Clinical Observation on the Efficacy of Pingle Guo’s Bone-Setting Manipulation Combined with Different Traction Methods in Treating Unstable Distal Radius Fractures
by Longfei Wen, Wei Li, Yan Zhang*
Orthopedic Department, Shenzhen Orthopedics Hospital, China
*Corresponding author: Yan Zhang, Orthopedic Department, Shenzhen Pingshan District Hospital of Chinese Medicine,Shenzhen Orthopedics Hospital, China; Lingnan University, Tuen Mun, New Territories, Hong Kong
Received Date: 11 August, 2025
Accepted Date: 19 August, 2025
Published Date: 21 September, 2025
Citation: Wen L, Li W, Zhang Y (2025) Clinical Observation on the Efficacy of Pingle Guo’s Bone-Setting Manipulation Combined with Different Traction Methods in Treating Unstable Distal Radius Fractures. J Orthop Res Ther 10: 1397. https://doi.org/10.29011/2575-8241.001397
Abstract
Objective: To compare the clinical effects of Pingle Guo’s orthopedic manipulation combined with neutral plate traction versus orthopedic manipulation combined with finger-cuff suspension traction in the treatment of unstable distal radius fractures. Methods: A prospective study was conducted on adult patients with unstable distal radius fractures treated in the Pingle Guo Orthopedics Department of Shenzhen Pingle Orthopedics Hospital from January to June 2024. Patients were divided into two groups: the experimental group received finger-cuff suspension traction, and the control group received neutral plate traction. The pre-reduction and post-reduction palmar tilt angle, ulnar deviation angle, radial height recovery, and Cooney wrist scores were recorded for both groups. Results: Before reduction, there were no statistically significant differences between the two groups in radiological indicators such as palmar tilt angle, ulnar deviation angle, radial height recovery, or Cooney wrist scores (p>0.05). After reduction, there were statistically significant differences between the two groups in terms of radial height recovery and Cooney score functional indicators (p<0.05). No significant differences were observed between the two groups in other indicators. Conclusion: Both neutral plate traction and finger-cuff suspension traction have good effects in the manual reduction treatment of patients.
Distal radius fractures (DRFs) represent the most common upper extremity fractures in middle-aged and elderly populations, accounting for 5.1% of all fractures and 48.37% of wrist fractures [1]. Treatment selection depends on fracture instability [2,3]. Radiographic indicators of instability necessitating surgical intervention include: dorsal comminution exceeding 50% of the dorsovolar distance, volar metaphyseal comminution, initial dorsal tilt >20°, initial translation >1 cm, initial shortening >5 mm, intra-articular involvement, concomitant ulnar fracture, and severe osteoporosis [4]. Although surgery achieves satisfactory reduction, complications such as loss of reduction, malreduction, extensor tendon irritation, hardware migration, traumatic arthritis, and functional impairment impede optimal outcomes [5,6].with distal radius fractures. However, finger-cuff traction is superior to neutral plate traction in terms of radial height recovery and functional outcomes, making it worthy of clinical application.
Keywords: Distal radius fractures; Finger-cuff suspension traction; Neutral plate traction
Objective
To compare clinical outcomes of Pingguo manual reduction combined with either finger trap suspension traction (FTST) or neutral plate traction (NPT) in unstable DRFs.
Methods
Design: Randomized controlled trial (60 patients; 30 per group).
Setting: Department of Orthopedics, Shenzhen Pingguo Orthopedic Hospital (Jan-Jun 2024).
Ethics: Approved by Institutional Review Board (No. KY2024010); written informed consent obtained.
Participants: Adults (>18 years) with unstable DRFs meeting ≥1 instability criterion. Exclusion criteria: open/pathological/old fractures, pre-existing dysfunction, inadequate closed reduction (radial shortening <2 mm, ulnar variance <5 mm, articular step-off <2 mm, volar tilt loss <10°), or cognitive impairment.
Interventions
a. FTST Group: Hematoma anesthesia with 1% lidocaine; 30-min gravity-assisted FTST followed by Pingguo reduction and splinting. Home-based FTST (1 hour, twice daily for 2 weeks).Outcomes
a. Radiographic: Volar tilt, ulnar inclination, radial height (pre-reduction, immediate post-reduction, 1/2/3 months).
Statistical Analysis
SPSS 24.0; χ²-test for categorical data; independent t-tests for continuous data (mean ± SD); significance at P < 0.05.
Results
1. Baseline radiologic parameters were comparable (P > 0.05). At 3 months:
- Both groups showed significant improvement in all parameters.
- FTST group exhibited superior radial height restoration vs. NPT (P < 0.05).
- No intergroup differences in volar tilt or ulnar inclination.
2. Functional outcomes (modified Cooney score):
- FTST group demonstrated better functional status (P < 0.05).
- No differences in pain, grip strength, dorsiflexion, or palmar flexion.
3. No adverse events occurred in either group.
Discussion
Conservative management remains valuable for DRFs, particularly for patients declining surgery. Our findings confirm that Pingguo manual reduction achieves satisfactory initial alignment, consistent with prior studies [8,9]. However, maintaining reduction is challenging due to loss of traction, cancellous bone defects, dorsal “negative support” [10], increased radiocarpal stress from radial shortening [11], muscle spasm, edema resolution, and early mobilization [11,12]. Radial shortening contributes to ulnar impaction, ulnocarpal impingement, restricted motion, and pain [13,14].
FTST provides sustained longitudinal traction, counteracting muscular forces and promoting fracture consolidation [7]. Both traction methods effectively reduced secondary displacement and reoperation risk. FTST’s superiority in restoring radial height and functional status may stem from greater axial traction force compared to NPT’s transverse mechanism. Preserved radial height mitigates distal radioulnar joint instability and ulnocarpal impingement, explaining FTST’s functional advantage.
Conclusion
Both FTST and NPT combined with Pingguo reduction are viable for unstable DRFs. FTST demonstrates superior efficacy in restoring radial height and functional outcomes, making it the preferable conservative option. Patient preference and informed consent remain crucial in clinical decision-making.
|
Group |
n |
Volar Tilt (°) |
UlnarInclinatin(°) |
Radial Height (mm) |
|||
|
Pre-red |
3mo Post |
Pre-red |
3mo Post |
Pre-red |
3mo Post |
||
|
FTST |
30 |
-13.52 ± 14.87 |
11.3 ± 6.67 |
14.1 ± 5.65 |
19.13 ± 4.98 |
-2.14 ± 3.64 |
3.75 ± 2.6 |
|
NPT |
30 |
-14.03 ± 15.13 |
10.0 ± 5.79 |
14.2 ± 4.15 |
18.87 ± 4.42 |
-2.44 ± 3.19 |
2.04 ± 2.82 |
|
*t*-value |
0.13 |
0.81 |
-0.08 |
0.21 |
0.34 |
2.45 |
|
|
P-value |
>0.05 |
>0.05 |
>0.05 |
>0.05 |
>0.05 |
<0.05 |
|
Table1: Comparison of the ulnar deviation angle, volar tilt angle, and shortening distance of the distal radius height between the two patient groups before reduction and 3 months after reduction based on X-ray image.
|
Group |
Pain |
Functional Status |
R |
OM |
Grip Stren |
||||
|
n |
Pre-red |
3mo Post |
Pre-red |
3mo Post |
Pre-red |
3mo Post |
Pre-red |
3mo Post |
|
|
FTST |
30 |
7.5± 7.63 |
22.67 ± 3.14 |
7.33± 8.07 |
23.83 ± 2.15 |
6.17 ±4.86 |
22.66± 4.3 |
5.83± 4.93 |
20.67 ± 5.04 |
|
NPT |
30 |
7± 7.61 |
21.83 ± 3.34 |
7.17± 7.84 |
22.32 ± 2.86 |
5.67 ± 3.88 |
20.66 ± 5.21 |
5.5± 4.42 |
20.83 ± 5.27 |
|
*t*-value |
0.25 |
1 |
0.08 |
2.32 |
0.44 |
1.62 |
0.27 |
-0.12 |
|
|
P-value |
>0.05 |
>0.05 |
>0.05 |
<0.05 |
>0.05 |
>0.05 |
>0.05 |
>0.05 |
|
Table 2: Comparison of Cooney wrist scores between two patient groups before reduction and 3 months after reduction.

Figure 1: Before reduction.
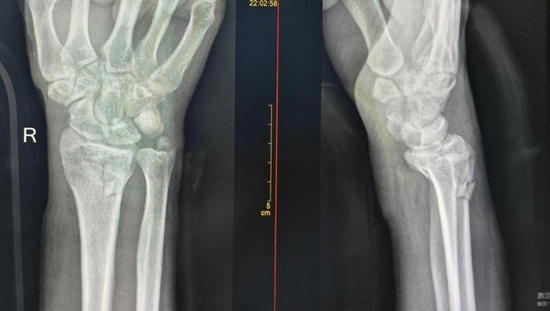
Figure 2: After reduction.

Figure 3: Two months after reduction.
Funding Statement
This work was supported by:
- Shenzhen Sanming Project for High-Level Medical Teams (Grant No. SZZYSM202108013)
- 2023 Pingshan District Health System Research Project, Shenzhen (Grant No. 2023218)
Author Contributions
Longfei Wen: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft.
Wei Li: Data curation, Formal analysis.
Yan Zhang: Supervision, Validation, Writing – review & editing, Project administration.
References
- Yu Chang (2010) Long Orthopedic Rehabilitation. People’s Medical Publishing House, China,391.
- S Terry Canale, James H Beaty (2013) Campbell’s Operative Orthopaedics. Trauma, 12th Edn, People’s Military Medical Press 6: 2683-2687.
- Tian Wei (2008) Practical Orthopedics. People’s Medical Publishing House, China, 422-429.
- Li Tao, Song Qizhi, Yang Shuhua (2010) Surgical treatment of unstable distal radius fractures. Chinese Journal of Traumatology 26(7): 602605.
- Jakob M, Rikli DA, Regazzoni P (2000) Fractures of the distal radius treated by internal fixation and early function. A prospective study of 73 consecutive patients. J Bone Joint Surg Br 82(3): 340-344.
- Wang Jiliang, Xu Jianzhong (2005) Advances in the treatment of distal radius fractures. Orthopedic Journal of China 13(16): 1260-1262.
- Yu Aorui (2022) Clinical study on finger trap traction combined with Pingle traditional bone-setting splint external fixation for distal radius fractures. Health Must-Read 27: 101-102.
- Nie Weizhi, Sui Xianyu, Hu Yali (2017) Research progress on noninvasive external fixation for Colles fractures. Chinese Journal of Traditional Medical Traumatology & Orthopedics 25(6): 79-82.
- Zhang Rongchao, Xu Weiguo, Jin Hongbin (2016) Research progress on conservative treatment of distal radius fractures with traditional Chinese medicine. Journal of Liaoning University of Traditional Chinese Medicine 18(4): 246-249.
- Keast-Butler, Schemitsch EH (2008) Biology versus mechanics in the treatment of distal radial fractures. J Orthop Trauma 22(8 Suppl): S9195.
- Markolf KL, Tejwani SG, Benhaim P (2005) Effects of wafer resection and hemiresection from the distal ulna on load-sharing at the wrist: a cadaveric study. J Hand Surg Am 30(2): 351-358.
- Qu Yuxing, Jiang Tao, Zhao Hong (2014) Treatment of distal radius fracture malunion with adjustable locking plate. Chinese Journal of Orthopaedics 34(7): 717-722.
- Wang Shuhuan, Wei Jianing, Tian Guanglei (1999) Hand Surgery. 2nd Edn, People’s Medical Publishing House, China, 303-309.
- Knirk JL, Jupiter JB (1986) Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am 68(5): 647-59.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.