Clinical Case of Bullet Removal with Robot-Assisted Surgery
by Ts Minchev*, A Angelov, S Bogdanov
ACC Tokuda Hospital, Sofia, Thoracic Surgery Clinic, Hospital in Sofia, Bulgaria
*Corresponding author: Ts Minchev, ACC Tokuda Hospital, Sofia, Thoracic Surgery Clinic, Hospital in Sofia, Bulgaria
Received Date: 23 March 2025
Accepted Date: 27 March 2025,
Published Date: 31 March 2025
Citation: Minchev T, Angelov A, Bogdanov S (2025) Clinical Case of Bullet Removal with Robot-Assisted Surgery. Ann Case Report. 10: 2235. DOI:10.29011/2574-7754.102235
Abstract
Thoracic trauma accounts for up to 35% of trauma-related deaths in the United States and encompasses a wide range of injuries that can cause significant morbidity and mortality. Rapid assessment during the primary trauma examination is key to identifying those injuries that are immediately life-threatening and require immediate intervention. Chest injuries are generally divided into penetrating and non-penetrating. Penetrating chest injuries most commonly occur from gunshots and stab wounds.
Penetrating thoracic trauma could present with a wide range of injuries, ranging from superficial injuries to injuries causing hemodynamic instability requiring immediate life-saving interventions. Even apparently stable patients with penetrating thoracic injuries can deteriorate rapidly, therefore, targeted clinical evaluation should be performed promptly.
Although penetrating chest trauma is more lethal than blunt trauma, most penetrating injuries do not require major surgical intervention and in many patients, management of these injuries involves conservative observation and serial evaluation, while some require only the placement of a chest tube. Approximately 15 to 30% of penetrating chest injuries require surgery, as opposed to less than 10% of blunt chest trauma injuries.
Incidence of penetrating chest trauma varies geographically. In the United States, penetrating chest trauma accounts for approximately 3% of all trauma-related deaths. In Europe, the incidence of penetrating trauma is reported to be as low as 4 percent. Urban centers tend to have higher rates of interpersonal violence and a correspondingly higher percentage of injuries involving penetrating mechanisms than rural areas. In countries or regions involved in hostilities, up to 95 percent of military deaths may result from a penetrating mechanism of injury.
The exact incidence of specific injuries caused by penetrating chest trauma is difficult to determine. Major vascular injuries occur in approximately 4 percent of patients with penetrating chest injuries. Penetrating tracheobronchial wounds are associated with concurrent esophageal injuries and major vascular damage in approximately 30% of cases. Cardiac injuries occur in 3% of patients with penetrating tracheobronchial wounds and are associated with high mortality.
Foreign bodies retained in the chest following penetrating chest trauma may include bullets, shrapnel, pieces of clothing, bones, and rib fragments. The risks of removing foreign bodies must be evaluated against the complications of leaving them in the chest.
Purpose
Our purpose is to present a case series of a man with a penetrating gunshot wound to the chest that required surgical removal nearly 30 years after the trauma. We would also like to emphasize that obliterated pleural cavity is not always a contraindication for minimally invasive surgery. We would also like to present robot-assisted surgery as a modern method for extracting foreign bodies from the chest and in old gunshot wounds.
Materials and Methods
We present a clinical case of a 53-year-old patient who was admitted for elective surgery due to the presence of a foreign body a bullet in the chest (Figure 1). The patient has undergone multiple surgeries due to the presence of disc herniations at different vertebral levels. Due to recurrent pain syndrome, it is necessary to perform an MRI to refine subsequent management. From a CT scan of the chest - data on a well-circumscribed metal object 28 mm from the arch of Th11 extrapulmonary to the right at the level of the 10th-11th intercostal space. According to anamnestic data, he was shot in April 1995, and then emergency surgical treatment was performed - a Rio-Branco laparotomy with suture of the liver and definitive hemostasis and the placement of chest tubes in the right pleural cavity.
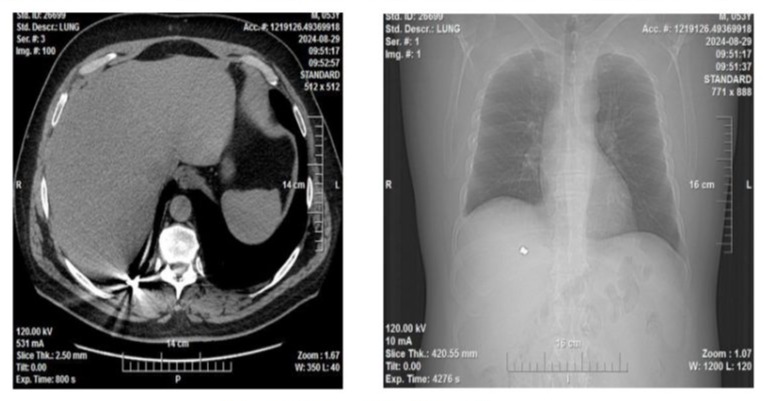
Figure 1: A foreign body a bullet in the chest.
Results
Operative time was 60 minutes due to the presence of multiple dense adhesions in the right pleural cavity of the lung to the chest wall and diaphragm. Hospital stay was 3 days. No intra- and postoperative complications were recorded (Figure 2). In the patient, the pleural drain was removed on 2 post-operative day with zero secretion and expanded lung parenchyma. Discharge was also on 2 post-operative day.
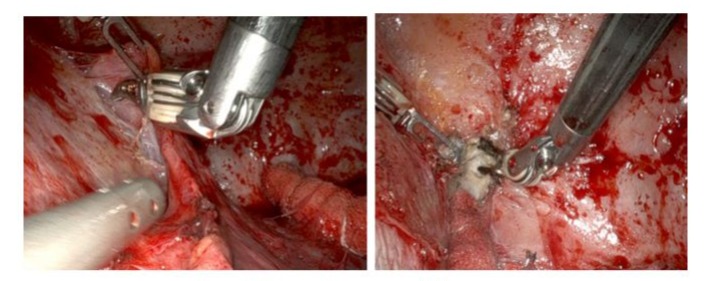
Figure 2: Robotic dissection and Bullet removal.
Discussion
Most often, penetrating chest injuries with foreign body retention in the chest do not require surgical treatment. A similar conclusion was reached by Sameh I Sersar et al. In their 2015 report, they described 90 cases of foreign body retention after penetrating chest injury, with only 12 of them requiring surgical removal. However, the removal of such foreign bodies can be challenging [1,2].
The presence of pleural adhesions could make it difficult to successfully perform the planned surgical intervention. Pleural adhesions are classified into 4 groups (mild, moderate, severe, very severe) [3,4] according to the percentage of dense adhesions - requiring acute separation with electrocoagulation or an energy device, and according to the percentage of adhesions from the total surface of the pleural cavity (Figure 3).
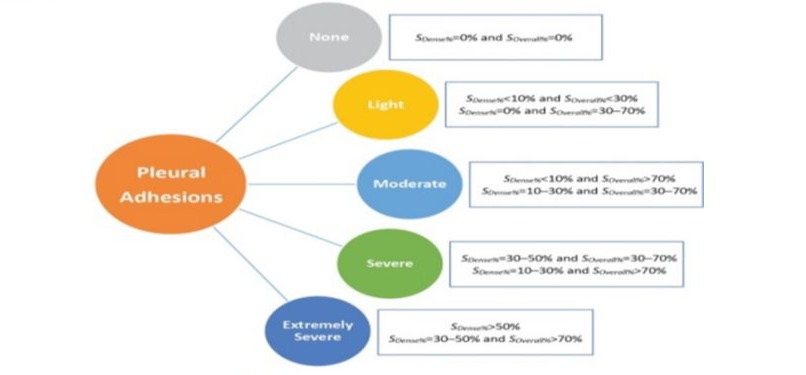
Figure 3: The total surface of the pleural cavity
In a 2018 article, Shuang-Jiang Li and co-authors confirmed that the presence of pleural adhesions is associated with a much higher risk of conversion to thoracotomy, postoperative complications, longer chest tubes stay, and longer hospital stay. Therefore, in the future, it would be good to develop an effective method for preoperative assessment of pleural adhesions – respiratory-dependent radiography and respiratory-dependent chest CT. In the literature, we found only two articles, similar to each other, on robot-assisted tracheal suture after gunshot wound as follows: Robotic Repair of Gunshot Injury to Trachea [5] by Ali Syed (Jan 2023) and Robot-assisted thoracoscopic repair of tracheal gunshot wound by Antoine Nehmе, Salman Zaheer, Alexander Leung (Apr 2024) [6].
There are many cases of foreign body removal with video-assisted thoracoscopy described - for example: Uniportal video-assisted thoracoscopic surgery for retained shrapnel in the thoracic cavity: An update surgical approach for removal of foreign body by Rawand Abdulrahman Essа [7].
Conclusion
Minimally invasive techniques are rarely used in patients with trauma requiring surgery, and there is very little literature on the application of robotic surgery in these patients. Currently, most studies involving the use of robots in trauma surgery have examined their use in orthopedic trauma. However, robotic surgery has been used in patients requiring emergency general surgery with promising results. Although not widely used in traumatic injuries, robot-assisted surgery has been used in the chest since at least 2001 for a growing number of indications and is associated with faster recovery times compared to open approaches for similar procedures. The use of a robot can assist surgeons performing correction of traumatic injuries by helping them gain access to difficult-to-reach areas such as the superior mediastinum, where a posterior thoracotomy or median sternotomy provides poor visualization and limited working space.
This report suggests that robotic surgery may be a safe and effective way to treat certain traumatic injuries to the chest.
Robot-assisted surgical technique is an extremely cutting-edge and innovative method, allowing visualization of the surgical field and surgical precision at a new, much higher level. It depends largely on the skills and experience of the surgeon. Future development of the methodologies and the accumulation of clinical experience will objectify the possibility of its application as one of the methods of choice in the surgical treatment of thoracic injuries.
References
- Julie M Winkle, MD, FACEP, FCCM, Eric Legome, MD (2024) Initial evaluation and management of penetrating thoracic trauma in adults.
- Sameh I S, Khalid A A, Hysam A (2016) Impacted thoracic foreign bodies after penetrating chest trauma. Asian Cardiovasc Thorac Ann. 24: 782-787.
- Shuang-Jiang L, Kun Z, Yan-Ming W, Ming-Ming W, Cheng S, et al (2018) Presence of pleural adhesions can predict conversion to thoracotomy and postoperative surgical complications in patients undergoing video-assisted thoracoscopic lung cancer lobectomy. J Thorac Dis. 10: 416-431.
- David F. S, Michael A. G, Lambros D. A (2023) Thoracic Trauma- Luke Edgecombe.
- Ali S (2023) Robotic Repair of Gunshot Injury to Trachea.
- Antoine Nehmе, Salman Zaheer, Alexander Leung (2024) Robot-assisted thoracoscopic repair of tracheal gunshot wound, Trauma Case Rep. 51: 1011023.
- Rawand Abdulrahman E, Sirwan Khalid A (2022) Uniportal video-assisted thoracoscopic surgery for retained shrapnel in the thoracic cavity: An update surgical approach for removal of foreign body. Ann Med Surg. 75: 103402.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.