Case Report: Pentoxifylline Use for Inhibition of Significantly Increased Inflammatory Response in Preterm Infant with Diagnosed Late-Onset Sepsis.
by Agnieszka Ochoda-Mazur, Ryszard Lauterbach*, Dorota Pawlik, Małgorzata Jabłońska
Department of Neonatology Medical College Jagiellonian University Kraków Poland
*Corresponding author: Ryszard Lauterbach, Department of Neonatology Medical College Jagiellonian University Kraków Poland
Received Date: 07 January 2025
Accepted Date: 11 January 2025
Published Date: 15 January 2025
Citation: Ochoda-Mazur A, Lauterbach R, Pawlik D, Jablonska M (2025) Case Report: Pentoxifylline Use for Inhibition of Significantly Increased Inflammatory Response in Preterm Infant with Diagnosed Late-Onset Sepsis. Ann Case Report. 10: 2159. https://doi.org/10.29011/2574-7754.102159
Introduction
Sepsis is still one of the leading causes of neonatal morbidity and mortality. This ap-plies especially to prematurely born children. The risk of death from sepsis in very low birthweight infants is approximately 120 times higher compared to the full-term new born population [1]. An important factor increasing the risk of death during sepsis is the markedly increased inflammatory response occurring particularly in the body of the prematurely delivered infants.
Late-onset sepsis (LOS) is defined as an episode of sepsis after the first 72 hours of life. It is difficult to diagnose sepsis in preterm infants because of the scarcity of clinical symptoms characteristic of the disease and their low specificity. The similar clinical signs such as respiratory distress, apnea, bradycardia, as well as body temperature instability or cyanosis are observed in various of pathologies associated with immaturity of the body. Therefore, to confirm the initial diagnosis of sepsis, biochemical markers of inflammation should be measured and blood cultures performed. According to Kashlan et al. [1] the elevated serum concentration of interleukin-6 (IL-6) is the earliest marker of systemic infection in the new born. It is released into the blood by many cells as early as in the second hour after the onset of bacteriemia. Particularly strong inflammatory response, confirmed by high serum concentration of IL-6 is found in premature infants [2]. A recent analysis of 480 episodes of LOS diagnosed in 208 preterm neonates born below 32 weeks of gestational age showed that increased IL-6 serum concentrations were associated with sepsis severity and mortality risk [3].
Postnatal bacterial infections, regardless of the results of the blood cultures, are generally accepted as an important risk factor, that may cause widespread abnormalities of brain development in preterm infants [4]. It was found that inflammatory response due to sepsis may impair the process of myelinization and in turn either disrupts the white matter tissue development, or inhibits brain growth, which increases the risk of attentional performance in preterm infants [5]. Also, Giordano and co-authors [6] suggested that neonatal sepsis might be a risk factor for behavioural abnormalities observed at the age of 5 years in former very low birth weight infants.
At this point, the question arises whether we should routinely enter an anti-inflammatory drug into the treatment of neonatal sepsis to lessen the risk of organ damage and death. In this case, the promising candidate, which exerts several antioxidant and anti-inflammatory activities seems to be pentoxifylline (PTX), a methylxanthine derivative, a non-specific phosphodiesterase inhibitor. This drug has a protective effect on endothelium cells and reduces the development of severe coagulation cascade triggered by proinflamma-tory cytokines what allows for maintaining tissue perfusion and avoiding severe hypoxia. Recently, the results of several experimental and clinical studies were published, providing evidence for neuroprotective effects of PTX [7-11].
The studies of administration of PTX as an adjunct to antibiotic therapy of sepsis, dates in our neonatal department to the period between 1994 - 1999, when we published the results of the first prospective, randomized, double-blind, placebo-controlled study on the effectiveness and safety of PTX in the treatment of neonatal sepsis [12].During subsequent several years of clinical observation, after collecting data and experience, we made modifications and determined different schedules for PTX administration in septic neonates. They were based principally on the clinical symptoms and the results of different biochemical analyses including the perfusion disorders (capillary refill time > 3 seconds), metabolic acidosis, activity of protein C and presence of coagulation disorders, occurring during sepsis. In 2016, we published the results of sepsis therapy, diagnosed in very low birth weight infants [13]. Among the 458 infants with confirmed sepsis both EOS and LOS (median birthweight 1010g; median gestational age: 29 weeks), death occurred in 19 of those patients (4.2%).
This article reports the case of severe LOS, caused by Gram negative bacteria Enterobacter hormaechei followed by extremely rare pneumonia caused by Elisabethkingia oenophiles in the neonatal period. The objective of this work is to present a case of sepsis with extremely increased blood IL-6 concentration with values up to 250.000 pg/ml whereas the cutt-off values for diagnosis, suggested by several authors, range from 40 to 80 pg/mL. Also, we present the efficacy and safety of a modified, significantly increased dosage of PTX, that we use to decrease this incredible inflammatory response.
Case Presentation
A premature male neonate was born at 34 + 2 weeks as the first twin. Due to premature rupture of the membranes (PROM) a cesarian section was performed. The Apgar score was 9 in the first and fifth minute after birth. During the next four hours patient gradually developed respiratory insufficiency. The child was admitted to the neonatal intensive care unit and nasal CPAP was introduced to provide non-invasive ventilation. The ultrasound examination revealed heterogenous picture of the lungs typical of transient tachypnea of the new born (B lines and double lung point). Echocardiogram presented a small, a hemodynamically non-significant ventricular a septal defect and spontaneously closed ductus arteriosus. Standard caffeine treatment was introduced, and ventilatory support was continued on high flow nasal cannulas with a FiO2 value of 0,21. For the next four days, the clinical condition of the patient remained stable, however on the 5th day of life (DOL) a sudden deterioration of respiratory and cardiovascular condition was observed.
Physical examination on the 5th DOL
The patient presented with tachycardia and perfusion disorders, and a prolonged capillary refill time (CRT >3 sec.).
Due to repeated episodes of apnea, the patient needed intubation followed by mechanical ventilation. As bloody gastric residues were found in the stomach before the intubation, pulmonary hemorrhage was suspected and eventually confirmed. A neurological examination was performed and firstly revealed increased muscle tension and anxiety which followed by a lack of reactivity. Cardiovascular system insufficiency presented as hypotension with a mean arterial pressure 30 mmHg (invasive evaluation). Echocardiogram revealed pulmonary hypertension and right ventricle insufficiency followed by renal failure (anuria on the 7th and 8th DOL, 0,4 ml/kg/day) Also, extensive pulmonary and brain oedema were diagnosed.
Laboratory results
Within the first 72 hours of life, the blood of IL-6 concentration was evaluated and showed normal values below 40 pg/ml. However, on the fourth day after birth, when the clinical deterioration occurred, the blood IL-6 concentration significantly increased up to a value of 29.919 pg/mL. Moreover, the next evaluation of serum Il-6 performed after 6 hours, showed a dramatic increase in concentration up to 246.463 pg/ml (Figure 1). At the same time, there was a discovery of metabolic acidosis (pH -7,1, BE – (-11,0 mmol/l), thrombocytopenia (42.000/µl) and severe anemia (Hb- 6,8 g/l, Ht- 20,3%). Also, a significantly increased value of INR (4,79), decreased fibrinogen serum concentration (1,0 ug/ml), reduced protein C activity (10,7%) and hypoalbuminemia (20,7 g/l) were present.
Ultrasound brain monitoring
Transfontaneal ultrasound examination performed on the 6th DOL showed intra-ventricular hemorrhage grade III bilaterally (Figure 2), increased resistance index values in the anterior and median cerebral arteries and inhomogeneous echo-structure of the white matter that evolved into periventricular leukomalacia of grade II. Sonography performed on the 11th DOL revealed focal lesions (subcortically in the temporal left lobe) that were marked as typical ultrasound signs for an abscess (Figure 3). These ultrasound findings were accompanied by generalized clonic seizures and hypertonia.
Treatment
The patient demanded intubation and administration of dopamine at a dose of 5 ug/kg/min. Also, transfusions of blood components (fresh frozen plasma, red blood cells concentrate, platelets) were performed. Furosemide, in the range of doses between 1 to 5 mg/ kg and infusion of bumetanide in a dose of 7 ug/kg/min were continued for 6 consecutive days.
Antibiotics
The empiric broad spectrum antibiotics: vancomycin in a dose of 30 mg/kg/day, given as a continuous 24-hour infusion and meropenem in a dose of 40 mg/kg, given in a 4-hour infusion and repeated every 8 hours were started immediately after drawing blood for culture examination. Enterobacter species was identified as a result of the blood culture testing. According to the results of the antibiotic sensitivity test, vancomycin was replaced with gentamycin at a dose of 4,5 mg/kg given every 36 hours.
Pentoxifylline
PTX was introduced on the first day of therapy, immediately after the laboratory results showed a significantly increased serum IL-6 concentration (29.919 pg/ml). An infusion was introduced for the administration of PTX with a dose of 5 mg/kg/hour. After 12 hours of continuous infusion of PTX, the consecutive evaluation of serum IL-6 level found a dramatic increase in the concentration of cytokine up to 246.463 pg/ml (4th/5th DOL). The dose of drug was increased by twofold (10 mg/kg/hour) and the infusion was continued until the serum IL-6 level decreased to 240 pg/ml (8th DOL). Then we returned to the previous dose of PTX (5 mg/ kg/h for 24 hours) and continued infusion until the 21st DOL to reach the normal values of serum IL-6 concentration. Because the results of ultrasound brain monitoring, performed on the 11th DOL, showed typical ultrasound signs for abscesses, PTX therapy in a dose of 2,5 mg/kg/h for 24 hours was extended for the next 2 weeks to prevent the possible local inflammatory response that might resulted in an immature brain impairment (Figure 4).
A systematic lung ultrasound examination during sepsis treatment resulted in a quick diagnosis of pneumonia (14th DOL). A chest X-ray performed on the next day confirmed earlier findings. The bronchoalveolar lavage culture was positive for two microorganisms: Stenotrophomonas maltophilia and Elisabethkingia oenophiles which is extremely rare in newborn. Determining antibiotic sensitivity allowed to establish treatment that consisted of ciprofloxacin administered in three doses of 10 mg/kg and trimethoprim-sulfamethoxazole administered every 6 hours in a dose of 4 mg/kg.
Due to the suspicion of central nervous system infection and the concurrent contraindication to lumbar puncture, the antibiotic therapy has been continued for three weeks. However, lumbar puncture performed on the 40th DOL (before the end of antibiotic treatment) revealed no abnormalities in cerebrospinal fluid.
Before the infant was discharged, a magnetic resonance imaging (MRI) of the brain and electroencephalography (EEG) were also performed. The MRI outcome examination was consistent with previous ultrasound observation. There were present consequences of heterochronic intraventricular and intraparenchymal bleeding which resulted in multifocal leukomalacia of the brain and cerebellum as well as the brain tissue immaturity.
The hospitalization was complicated by the necrotizing enterocolitis (Bell IIIA, 5th DOL) followed by ileus and gastroparesis. Full enteral feeding was eventually achieved at 40 days of life. The patient experienced cholestasis but he gradually recovered before being discharged. The peak serum concentrations of AST (110 U/l)/, ALT (84 U/l), GGTP (1488 U/l) and ferritin (3246 mcg/l) were observed between 14 and 30th DOL (Figure 5). Ursodeoxycholic acid administered orally in doses of 10 mg/kg every 12 hours and intravenous infusions of DHA (Omegaven 2 g/ kg/day for 2 weeks followed by 1 g/kg/day the next two weeks). Starting from the 47th DOL the serum concentration of liver enzymes gradually decreased until it reached normal values.
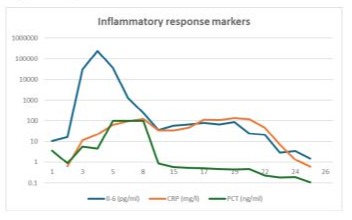
Figure 1: Inflammatory markers concentration noted on the following days of hospitalization.
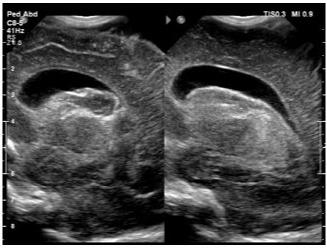
Figure 2: Ultrasound picture of IVH grade III.
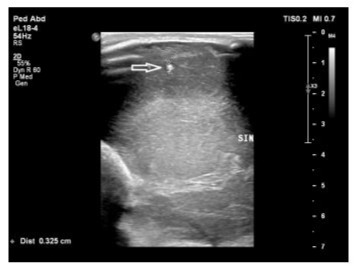
Figure 3: A focal lesion observed in parieto-temporal part of the left lobe of the brain.
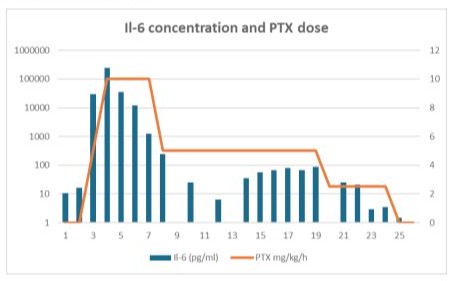
Figure 4: Pentoxifylline dosing according do Il-6 concentration during following days of hospitalization.
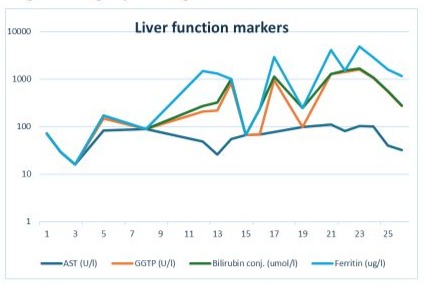
Figure 5: Liver function markers observed in the course of disease.
The extubation was performed on the 23rd DOL followed by synchronized non-invasive positive pressure ventilation and high flow nasal canula support until the patient was 46 days old. The serious unstable state of the patient led to retinopathy of prematurity which was treated with ranibizumab (Lucentis) single binocular injection.
Due to severe sepsis with an exclusively high serum IL-6 concentration that was followed by immediate pneumonia, we developed the diagnostic path for congenital immuno-deficiency syndromes by measuring the concentration of immunoglobulins followed by Next-generation sequencing (NGS). Although IgG serum level was low, NGS showed no pathologic syndromes. Further immunologic examination revealed no signs of congenital immunodeficiency syndromes.
The patient’s clinical condition was severe at the beginning of sepsis. Hypertonic, abnormal posture, the lack of reactivity and clonic seizures were observed. Anticonvulsants (phenobarbital, levetiracetam) and sedatives (ketamine, dexmedetomidine, midazolam) were adjusted according to the clinical state. The sucking reflex was restored during the transition to non-invasive ventilation (24th DOL). First attempts to bottle-feed were made on 40th DOL. Gradual progress in feeding was noted.
A neurologic consultant found no major abnormalities except for a tendency to hypertonia at the point of 42 weeks corrected age. Also, an EEG performed on the 55th DOL showed normal brain activity.
The infant was discharged on the 65th day of life with a referral to multidisciplinary ambulatory care.
A neurologic consultation performed on the 3rd month after patient was released from the hospital, found that he had normal righting reflexes and was forming a good eye contact. However, the head circumference was below the range of values for the 2rd percentile.
Discussion
Prematurity is characterized by a chronic hyperinflammatory which is not the same as the inflammatory response in adulthood. Even in the absence of disease, the inflammatory reaction is more pronounced in preterm infants with markedly elevated concentrations of proinflammatory cytokines. It is partially due to an increase in production of proinflamma-tory mediators, but it is also due to the lack of negative regulators [2]. Determining the concentration of IL-6 in the blood, as the earliest (apart from TNF-a) marker of inflammation during sepsis, allows for a quick recognition of the threat and the initiation of therapeutic intervention, thus limiting the inflammatory reaction.
The crucial issue during the diagnosis of sepsis was to obtain the optimal cutt-off values for blood IL-6 concentration. Recently, Kung E et al [14] published a retrospective analysis a group of 1695 new-borns consisting of preterm infants born before the 32nd week of gestation. The group of analysed patients included both healthy preterm neonates and new-borns with EOS (early onset sepsis) confirmed by positive culture results. Due to physiological changes in IL-6 concentrations in the first few days after birth, cut-off values were determined separately for the first day of life, then for the period between days 2-7and after day 7. They were as follows: 80 pg/mL, 40 pg/mL and 30 pg/mL. In turn, Tessema et al. [15] based on the results of their own research, they indicated a concentration of 313.5 pg/mL as the cutt-off value allowing to diagnose both EOS and LOS. In contrast, Ebenebe et al. [16] reported that a cutt-off value for IL-6 blood concentration during the first 72 hours of life was 40 pg/mL. The importance of determining IL-6 concentration in the process of EOS and LOS diagnosis has been indicated by all authors who have mentioned publications.
The reduction of IL-6 levels in the blood in sepsis is possible by using pentoxifylline, the effect of which, consisting in the inhibition of the synthesis and release of this cytokine, has been described in many publications [12,17,18, 20]. This is particularly important in the context of limiting the damaging effects of the inflammatory process on the immature central nervous system of the preterm infant. In our first prospective, randomized, doubleblind, placebo-controlled study on the effectiveness and safety of PTX in the treatment of neonatal sepsis, published in 1999, we suggested pentoxifylline infusion in a dose of 5 mg per kg per hour given for 6 hours [12]. Therapy was usually continued for 5-6 consecutive days. During the period between 1994 - 1999, there were no possibilities for routine deter-mining the concentration of IL-6 in blood, and for adjusting the dosage of the drug and the length of infusion of pentoxifylline, according to the values of serum cytokine concentrations. During the last several years of testing IL-6 blood concentration in the process of sepsis diagnosis, authors optimized the scheme of pentoxifylline use, determining both the dose of the drug per kg/hour and the length of intravenous infusion in depending on the concentration of this cytokine in the serum [19].
We described a case of a preterm infant who developed LOS relatively early after birth. The value of serum IL-6 concentration, found in the first assay, was 29.919 pg/ml and significantly exceeded the cutt-values for sepsis diagnosis, recently published by several authors. Surprisingly, the immediate introduction of PTX infusion at a dose of 5 mg/kg/h, did not inhibited or even slow down the further increase in serum IL-6 concentration. Only then when a drug dose was increased by two-fold (10 mg/kg/hour) the serum IL-6 concentration showed a tendency to decrease and reached values below 1000 pg/m during the next 5 consecutive days. It is widely accepted that proinflammatory cytokines stimulate the coagulation cascade which may lead to thrombosis, perfusion disorders, organ dysfunction and eventually cause hemorrhagic diathesis and severe bleeding. All these symptoms were pre-sent in our patient during the first few days of the disease. The most important factor for both the survival and the neurological status in the future of our patient was a significant inflammatory response in the brain. It was caused both by a significantly increased serum IL-6 concentration during sepsis and the presence of extravasated blood which released a considerable amount of iron. It is known that iron, which is necessary for many important processes in an organism, can stimulate the production of free radicals when in excess. The inflammatory reaction becomes more intense, and the injury of cells and tissues increases. It may lead to death of the cell during the process of ferroptosis. During severe sepsis, the episodes of ischaemia reperfusion may occur relatively frequently and apart from hypoxia, they can stimulate the process of ferroptosis. Recently, the results of the experimental study provided evidence for protection by PTX against the ischemia-reperfusion injury through ferroptosis regulation [10].
Recently, Haggar and co-authors showed that PTX has neuroprotective effects in adults. Twelve weeks of PTX administration at a dose of 800 mg/day caused a significant increase in blood concentration of the brain derived neutrophic factor (BNDF) [20]. BNDF plays a crucial role for the development of the peripheral and central nervous system. It was found in the experimental studies that PTX may stimulate neurogenesis processes and pre-vent neuronal degeneration, especially in the hippocampus. Primarily, the increase in cAMP levels as well as the reduction of proinflammatory cytokines concentrations, likely played an important role in promoting neurogenesis by PTX [11]. Moreover, Zheng and co-authors [7], based on the results obtained in the experimental study, suggested an important role of PTX in modulating of microglial associated phagocytosis and the protective effects against white matter injury were observed after episodes of hypoxia. It is also known that significantly increased proinflammatory cytokines concentrations due to sepsis may impair pre-oligodendrocytes, which ultimately causes white matter injury and myelinization [21]. Furthermore, recently Ruiz-Perera and co-authors, showed using of a model of human neuronal stem cells, that PTX shifted stem cell differentiation towards oligodendroglial cells [22]. Experimental and clinical research should be conducted to determine if it can improve the impaired process of myelinization.
We cautiously suggest that a lack of major brain damages and the optimistic results of neurological examinations, observed both before the discharge and on the 3rd month after release patients from hospital, were caused by the use of PTX during the period of significantly increased inflammatory reactions occurring in the LOS. However, it should be under-lined that the dosage of drug and the length of the infusion administered to this patient, differed markedly from that described in our previous publication in 1999.
Finally, basing on the results presented above, authors indicate that the scheme of pentoxifylline use, based on the serum IL-6 concentration should be considered during therapy for different clinical conditions, when a significant inflammatory response is the most important reason for the infant disease.
Author contributions: Agnieszka Ochoda-Mazur and Ryszard Lauterbach: writing – review and editing, supervision. Dorota Pawlik and Małgorzata Jabłońska: collecting the information of in-fant. All authors contributed to the article and approved the submitted version.
Conflict of interest: The authors declare that the case presentation was conducted in the absence of any commercial or financial relationship that could be construed as a potential conflict of inter-est.
References
- Kashlan F, Sumulian J, Shen-Schwarz S, Anwar M, Hiatt M, et al (2000) “Umbilical vein interleukin 6 and tumour necrosis factor alpha plasma concentration in very preterm infant”. Pedi-atr Infect Dis J 19:238-243.
- Martin CR. (2016) Chapter: “Infection disease and immunology”. In Year Book of Neo-natal and Perinatal Medicine. Elsevier Inc 94.
- Kurul S, Simons S, Ramakers C, De Rijke Y, Kornelisse RF, et al (2021) “Association of inflammatory biomarkers with subsequent clinical course in suspected late onset sepsis in preterm neo-nates”. Critical Care 12:1-10.
- Eichberger J, Resh E, Resh B. (2024) “Reliability of IL-6 alone and in combination for diagnosis of late onset sepsis: a systematic review”. Children 11:486.
- Cappelletti M, Ferrazzi E, Mavilio D, Bella SD, Divanovic S (2016) “Inflammation and preterm birth”. J Leukoc Biol. 99:67-78.
- Giordano V, Stummer S, Lindtner C, Fuiko R, Berger A, et al (2022) “Neonatal sepsis is associated with behavioral abnormalities in very low birthweight infants at preschool age”. Front Pediatr 10: 906379.
- Zheng L, Junqiu J, Chen Y, Liu R, Cao R, et al (2022) “Pentoxifylline alleviates ischemic white matter injury through up-regulating Mertkmediated myelin clearance.” J Neuroinflammation 19:1-15.
- Siegel A, Rodrigues N, Nasri F, Wilkialis L, Lipsitz O, et al (2021) “Novel therapeutic targets in mood disor-ders: Pentoxifylline (PTX) as a candidate treatment”. Prog Neuropsychopharma-col Biol Psychiatry 104; 110032.
- Merza Mohammad T, Salman D, Jaafar H. (2024) “Pentoxifylline as a novel add-on ther-apy for major depressive disorder in adult patients: a randomized, double-blind, placebo-controlled trial.” Pharmacopsychiatry.4:205-214.
- Li P, Chen J, Ge S, SunM, Lu JD, et al (2024) “Pentoxifylline protects against cerebral ischaemia-reperfusion injury through ferroptosis regulation via the Nrf2/SLC7A11/GPX4 signalling pathway”. Eur J Pharmacol 15:967:176402.
- Halis H, Bitiktas S, Bastug O, Tan B, Kavraal S, et al (2019) Differential effects of pentoxifylline on learning and memory impairment induced by hypoxic-ischemic brain injury in rats”. Clin Psychopharmacol Neurosci 17:388-399.
- Lauterbach R, Pawlik D, Kowalczyk D, Ksycinski W, Helwich E, et. Al (1999) Effect of the immunomodulating agent, pentoxifylline, in the treatment of sepsis in prematurely delivered infants: a randomized, placebo-controlled double-blind trial”. Crit Care Med 27:807-814.
- Lauterbach R, Wilk B, Bocheńska A, Hurkala J, Radziszewska R (2016) Non-activated protein C in the treat-ment of neonatal sepsis: a retrospective analysis of outcome”. J Pediatr Infect Dis 35:967-971.
- Kung E, Unterasinger L, Waldhor T, Berger A, Wisgrill L (2023) “Cutt-off values of serum interleukin 6 for culture confirmed sepsis in neonates.” Pediatr Res 93: 1969-1974.
- Tessema B, Lippmann N, Willenberg A, Knupfer M, Sack U, et al (2020) “The diagnostic performance of in-terleukin-6 and C reactive protein for early identification of neonatal sepsis. Di-agnostics (Basel) 10: E978.
- Ebenebe C, Hesse F, Blohm M, Jung R, Kunzmann S, et al (2021) “Diagnostic accuracy of inerleukin-6 for early onset sepsis in preterm neonates.” J Matern Fetal Neonatal Med 34:253-258.
- Harris E, Schulzke S, Patole S. (2010) “Pentoxifylline in preterm neonates: a systematic review”. Paediatr Drugs 12:301-311.
- Wong F, Rath C, Gowda B, Patole S (2024) “Role of pentoxifylline in neonatal hypoxic Is-chemic encephalopathy: a systematic review of animal studies.” Lab animal re-search 40:4.
- Lauterbach R, Pawlik D. (2023) “May pentoxifylline protect immature brain against dis-orders induced by inflammatory response in neonatal sepsis?” J Neonatol Pediatr Care 103.
- El-Hagar S, Eissa M, Mostafa T, EI-Attar KS, Abdallah MS (2018) “The phosphodiesterase inhibitor pentoxi-fylline as a novel adjunct to antidepressant in major depressive disorder patients: a proof-of concept, randomized, double blind, placebo-controlled trial.” Psychother Psychosom 87:331-339.
- Hagberg H, Mallard C, Ferriero D, Vannucci SJ, Levison SW, et al (2015) “The role of inflammation in perinatal brain injury” Nat Rev Neurol 11:192-208.
- Ruiz-Perera M, Greiner J, Kaltschmidt C, Kaltschmidt B (2020) “A matter of choice: inhibition of c-Rel shifts neuronal to oligodendroglial fate in human stem cells”. Cells 4:1037.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.