Classification of Molar Extraction Sites for Immediate Dental Implant Placement Revisited: Additional Technical Note
by Satoshi Kato1*, George Kato2
1ZAGA Center Osaka, Kato Dental Clinic, Osaka, Japan
2Deputy hospital director, ZAGA Center Osaka, Kato Dental Clinic, Osaka, Japan
*Correspondence author: Satoshi Kato, ZAGA Center Osaka, Kato Dental Clinic, 4-17 Honmachi, Tondabayashi, Osaka 584-0093, Japan
Received Date: 26 October 2025
Accepted Date: 03 November 2025
Published Date: 05 November 2025
Citation: Satoshi Kato, George Kato (2025) Classification of Molar Extraction Sites for Immediate Dental Implant Placement Revisited: Additional Technical Note. J Surg 10: 11479 https://doi.org/10.29011/2575-9779.011479
Abstract
Success of a dental implant immediately installed into the fresh extraction socket could be possible under the initial implant stability attained. This paper adds two classes to the previously reported categorization system for molar extraction sites that illustrates extraction sockets based on available bone and structure inside the socket for stabilization of an immediately installed implant. Three classes, types A, B, and C, were initially used. Type A and B sockets depend highly on the condition of the inner septal bone. Wide diameter implants (WDIs) that can be engaged with the outer wall might be used in a type C socket because there is little or no septal bone. Two more classes, types D and E, are added. A type D socket does not allow implant stability with a WDI, which cannot be engaged in the outer wide periphery wall, has little to no septal bone, but one of the root sockets and buccal bone remain. A type E socket, for which a WDI cannot be used, has neither septal bone nor any root socket, but buccal bone remains. Treatment protocols and pertinent clinical cases are showed based on the classification of the socket according to the newly expanded categorization system.
Keywords: Compromised Extraction Socket; Molar Single Implant; Primary Stability; Single Tilted Implant
Introduction
To establish more predictable treatment protocols for immediate implant insertion might need classification of extraction sockets with simplicity and rationality [1-4]. Elian et al. reported a simple categorization of extraction sockets as classes 1, 2, and 3 depending on the level of buccal bone loss for implant placement regardless of the type of tooth [1]. This classification has been further developed into the esthetic zone [2,3] and into the classification of molars, [4] which might be considered the most difficult. Success of a dental implant immediately installed into the fresh extraction socket could be an alternative option to a delayed protocol [5,6]. One of the important factors to lead success of immediate implant placement might be initial stability of the implant with anchorage of peripheral bone. As Smith and Tarnow pointed out, [4] reaching primary stability might be hard due to anatomical limitations with poor visibility and bone quality. Therefore, these implants are inserted in the molar extraction socket in most cases. In cases in which implants are installed in an axial direction, the condition of the septal bone of the multi-rooted molar and the bone around the socket may be an important factor as an immediate loading procedure [4]. However, there are few reports of a tilted single implant of molars for immediate implant insertion to an extraction socket, [7,8] although there have been many reports of multiple implants [9,10]. It can be also true that there have been situations in which the delayed approach had to be chosen depending on the condition of the molar sockets that have no septal bone with endodontic, periodontic, root fracture furcation involvement, and/or specific anatomical tooth morphology. One of the reasons for selecting a delayed approach is that clinicians might believe that implants should not be placed immediately into an inflamed socket for fear of infection. However, there does not appear to be any problem with immediate insertion after appropriate treatment of infected sockets [10]. Another reason may that the case does not fit one of the categories in the previously reported classification [4]. The purpose of the present report was to help establish additional guidelines according to the new categorization of molar extraction sites for immediate dental implant placement and provide treatment protocols and pertinent clinical cases.
Classification of Molar Extraction Sites
In the original report, molar extraction sockets were divided into three classes (Figure 1a-c) [4]. A type A socket has sufficient septal bone to cover the coronal portion of the implant completely inside the bone. A type B socket has enough septal bone to secure the implant but not fully cover it. A type C socket does not have enough septal bone inside the socket, but a Wide Diameter Implant (WDI) can be stabilized with engagement of the peripheral bone walls of the socket (Figure 1c). Two more classes, type D socket and type E socket, are introduced. A type D socket does not allow implant stability with a WDI, which cannot be engaged in the outer wide periphery wall, has little to no septal bone, but has just one of the root sockets and buccal bone remains (Figure 1d). A type E socket does not allow implant stability with a WDI for the same reasons, and there is neither septal bone nor any root socket, but buccal bone remains (Figure 1e). The cases of Type D and Type E sockets experienced by the authors are shown in (Table 1). Surgery was performed by two surgeons who shared the same protocols.
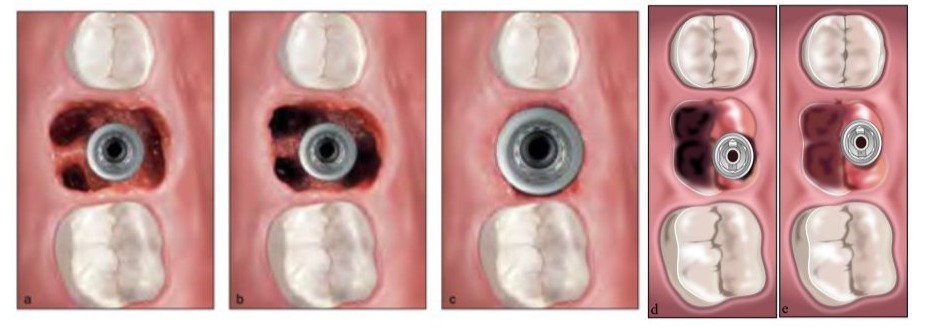
Figures. 1(a-e): a. A type A socket. An implant to fit completely for stability within the septal bone.
- A type B socket. An implant to fit for stability within the septal bone but to cover with bone incompletely.
- A type C socket. A WDI can be fixed within the socket wall and/or apical bone because no or incompletely septal bone for stability.
- A type D socket. Use of a WDI is not possible. No septal bone is available, but at least one of the root sockets remains. A WDI engages the socket. An extraction socket of palatal root often remains.
- A type E socket. Use of a WDI is not possible. No septal bone and no socket are available. A WDI is stabilized with axially or tiltedly remaining, lingual cortical or between palatal and bottom of the maxillary sinus cortical bone.
Discussion and Treatment Protocols
The treatment protocol for type A, B and C sockets from the previous report is as follows. A full-thickness flap should be avoided for significant ridge remodeling. Molars should be sectioned into individual roots to preserve septal bone as much as possible. The anatomy of the tooth might decide socket morphology and implant positioning. The vertical location of the immediate implant platform may be positioned on the most coronal side of the septal bone. The implant length depends on available bone and must be constrained by the position of the mandibular canal and maxillary sinus. The cement-enamel junction (CEJ) is connected to the implant platform width and the implant placement depth for a proper emergence profile (Figure 1g). A WDI (≥6 mm) may provide a predictable platform. Detailed descriptions for the treatment of type A, B and C sockets are available in the previous report (Figure 1a-c,f,g) [4].

Figure 1(f,g): f. Sectioned root each in maxillary first molar before extraction. g. An implant placement in the septal bone for adequate emergence profile.
The authors frequently encountered cases in which socket destruction is more advanced than that of a type C socket. They wondered whether it would be possible to perform immediate implant placement after tooth extraction in such cases, since there little to no septal bone and extensive socket bone loss, and they realized the necessity of the type D and type E socket categories, which are the basis for creating treatment protocols, and so proposed the addition of these two categories (Figure 1d,e). In some cases of type D or E sockets, which have a large horizontal bone defect, bone grafting or sinus lifting with full-thickness elevation using Autologous Platelet Concentrates (APC) and/or a buccal fat pad (BFP) in the maxilla may be considered at the same time [11-13]. Socket Preservation Technique (SPT) should be considered in type D and E sockets [14,15]. SPT should be considered even for type A, B, and C sockets with full thickness elevation and a maxillary sinus graft. The basic principles of these protocols are as follows. If necessary, a full-thickness flap is used. Molars should be sectioned into individual roots to preserve septal bone even if it there appears to be no septal bone for peripheral bone preservation. Implant positioning will be determined by the remaining available bone for stability with a high Insertion Torque Value (ITV). If even just one of the root sockets remains, it should be considered a good candidate for implant insertion. The vertical positioning of the immediate implant platform may be placed both in available bone itself and the trajectory toward an access hole on the occlusal table. However, in some cases with buccolingual tilting over 20° to the occlusal plane, an access hole may appear on the buccal side from the authors’ experience. The implant length depends on available bone and must be constrained by the position of the mandibular canal and the maxillary sinus. However, tilted implant technique can be chosen to avoid anatomical problems [79]. The CEJ is often not useful and is determined based on the height of the remaining surrounding buccal and lingual bone. Implant diameter and length might be determined according to the actual surgery. It is recommended to use tapered implants with a diameter ≥4.1 mm [16-18]. The following presents a discussion and treatment examples of a type D socket, and type E sockets.
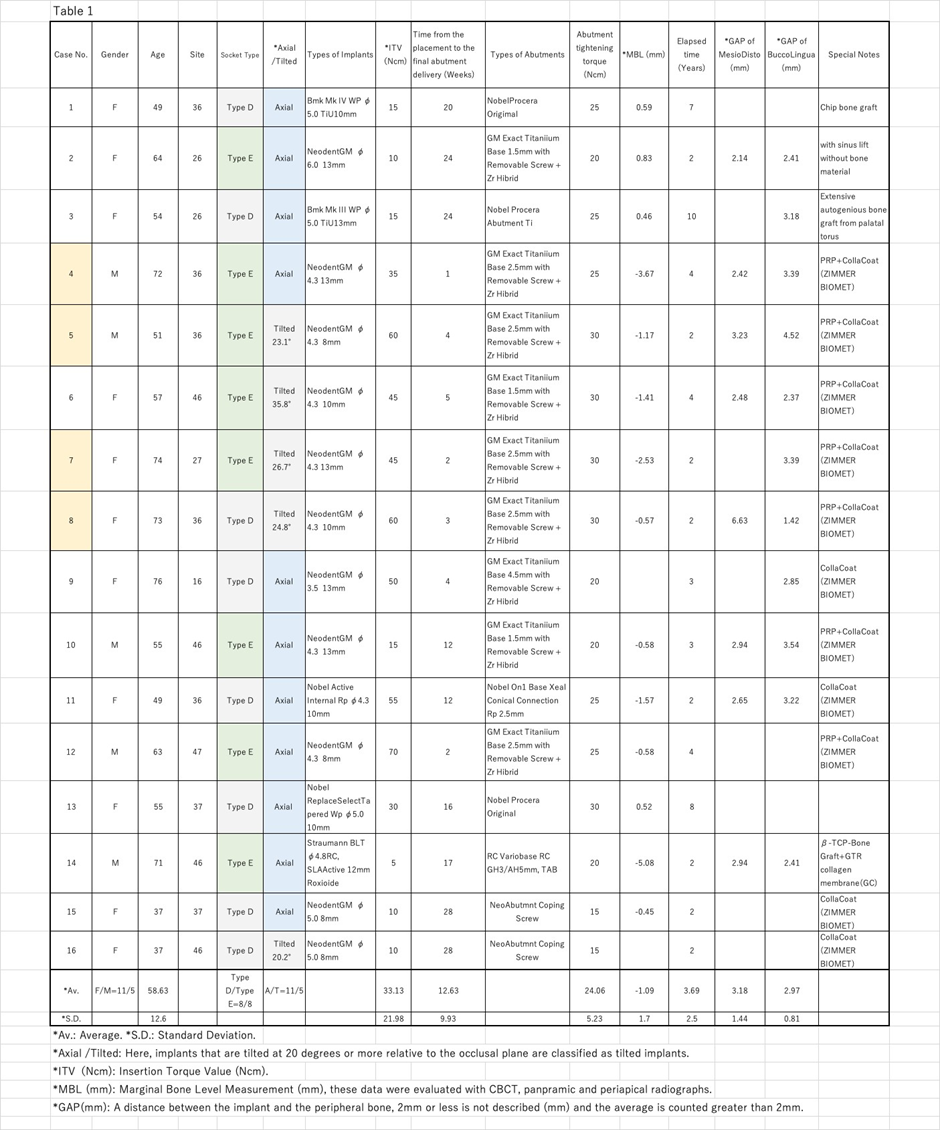
Treatment of a Type D Socket in the Mandible: Case 8
A type D socket does not allow implant stability with a WDI, which cannot be engaged in the outer wide periphery wall, has little to no septal bone, but one of the root sockets and buccal bone remains (Figure 2a,b). If even just one of the root sockets remains it should be considered a good candidate for implant placement (Figure 2a-d).
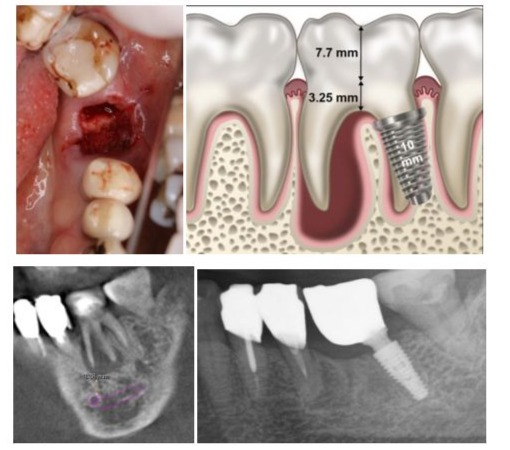
Figure s. 2a to 2d: a. A healthy 74-year-old female patient occupied housewife who visited for gingival swelling. A type D socket after the tooth extraction; b. A schema of an implant placement in the type D socket. A slight tilt might allow for the use of an implant longer than 10mm. The schema was created based on fig.3 of reference 4; c. A preoperative treatment plan with sagittal tomographic images. Fortunately, the distal root is small and short; d. A panoramic radiograph cut out 3 years after the surgery.
In many cases, full-thickness mucosal elevation is prepared to check for remaining alveolar bone, dissection of the socket and the narrow apical part of the root socket, and, in some cases, the socket may break during drilling, requiring a switch to type E socket treatment. However, there could be some problems with type D sockets, such as cantilever morphology leading to poor hygiene, food traps, irregularly screw access opening, and biomechanics that can arise when installing an implant into a residual root socket. The original report also explained that there will an erratically shaped crown with a cantilevered portion and/or a positioned screw access opening to redirect the opening [4]. The authors do the following to mitigate these shortcomings. For the cantilever morphology, before initial socket drilling, the bar should enter along the socket, correcting the direction of osteotomy toward the central occlusal table as much as possible, continuing until final drilling and installing the implant in the direction. These procedures improve screw access positioning, reducing the cantilever and allowing one to make closer to a regular crown shape. Regarding hygiene and food traps, during surgery, the buccal measurement and the height of the bone edge and the lingual side are recorded at the cantilever equivalent part, and based on them, the bone healing form is predicted. A form with a 3-mm mucosal thickness is added to this form, and a saddle-type shape that is slightly convex on the mucosal surface for easy access by dental floss is also added to the mucosal surface of the extension part according to this form (Figure. 2d) (in the case of final restoration placed within 3 weeks).
Regarding the biomechanical aspects, use of implants with a WDI is recommended [16-18]. An experimental study with finite element analysis reported that a defect of a single molar implant in the mandible with tilting compared with an axial type that tilted the implant by 17° doubled the von Mises stress transmitted to bone, and the highest rise was with an implant tilting at 45° in type 1 or type 2 bone. Therefore, a short implant axially placed could be a better alternative than titling a standard-length implant to support single crown restoration from a biomechanical point of view [21]. However, this study is purely experimental and not clinical, the authors have experienced many cases in which it was difficult to achieve initial stability with a short implant. Another study concluded that an implant tilted by 25 degrees can be used in the posterior region of the maxilla to replace a maxillary first molar without sinus penetration [22]. In any case, the implant-bone interface with a tilted implant received more stress than the straight one. However, the stability of peri-implant tissues, especially the marginal bone level in angulated implants of single-crown restorations, has not been extensively investigated. Zlatev et al. reported that the T-test of marginal bone loss between axial implants and angulated implants showed no statistically significant difference and concluded that single-unit prostheses can be a trustworthy restoration technique over angulated implants regarding to peri-implant marginal bone loss, but the angulated implant might bring merits to both patients and operators [8]. The other authors suggested that the differences in inclination of dental implants might not impact implant survival rate or marginal bone loss [23].
Treatment of Type E Sockets in the Mandible: Case 4 and 5.
In a type E socket, which does not allow implant stability with a WDI for the same reasons, there is neither septal bone nor any root socket, but buccal bone plate remains (Figure 3a). If the distance and bone quality to the mandibular canal or maxillary sinus allow insertion of an implant with possible high ITV, the implant can be inserted in the axial direction (Figure 3b,c).

Figures 3a to 3c: a. A case of healthy 72-year-old male patient retired who visited for tooth pain. A type E socket is apparent after tooth extraction; b. Mandibular molar without septal bone but existing axial bone tissue for implant stability with a sagittal tomographic image; c. A panoramic radiograph cut out after 4 years.
However, if insertion of the implant under that condition is not possible, the authors use tilted implants anchored to the lingual cortical plate of bone in the lower jaw and between the palatal cortical and lateral walls of the maxillary antrum cortical bone, avoiding maxillary sinus penetration (Figures 4a and 5a). One of the major concerns with the tilted implant procedure in the mandibular molar region can be perforation of the lingual cortical bone, possibly leading to serious hemorrhage [24,25]. Two important things must be done to prevent these complications. The first is precise preoperative diagnosis using CBCT with virtual implant simulation. The location of the implant platform is decided from the inferior alveolar nerve, both buccal and lingual bone crests, and the opposite tooth. Implant tilting, width, and length are also simulated based on the perforation point to the lingual cortical plate of bone at the same time (Figure 4b). The second is sufficient mucoperiosteal flap elevation in the surgery (Figure 4a). Elevation far beyond the expected perforation point is recommended for placing a mucosal dissector or saline-soaked gauze for soft tissue protection against the apex of preparation drills (Figure 4a). If these two things are appropriately done, it is the authors’ view that complications will never occur. The major advantage of this method is that it can achieve reliable initial stability with high ITV (more than 40 Ncm) [27,28]. When placing implants to cortical plate of bone with increased ITV of more than 40 Ncm, decreased or absent micromotion might help achieve predictable osseointegration [28]. This can lead to complete early final restoration, and, ultimately, the treatment period is shortened [28,29]. It has been reported that a definitive screw-retained prosthesis with zirconia was placed on standard and zygomatic implants for an edentulous maxilla seven days postoperatively [31]. Soft tissue of post-surgical healing around an implant appears to be completed after 2 weeks, and structural integrity is complete at the same time (about 2-3 weeks). Maturation of barrier function requires 6-8 weeks of healing [32]. This is based on the authors’ hypothesis that the goal is to improve barrier function by providing a highly biocompatible final prosthesis early on (2-3 weeks) and avoiding the need to attach and remove the implant abutments during soft tissue barrier maturation of 6-8 weeks post-surgically. After tooth extraction and immediate implant placement, the bone undergoes significant modeling in the edentulous ridge of the alveolar process, resulting in a decrease of the ridge dimension [19]. Moreover, when a flap procedure has been added, bone modeling might be accelerated. Regarding to the space distance between an implant and the adjustment bone wall, if the space is >2 mm, the site ought to be grafted with primary closure. In contrast, even if the space is >2 mm, success of the implant may be attained with no primary closure, no grafting, and no flap elevation [4]. In type D and E sockets, flap elevation might be required; thus, aggressive SPT is recommended if the gap is ≥3
mm [15,15,33,34]. Moreover, the implant platform can be located 0.5-1.0 mm below the line connecting the crest of buccal bone and the crest of lingual bone (Figure 4a,b) [34]. In many cases, the height of the crest of buccal bone is located below the crest of lingual bone, and the line tilts buccally, so that the implant will be also tilted buccally (Figure 4a-e). Fixation to the lingual cortical plate of bone may be required.
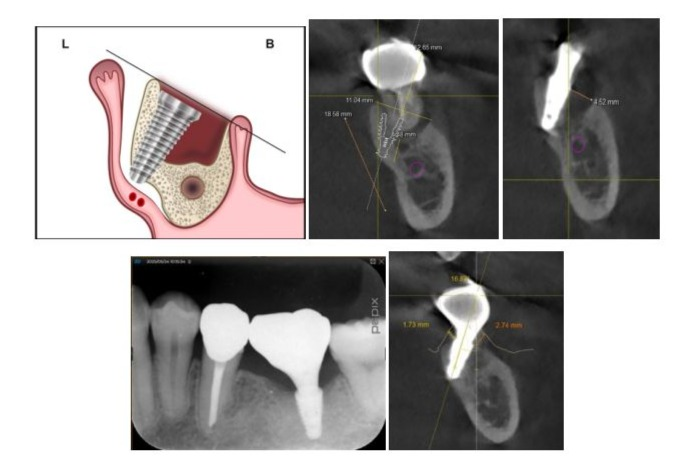
Figures 4a to 4e: a. A schema of a type E socket: L, Lingual and B, Buccal. Please pay attention to the position of the implant platform; b. A treatment plan with coronal sectional image for a case of healthy 51-year-old male patient company employee who visited for tooth pain. A type E socket without any septal and root sockets. Furthermore, there might be a lack of axial bone required for initial stability; c. Existing gap of about 5 mm; d. A periapical radiograph after 3 years; e. Soft tissue thickness of about 3 mm observed on the new bone into the gap.
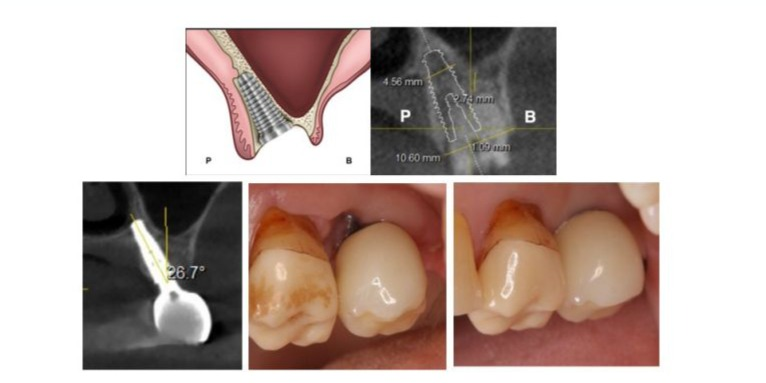
Figures. 5a to 5e: a. A Schema of a type E socket: P: Palatal and B: Buccal;b. A treatment plan with coronal sectional image for a case of healthy 73-year-old female patient occupied housewife who visited for tooth pain for an implant placement in the type E socket; c. The implant with a 26.7-degree angle to the occlusal plane with sectional image 3 years after the surgery; d. Buccal view at the time of restoration with soft tissue placed 2 weeks after the surgery; e. Buccal view of the restoration with soft tissue 12 weeks after the surgery.
Treatment of a Type E Socket in the Maxilla: Case 7.
The tilted implant in a type E socket in the maxilla might have a higher ITV than an axial implant. The reason is that, whereas axial implants rely on the cortical bone plate of the maxillary sinus floor alone for stability, a tilted implant can be inserted into the region surrounded by two or three walls: the lateral cortical bone of the maxillary sinus floor, the cortical bone plate of the palate, and sometimes the cortical plate of bone on the nasal cavity floor (Figure. 5a-c). Therefore, a longer implant and higher ITV than an axial implant can be expected, if anatomical conditions permit. Under these circumstances, minimal flap or flapless elevation under good visibility would be possible. The soft tissue depression created at the time of surgery appears to gradually return to a normal shape over a period of approximately 6 to 12 months as bone forms in the gap area (Figure 5d,e).
Conclusion
Two new categories added to the classification system for molar extraction sites were presented. This classification system describes the types of extraction sockets available to accept implants and helps facilitate communication among clinicians more than ever. Treatment protocols can be recommended based on the characteristics of the sockets with this system. Immediate implants can be placed in molar sockets if primary stability is achieved under completely covered (type A socket) or partially covered (type B socket) within the septal bone or by engaging the peripheral walls of the socket (type C socket). When there is little to no septal bone, immediate implants may be placed by engaging any remaining extraction socket (type D socket), or by engaging axially remaining bone above the mandibular canal, lingual cortical plate of bone in the mandible or between the palatal cortical bone and the cortical plate of bone on the side wall in the maxillary sinus with a tilting implant with high ITV (type E socket). If, however, the buccal bone plate is missing, a conventional delayed protocol should be used.
References
- Elian N, Cho SC, Froum S, Smith RB, Tarnow DP (2007) A simplified socket classification and repair technique. Pract Proced Aesthet Dent 19: 99-104.
- Tarnow DP, Chu SJ, Salama MA, Stappert CF, Salama H, et all (2014) Sarnachiaro GO, Sarnachiaro E, Gotta SL, Saito H. Flapless postextraction socket implant placement in the esthetic zone: part 1. The effect of bone grafting and/or provisional restoration on facial-palatal ridge dimensional change – a retrospective cohort study. Int J Periodontics Restorative Dent 34: 323-331.
- Chu SJ, Sarnachiaro GO, Hochman MN, Tarnow DP (2015) Subclassification and clinical management of extraction sockets with labial dentoalveolar dehiscence defects. Compend Contin Educ Dent 36: 516, 518-520, 522 passim.
- Smith RB, Tarnow DP (2013) Classification of molar extraction sites for immediate dental implant placement: technical note. Int J Oral Maxillofac Implants 28: 911-916.
- Smith RB, Tarnow DP, Sarnachiaro G (2019) Immediate placement of dental implants in molar extraction sockets: an 11-year retrospective analysis. Compend Contin Educ Dent 40: 166-170.
- Ragucci GM, Elnayef B, Criado-Cámara E, Del Amo FS, HernándezAlfaro F (2020) Immediate implant placement in molar extraction sockets: a systematic review and meta-analysis. Int J Implant Dent 6: 40.
- Kawasaki T, Komatsu K, Tsuchiya R (2011) Tilted placement of tapered implants using a modified surgical template. J Oral Maxillofac Surg 69: 1642-1650.
- Zlatev S, Ivanova V, Chenchev I, Todorov R, Chenchev L (2020) Crestal bone loss around tilted or axial implants with single unit restorations. Journal of Dental and Medical Sciences 19: 6-9.
- Krekmanov L, Kahn M, Rangert B, Lindström H (2000) Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants 15: 405-414.
- Yang H, Luo D, Yuan MJ, Yang JJ, Wang DS (2023) Five-year outcomes of immediate implant placement for mandibular molars with and without chronic apical periodontitis. World J Clin Cases 11: 5224-5235.
- Moraschini V, Barboza ES (2015) Effect of autologous platelet concentrates for alveolar socket preservation: a systematic review. Int J Oral Maxillofac Surg 44: 632-641.
- El-Haddad SA, El-Shall MA (2017) Two-year clinical evaluation of pedicled buccal fat pad alone and with Emdogain for root coverage of severe gingival recession defects: A case series. Int J Periodontics Restorative Dent 37: 901-907.
- Nascimento RD, Gonçalves TS, Cardoso PE, de Moraes MB, Raldi FV (2020) Use of buccal fat pad in the treatment of peri-implant mucosal defect: a case report. J Oral Implantol 46: 128-132.
- Clementini M, Agostinelli A, Castelluzzo W, Cugnata F, Vignoletti F, et all (2019)The effect of immediate implant placement on alveolar ridge preservation compared to spontaneous healing after tooth extraction: Radiographic results of a randomized controlled clinical trial. J Clin Periodontol 46: 776-786.
- Avila-Ortiz G, Chambrone L, Vignoletti F (2019) Effect of alveolar ridge preservation interventions following tooth extraction: A systematic review and meta-analysis. J Clin Periodontol 46: 195-223.
- Hadaya D, Pi-Anfruns J, Bellon B, Pippenger BE, Aghaloo TL (2022) Immediate loading of a fully tapered implant with deep apical threads placed in healed alveolar ridges vs. immediate extraction sockets. Clin Oral Implants Res 33: 501-510.
- Vandeweghe S, Hattingh A, Wennerberg A, Bruyn HD (2011) Surgical protocol and short-term clinical outcome of immediate placement in molar extraction sockets using a wide body implant. J Oral Maxillofac Res 3: e1.
- Ding X, Zhu XH, Liao SH, Zhang XH, Chen H (2009) Implant-bone interface stress distribution in immediately loaded implants of different diameters: a three-dimensional finite element analysis. J Prosthodont 18: 393-402.
- Araújo MG, Linder E, Lindhe J (2011) Bio-Oss collagen in the buccal gap at immediate implants: a 6-month study in the dog. Clin Oral Implants Res 22: 1-8.
- Lundgren S, Johansson AS, Cricchio G, Lundgren S (2019)Clinical outcome and factors determining new bone formation in lateral sinus membrane elevation with simultaneous implant placement without grafting material: A cross-sectional, 3-17 year follow-up study. Clin Implant Dent Relat Res 21:827-834.
- Anitua E, Saez de Ibarra NL, Martín IM, Rotaeche LS (2022) Influence of implant tilting and length on the biomechanics of single-tooth restoration: a finite element analysis in atrophic mandible. Dent J 10: 77.
- Hamed HA, Marzook HA, Ghoneem NE, El-Anwar MI (2018) Angulated dental implants in posterior maxilla FEA and experimental verification. Open Access Maced J Med Sci 6: 397-401.
- Chrcanovic BR, Albrektsson T, Wennerberg A (2015) Tilted versus axially placed dental implants: a meta-analysis. J Dent 43: 149-170.
- Tomljenovic B, Herrmann S, Filippi A, Kühl S (2016) Life-threatening hemorrhage associated with dental implant surgery: a review of the literature. Clin Oral Implants Res 27: 1079-1084.
- Carreira-Nestares B, Urquiza-Fornovi I, Carreira-Delgado MC, Gutierrez-Díaz R, Sánchez-Aniceto G (2023) Clinical case and literature review of a potentially life-threatening complication derived from mouth floor hematoma after implant surgery. Eur Dent Res Biomater J 4:13-24.
- Sun Y, Hu S, Xie Z, Zhou Y(2023) Relevant factors of posterior mandible lingual plate perforation during immediate implant placement: a virtual implant placement study using CBCT. BMC Oral Health 23: 76.
- Trisi P, Todisco M, Consolo U, Travaglini D(2011) High versus low implant insertion torque: a histologic, histomorphometric, and biomechanical study in the sheep mandible. Int J Oral Maxillofac Implants 26: 837-849.
- Greenstein G, Cavallaro J (2017) Implant insertion torque: its role in achieving primary stability of restorable dental implants. Compend Contin Educ Dent 38: 88-95.
- Rieder D, Eggert J, Krafft T, Weber HP, Wichmann MG, et all (2016) Impact of placement and restoration timing on single-implant esthetic outcome – a randomized clinical trial. Clin Oral Implants Res 27:e8086.
- Lee J, Lim YJ, Kim B, Koo KT (2020) Early loading of mandibular molar single implants: 1 year results of a randomized controlled clinical trial. Materials 13: 3912.
- Nicolopoulos C, Yuvanoglu P(2023) A Global ZAGA Mentor Experience In: Aparicio C (ed.). Advanced zygomatic implants; ZAGA concept, Quintessence, 308-311.
- Sculean A, Gruber R, Bosshardt DD (2014) Soft tissue wound healing around teeth and dental implants. J Clin Periodontol 41: S6-22.
- Tarnow DP, Chu SJ (2011) Human histologic verification of osseointegration of an immediate implant placed into a fresh extraction socket with excessive gap distance without primary flap closure, graft, or membrane: a case report. Int J Periodontics Restorative Dent 31: 515521.
- Covani U, Cornelini R, Calvo-Guirado JL, Tonelli P, Barone A (2010) Bone remodeling around implants placed in fresh extraction sockets. Int J Periodontics Restorative Dent 30: 601-607.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.