapine was discontinued and the patient started taking oral amitriptyline 25mg/day and perphenazine 2mg/day. After approximately 20 days, a satisfactory reduction in headache was observed, complete remission of depressive feelings, euphoric feelings, complete recovery of the patient’s functionality in all areas of his life and his complete socialization.
Discussion
The clinical case presents a young man, born in 1994, who develops emotional disorder with the character of depressive symptoms, accompanied by a significant impairment of executive functions and functionality, in general, in all areas of his life after suffering a severe TBI. It seems that the TBI a) significantly worsened the pre-existing condition of depression, which had been adequately treated with per os administration of mirtazapine 30mg/day, with full recovery of the patient’s functionality approximately 30 days before the TBI and b) caused a significant decline in executive functions, resulting in a marked decline in the patient’s functionality in all areas of his life and with marked social withdrawal. Depression is among the most pervasive and debilitating neuropsychiatric sequelae experienced by patients following a traumatic brain injury (TBI). While the individual pathophysiological mechanisms underlying depression and TBI have been widely studied, the neurobiological bases of depression after TBI remain largely unknown. Antidepressants are used for depressive syndromes, independent of the diagnoses, in SZ, in BD and MDD, among many others. Atypical antipsychotics are used for treatment of a variety of syndromes, independent of the particular diagnosis, such as delusions, hallucinations, anxiety, depression, agitation, sleep disturbances, and others. Atypical Antipsychotics (AAP) like aripiprazole, quetiapine, and olanzapine are also used for augmentation of Treatment-Resistant Depression (TRD) [1]. Besides the involvement of calcium signaling dysregulations in the pathophysiology of depression, there is some evidence of overexpressed CACNA1C (the gene encoding the Cav1.2 channels) following chronic stress in the brain regions, which involved in emotional and stress responses. Based on the data indicating the aripiprazole’s effects on intracellular calcium levels, a study in the rat stress-induced model of depression has demonstrated that the administration of aripiprazole could alleviate chronic stress-induced depressive-like symptoms. It could reduce immobility behavior, as well as reverse the elevated inflammatory cytokine, IL-6 in serum. Moreover, findings suggest that the antidepressant effects of aripiprazole are partly due to the inhibition of CACNA1C overexpression, restoration of BDNF and GAP-43 levels in the hippocampus and PFC, and increased hippocampal cells [2-3]. Also, evaluating the results of our studies [4-7] and guided by our clinical examination based on our medical skill and experience, we observe a gradual improvement in the clinical status of patients with psychosis and AUD/SUD, after the first two months of administration of the Depot aripiprazole therapy, such as their daily functionality, their affective and cognitive response to any form of everyday stimuli , in combination with the improvement of their quality of life and the reduction of their hospitalizations. The significant improvement and the stabilization of all the variables manifest into six months from the beginning of the therapy. Our patient’s symptoms improved significantly after treatment with Depot aripiprazole and per os mirtazapine, while the patients’ functionality and the quality of life improved particularly significantly within 20 days when mirtazapine was replaced by the combination of amitriptyline and perphenazine (25-2), keeping the daily dose of Levetiracetam constant and the monthly administration of long-acting (depot) aripiprazole.
References
- Stein F Kircher T (2025) Transdiagnostic findings across major depressive disorder, bipolar disorder and schizophrenia: A qualitative review. J Affect Disord 387: 119464.
- Dashti S, Nahavandi A (2022) Neuroprotective effects of aripiprazole in stress-induced depressive-like behavior: Possible role of CACNA1C. J Chem Neuroanat 126: 102170.
- Pasparakis E, Koiliari E, Zouraraki C, Tsapakis EM, Roussos P, et al. (2015) The effects of the CACNA1C rs1006737 A/G on affective startle modulation in healthy males. Eur Psychiatry 30(4): 492-498.
- Koiliari EI, Mouzas I, Alevizopoulos G, Lesch O, Walter H (2024) Longacting injectable aripiprazole in patients with psychosis is associated with improved quality of life, better general clinical outcome and fewer hospitalizations. European Psychiatry 67: S729.
- Koiliari EI, Mouzas I, Alevizopoulos G, Lesch O, Walter H, et al. (2025) Better treatment outcomes with aripiprazole long-acting injection in community and incarcerated patients with serious mental illness. Front Psychiatry 16: 1499400.
- Pasparakis EL, Mouzas I, Detorakis GI, Koiliari EI (2025) Analysis of 7. the therapeutic effect of the long-acting injectable form of aripiprazole in incarcerated adult males in Greece. European Psychiatry 68: S385-S385.
- Koiliari EI, Mouzas I, Detorakis GI, Pasparakis EL (2025) The use of depot antipsychotics in patients with dual diagnosis of psychosis and substance use disorder is associated with improved quality of life, better general clinical outcome and fewer hospitalizations. European Psychiatry 68: S429-S430.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.