Cardiovascular Risk Factor Control in Patients with Type 2 Diabetes in Uruguay: Are we Meeting the Targets?
by Maria M Pineyro*, Vanessa Maffoni, Leonardo Diaz
Unidad Académica de Endocrinología y Metabolismo, Hospital de Clínicas “Dr. Manuel Quíntela”, Facultad de Medicina, Universidad de la República, Montevideo, Uruguay.
*Corresponding author: Maria M Pineyro Unidad Académica de Endocrinología y Metabolismo, Hospital de Clínicas “Dr. Manuel Quíntela”, Facultad de Medicina, Universidad de la República, Montevideo, Uruguay.
Received Date: 03 November 2025
Accepted Date: 16 November 2025
Published Date: 21 November 2025
Citation: Pineyro MM, Maffoni V, Diaz L (2025) Cardiovascular Risk Factor Control in Patients with Type 2 Diabetes in Uruguay: Are we Meeting the Targets? J Diabetes Treat 10: 10150. https://doi.org/10.29011/2574-7568.010150
Abstract
Background: Atherosclerotic Cardiovascular Disease (ASCVD) remains the leading cause of morbidity and mortality in Type 2 Diabetes (T2D). This study assesed the prevalence and control of Cardiovascular Risk Factors (CVRFs), and pharmacologic interventions in patients with T2D receiving care at the Endocrinology and Metabolism department of the Hospital de Clínicas. Methods: Descriptive, observational, cross-sectional study of 78 T2D patients between July and December 2019.
Results: Most participants were women (70.5%), with a mean age of 57 years and diabetes duration of 9.6 years. Obesity and hypertension were present in 60% and 68%, respectively. Smoking was reported in 13%, more frequently among men. Macrovascular complications were observed in 23.1%, and markers of renal damage in approximately 20% of patients. A cardiovascular risk score >20% was recorded in 11.1%, exclusively among men. HbA1c targets were achieved in 37.7% of patients without end-organ damage and in 50% with established disease. Only half met lipid goals. Statins were appropriately prescribed in 65.6% without and 75% with cardiovascular disease, the latter also receiving antiplatelets. Notably, only 5% achieved simultaneous control of all major CVRFs.
Conclusions: Most patients presented with obesity, suboptimal glycemic control, and dyslipidemia. Alarmingly, only a small proportion achieved comprehensive CVRF control, which is critical given the strong association between T2D and cardiovascular morbidity and mortality. These findings underscore the urgent need for a structured and integrative care model that combines intensive pharmacotherapy with individualized strategies to optimize CVRF management in patients with T2D.
Keywords: Type 2 Diabetes; Metabolic Control; Cardiovascular Morbidity and Mortality; Cardiovascular Risk Factors
Introduction
Type 2 Diabetes Mellitus (T2D) is a leading cause of global morbidity and mortality. Its prevalence continues to rise, driven by the ongoing epidemic of obesity, sedentary lifestyles, an aging population, and improved survival due to advances in treatment strategies over recent decades. In Uruguay, the reported prevalence of diabetes is approximately 8.0%, ranging from 6.0% to 8.0% [1,2].
Cardiovascular disease is the primary cause of morbidity and mortality among individuals with diabetes, with a 2- to 4-fold increased risk of death from cardiovascular causes compared to non-diabetic individuals. The main contributors to this poor prognosis are Atherosclerotic Cardiovascular Diseases (ASCVD), encompassing coronary, cerebrovascular, and peripheral arterial disease [3,4].
This population also bears a heavy burden of coexisting Cardiovascular Risk Factors (CVRFs), including hypertension, dyslipidemia, obesity, smoking, albuminuria, and Chronic Kidney Disease (CKD), all of which further compound their cardiovascular risk [5].
Multiple international studies have demonstrated that intensive and simultaneous management of these CVRFs is associated with a significant reduction in major cardiovascular events and mortality. Notably, the Steno-2 study showed that multifactorial intervention in T2D patients with microalbuminuria led to meaningful reductions in cardiovascular events and mortality, with long-term gains in cardiovascular disease-free survival [6-8].
More recently, Rawshani et al. analyzed a cohort of 271,174 individuals with T2D compared to 1,355,870 without diabetes. Their findings revealed that patients who maintained the five key CVRFs (HbA1c, LDL-C, blood pressure, smoking status, and albuminuria) within guideline-recommended targets exhibited rates of mortality, myocardial infarction, and stroke comparable to the general population [9].
However, a substantial gap persists between evidence-based recommendations and real-world clinical practice. Several studies have shown that fewer than half of patients with T2D achieve recommended targets for HbA1c, blood pressure, and lipid levels [10]. A recent meta-analysis of 24 studies including 369,251 patients from 20 countries found that the proportion of patients meeting all therapeutic goals remains strikingly low [11].
Furthermore, the presence of CKD-defined by an estimated glomerular filtration rate <60 mL/min/1.73 m² and/or albuminuriasubstantially increases residual cardiovascular risk. For this subgroup, clinical guidelines recommend moderate-intensity statin therapy, even when LDL-C levels are within normal range [12].
In Uruguay, there is a lack of current data on the frequency and degree of CVRF control in patients with T2D receiving routine care. In this context, the aim of this study was to describe the prevalence and control of CVRFs in a cohort of T2D patients followed at the Endocrinology and Metabolism Clinic of the Hospital de Clínicas.
Methodology
A retrospective cross-sectional study was conducted using the medical records of 78 patients with type 2 diabetes mellitus (T2DM) treated in the outpatient Endocrinology Unit of the Hospital de Clinicas, Montevideo, Uruguay. The study period spanned from July to December of 2019. Inclusion criteria: Patients aged 18 years or older, with diagnosis of T2DM for at least one year. In addition, availability of at least one clinical visit and the following laboratory tests within the study period: HbA1c, lipid profile, and renal function parameters. Exclusion criteria included pregnancy, older adults (>65 years) and other type of diabetes. We collected demographic, anthropometric, and clinical data (including blood pressure, BMI, and smoking status), as well as the presence of macrovascular (cardiovascular events, stroke, peripheral arterial disease) and microvascular (nephropathy) complications. Laboratory data included fasting glucose, HbA1c, lipid profile, creatinine, eGFR, albuminuria, and blood pressure levels. The use of pharmacologic treatment for glycemic, lipid, and blood pressure control was also documented. Global cardiovascular risk was estimated using the American Heart Association’s ASCVD Risk Estimator Plus tool (http://tools.acc.org/ASCVDRisk-Estimator-Plus). Achievement of guideline-based control of major cardiovascular risk factors (CVRFs) was assessed according to the 2021 ADA Standards of Care [13]. Metabolic control was defined as HbA1c <7% in most adults, or <8% in those with severe comorbidities or increased hypoglycemia risk. HbA1c values obtained within 6 months prior to the last clinical visit were considered valid. In individuals with low cardiovascular risk (10-year ASCVD risk <15%), the target blood pressure was <140/90 mmHg(10). Lipid targets were defined as follows: LDL <70 mg/dL for patients in secondary prevention or with ASCVD risk >20%, for whom high-intensity statin therapy (atorvastatin 40–80 mg/day or rosuvastatin 20–40 mg/day) is indicated.
Adults ≥40 years without established ASCVD and with 10-year risk <20% were recommended moderate-intensity statins (atorvastatin 10–20 mg/day or rosuvastatin 5–10 mg/day), with a goal LDL <100 mg/dL. In patients <40 years without ASCVD and risk <20%, statins were not indicated provided the target LDL <100 mg/dL was met. A fasting triglyceride goal <150 mg/dL was applied for all participants.
Other CVRFs recorded included: history of smoking (as documented in the medical record), obesity (BMI ≥30 kg/m²), albuminuria >30 mg/g within the previous year, and estimated GFR <60 mL/min/1.73 m² (CKD-EPI equation). Statistical analyses were conducted using R software (version 4.0.4). Descriptive statistics-including means, medians, standard deviations, and proportions-were calculated as appropriate. Inferential analyses were performed based on the type of variable: Student’s t-test was used for comparisons of means, while Chi-square or Fisher’s exact test was applied to assess associations between categorical variables
Results
A total of 78 patients with a diagnosis of Type 2 Diabetes Mellitus (T2DM) were identified from the outpatient records of the Endocrinology and Metabolism Clinic. The majority were female (70.5%), with a mean age of 57 years. The average duration of diabetes was 9.6 years. The main clinical and demographic characteristics of the study population are summarized in (Table 1). Notably, there was a high prevalence of arterial hypertension (68%) and active smoking (13%). Additionally, 11.5% of patients had a documented history of Acute Myocardial Infarction (MI).
|
Total n= 78 |
Women n= 55 |
Men n= 23 |
No data (W/M) |
P |
|
|
Age (years) |
57 ± 6 |
57 ± 6 |
57 ± 7 |
- |
0.955 |
|
Diabetes duration (years) |
9.6 ± 8.6 |
7.6 ± 8.0 |
10.5 ± 8.8 |
(2/0) |
0.164 |
|
Smoking |
10/77 (13.0%) |
3/55 (5.5%) |
7/22 (31.8%) |
(0/1) |
0.002 |
|
IMC ≥ 30 Kg/m2 |
47/75 (62.7%) |
34/53 (64.2%) |
13/22 (59.1%) |
(2/1) |
0.682 |
|
Hipertension |
53/78 (68.0%) |
39/55 (70.9%) |
14/23 (60.9%) |
- |
0,384 |
|
CV disease |
18/78(23.1%) |
10/55 (18.1%) |
7/23 (30.4%) |
||
|
MI |
9/78 (11.5%) |
4/55 (7.3%) |
5/23 (21.7%) |
- |
0.069 |
|
CVA |
5/78 (6.4%) |
4/55 (7.3%) |
1/23 (4.4%) |
- |
0.631 |
|
PAD |
3/78 (3.8%) |
2/55 (3.6%) |
1/23 (4.3%) |
- |
0.999 |
|
GFR < 60 ml/min |
15/73 (20.5%) |
10/50 (20.0%) |
5/23 (21.7%) |
(5/0) |
0.865 |
|
Albuminuria |
7/36 (19.4%) |
6/27 (22.2%) |
1/9 (11.1%) |
(28/14) |
0.465 |
|
ASCVD risk > 20% |
4/36 (11.1%) |
0/25 (0%) |
4/11 (36.4%) |
(16/5) |
0.001 |
|
Family history of premature CVD |
1/78 (1.3%) |
1/55 (1.8%) |
0/23 (0%) |
- |
0.516 |
|
*CVA: Cerebrovascular accident; PAD: Peripheral artery disease |
|||||
Table 1. Demographic characteristics of the patients in the study.
A significantly higher prevalence of smoking was observed among male participants compared to their female counterparts (31.8% vs. 5.5%, p = 0.002). In terms of nutritional status, obesity affected approximately two-thirds of the study population. Although a greater proportion of women were classified as obese compared to men (64.2% vs. 59.1%), this difference was not statistically significant (p = 0.682) (Figure 1).
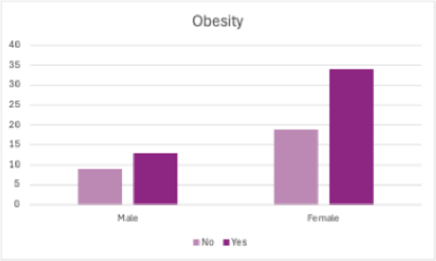
Figure 1: Obesity and gender.
Regarding overall cardiovascular risk, only male patients presented a 10-year cardiovascular disease (CVD) risk greater than 20%, with approximately one-third of them exceeding this threshold. In contrast, only one patient (1.3%) reported a family history of premature CVD.
Among participants with available renal function data, 20.5% had an estimated glomerular filtration rate (eGFR) below 60 ml/ min/1.73 m². No statistically significant association was found between HbA1c levels and the presence of reduced renal function. In the subgroup of patients over 50 years old with renal impairment (n=67), 90% were receiving statin therapy at either moderate or high intensity.
Macrovascular complications—including myocardial infarction, stroke, and cerebrovascular occlusive conditions—were present in approximately one-quarter of the cohort, with a higher frequency observed among men compared to women (26.1% vs. 18.2%, p = 0.63). However, no association was identified between HbA1c levels and the occurrence of macrovascular complications. Regarding lipid control, only 50% of the patients achieved target levels for both low-density lipoprotein cholesterol (LDL-C) and triglycerides (Table 2).
|
Total n= 78 |
|
|
LDL< 100 mg/dl |
24/49 (49.0%) |
|
LDL < 70 mg/dl |
7/33 (21.2%) |
|
TG < 150 mg/dl |
30/60 (50.0%) |
|
Hba1c < 7% |
23/61 (37.7%) |
|
Hba1c < 8% |
3/6 (50.0%) |
|
PA < 140/90 |
56/76 (73.7%) |
Table 2: Control of CVD risk factors.
A significantly lower proportion of patients with obesity achieved the target triglyceride (TGL) level of <150 mg/dL compared to their non-obese counterparts (29.8% vs. 53.6%; p = 0.02).
Among patients without terminal illness, one-third achieved an HbA1c level <7%. In contrast, 50% of those with advanced disease reached the recommended target of HbA1c <8%. Regarding blood pressure (BP) control, 68% of the study population had a diagnosis of hypertension, of whom 64.1% maintained BP values within the target range (<140/90 mmHg). Notably, 86.8% of hypertensive patients were receiving treatment with Angiotensin-Converting Enzyme Inhibitors (ACE inhibitors) or Angiotensin Receptor Blockers (ARBs), and 67.4% successfully met the BP target.
In the subgroup without macrovascular disease, 33.8% of patients had an LDL cholesterol level <100 mg/dL, while another 33.8% exceeded this threshold, and LDL values were unavailable for 29.3% of the group.
Among patients with established macrovascular disease, only 25% met the stricter LDL target of <70 mg/dL, whereas nearly half of them failed to achieve this goal (Figure 2).
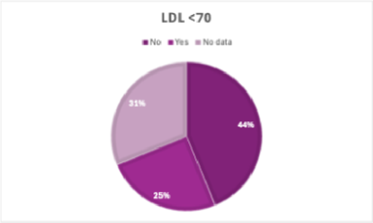
Figure 2: LDL target in patients with macrovascular complications.
With regard to pharmacological management, approximately 60% of patients were receiving treatment with angiotensinconverting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs), as well as statins at moderate doses. However, only a minority of the cohort were prescribed high-intensity statin therapy (Table 3).
|
ACEi/ARB |
46/78 (59.0%) |
|
Statins moderate dose |
45/78 (57.7%) |
|
Statin high dose |
16/78 (20.5%) |
|
Aspirin |
14/78 (17.9%) |
Table 3: Frequency of use of medication for cardiovascular risk factors.
Among patients over 40 years of age without macrovascular disease (n = 61), 65.6% were receiving statin therapy. Intermediate doses of atorvastatin predominated (61%), while high-intensity statin use was infrequent (5%). In contrast, among patients with established macroangiopathy, 75% were receiving high-dose statin therapy and aspirin. Overall, suboptimal control of cardiovascular risk factors was observed. Although blood pressure targets (<140/90 mmHg) were achieved in 72% of hypertensive patients, fewer than 40% met the recommended goals for glycemic control (HbA1c), LDL cholesterol, triglyceride levels, and body mass index. Notably, comprehensive control of all major cardiovascular risk factors was achieved in only 5% of the cohort, with no statistically significant differences between sexes (Table 3).
|
All patients |
Female |
Male |
p |
|
|
(n = 78) |
(n = 55) |
(n = 23) |
||
|
Hba1c < 7-8% |
26 (33%) |
19 (35%) |
7 (30%) |
0.726 |
|
LDL < 100 mg/dl (without MVC) |
21 (34%) (n = 62) |
14 (31%) (n = 45) |
7 (41%) (n = 17) |
0.453 |
|
LDL < 70 mg/dl with MVC) |
4 (25%) (n = 16) |
2 (20%) (n = 10) |
2 (33%) (n = 6) |
0.549 |
|
TG < 150 mg/dl |
30 (38%) |
22 (40%) |
8 (35%) |
0.667 |
|
BP < 140/90 mmHg |
56 (72%) |
39 (71%) |
17 (74%) |
0.787 |
|
BMI < 30 kg/m2 |
28 (36%) |
19 (35%) |
9 (39%) |
0.704 |
|
0 target met |
10 (13%) |
7 (13%) |
3 (13%) |
0.968 |
|
1 target met |
16 (21%) |
12 (22%) |
4 (17%) |
0.66 |
|
2 targets met |
26 (33%) |
17 (31%) |
9 (39%) |
0.484 |
|
3 targets met |
11 (14%) |
9 (16%) |
2 (9%) |
0.373 |
|
4 targets met |
11 (14%) |
8 (14%) |
3 (13%) |
0.865 |
|
5 targets met |
4 (5%) |
2 (4%) |
2 (9%) |
0.358 |
|
MVC: macrovascular complications |
||||
Table 3: Control of modifiable cardiovascular risk factors.
Discussion
This study highlights the suboptimal management of Cardiovascular Risk Factors (CVRFs) in a cohort of 78 patients with type 2 diabetes, despite the well-established elevated cardiovascular risk associated with the disease. Type 2 diabetes is widely recognized as a coronary heart disease risk equivalent, as stated by the U.S. National Cholesterol Education Program (NCEP) and the European guidelines [14,15]. Nonetheless, the achievement of therapeutic goals remains insufficient across several critical domains of cardiovascular risk management. Previous research has demonstrated that patients with type 2 diabetes and no prior Acute Myocardial Infarction (AMI) exhibit a similar risk of cardiovascular events and cardiovascular mortality to that of non-diabetic individuals with prior AMI [16]. The Framingham Heart Study further confirmed this risk, showing that diabetes doubles the risk of cardiovascular disease (CVD) in men and triples it in women, even after adjustment for other risk factors [17]. A meta-analysis including over 530,000 individuals across 102 studies corroborated these findings, reporting a pooled hazard ratio (HR) of 2.0 (95% CI: 1.8-2.2) for coronary heart disease in patients with T2D, with significantly higher rates of non-fatal myocardial infarction and cardiovascular mortality [18]. The overall cardiovascular risk in this population is determined by both the number of risk factors and the degree to which treatment aligns with evidence-based guidelines. In our cohort, the prevalence of CVRFs was notably high: 60.3% of patients were obese (BMI ≥30 kg/m²), a key contributor to atherogenesis [19]. Nearly 70% had hypertension, and about one-fifth exhibited reduced renal function (GFR <60 mL/min/1.73 m²). Additionally, 19.4% had at least one episode of elevated albuminuria, indicating early nephropathy. Interestingly, the prevalence of smoking was relatively low, a finding that may reflect the success of public health tobacco control strategies in Uruguay. This is particularly evident when compared to the 25.9% prevalence reported in the general population by the latest ENFRENT survey [20]. The 10-year cardiovascular risk, estimated using the AHA Risk Estimator Plus, exceeded the 20% threshold only among men in the sample, aligning with findings from original U.S. cohorts. However, studies such as ADVANCEON suggest that, with a similar burden of risk factors, women with T2D may have a higher relative risk of AMI, highlighting the need for gender-sensitive approaches to risk stratification [21].
Lipid control was suboptimal. Most patients had elevated LDL levels, and triglyceride levels were poorly controlled—especially in obese individuals (29.8%). This pattern is consistent with atherogenic dyslipidemia commonly seen in T2D, characterized by hypertriglyceridemia, low HDL cholesterol, and a predominance of small dense LDL particles. According to ADA 2021 guidelines, all patients over 40 years of age with diabetes should receive at least moderate-intensity statins, regardless of cardiovascular disease status [10]. In our sample, 65.6% of patients without macrovascular disease were receiving statin therapy, predominantly at intermediate doses, with limited use of high-intensity statins. In contrast, 75% of individuals with established macrovascular disease were prescribed high-dose statins and aspirin, in alignment with secondary prevention guidelines.
Despite antihypertensive treatment in 86.8% of hypertensive patients, 36% did not reach the target blood pressure of <140/90 mmHg. This therapeutic gap is clinically meaningful: the UKPDS demonstrated that each 10 mmHg reduction in diastolic blood pressure reduces the risk of diabetes-related complications, including AMI, by 12% [22].
Moreover, the incidence of both fatal and non-fatal AMI declined from 33.1 to 18.4 events per 100,000 person-years as systolic blood pressure decreased from ≥160 mmHg to <120 mmHg [23].
Only one-third of patients without terminal illness and 50% of those with terminal illness achieved glycemic targets (HbA1c), underscoring the persistent challenge of achieving optimal metabolic control.
While the association between glycemic control and macrovascular events remains debated, several large trials have shown modest but statistically significant cardiovascular benefit from intensive glycemic control. A meta-analysis of the ACCORD, ADVANCE, UKPDS, and VADT trials-including 27,049 participants and 2,370 major cardiovascular events-demonstrated a 9% relative risk reduction in cardiovascular events and a 15% reduction in myocardial infarction with intensive glycemic control. In patients without prior macrovascular disease, the reduction reached 16% [24].
Microvascular complications such as albuminuria and CKD were present in ~20% of the sample and are strongly associated with increased cardiovascular risk, as demonstrated in prior literature [25].
The cornerstone of cardiovascular prevention in T2D remains multifactorial intervention: glycemic control, smoking cessation, blood pressure regulation, and lipid management. Studies like VADT have shown that combined control of HbA1c and LDL yields greater benefit than managing either in isolation. Similarly, ADVANCE and BARI-2D confirmed that multifactorial interventions-including glycemia, blood pressure, lipids, and aspirin-significantly reduce cardiovascular morbidity and mortality [18,26,27].
A particularly striking finding in our study was that only 5% of patients achieved simultaneous control of all major CVRFs, and even fewer achieved combined control of two or three risk factors. No significant sex-based differences were observed in this outcome. This highlights a critical gap in comprehensive risk management and supports the urgent need for systematized, protocol-driven interventions aimed at improving multifactorial risk factor control. The principal limitations of this study include the relatively small sample size and the absence of a computerized clinical record system. These factors may have restricted a more comprehensive identification of eligible patients and hindered the systematic collection of relevant clinical parameters.
Conclusions
In this cohort of patients with type 2 diabetes mellitus, a high prevalence of obesity and suboptimal metabolic control was observed. Fewer than half of the participants met therapeutic targets for glycemic and lipid parameters. Moreover, simultaneous achievement of control across multiple Cardiovascular Risk Factors (CVRFs) was markedly low, despite robust evidence linking comprehensive risk factor management to improved cardiovascular outcomes.
These findings underscore the urgent need for the implementation of an integrated, multifactorial approach to diabetes care. Clinical strategies should emphasize the intensification of treatment based on standardized, evidence-based protocols. Achieving sustained and simultaneous control of key CVRFs must be considered a priority in the management of patients with type 2 diabetes, with the ultimate goal of reducing macrovascular complications and enhancing long-term health outcomes.
Acknowledgments
The data in this manuscript have been presented as an abstract at the X Congresss Uruguayan of Endocrinology, Diabetes and Metabolism, Anales de la Facultad de Medicina Editorial C. X CONGRESO URUGUAYO DE ENDOCRINOLOGÍA, DIABETES Y METABOLISMO: II ENCUENTRO DE ENDOCRINOLOGIA Y DIABETES DEL CONO SUR. An Facultad Med (Univ Repúb Urug) [Internet]. 26 de abril de 2023 [citado 29 de octubre de 2025];10. Disponible en: https://revistas. udelar.edu.uy/OJS/index.php/anfamed/article/view/1168.
Conflict of Interest: The authors declare no conflicts of interest in relation to this study.
Funding: None.
Data Availability: The primary data used in this study are available from the authors upon reasonable request, without undue restrictions.
Ethical Guidelines: The study protocol was reviewed and approved by the Ethics Committee of the Hospital de Clínicas.
References
- Ferrero RG, V (2005) Encuesta prevalencia de diabetes en el Uruguay. Arch Med Int 27: 7-12.
- Sandoya E (2016) Diabetes and cardiovascular disease in Uruguay 31: 505-514.
- Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, et al. (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375: 2215-2222.
- Rawshani A, Rawshani A, Franzén S, Eliasson B, Svensson AM, et al. (2017) Mortality and Cardiovascular Disease in Type 1 and Type 2 Diabetes. N Engl J Med 376: 1407-1018.
- Uusitupa MI, Niskanen LK, Siitonen O, Voutilainen E, Pyörälä K (1993) Ten-year cardiovascular mortality in relation to risk factors and abnormalities in lipoprotein composition in type 2 (non-insulindependent) diabetic and non-diabetic subjects. Diabetologia 36: 11751184.
- Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O (2003) Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med 348: 383-393.
- Gaede P, Lund-Andersen H, Parving HH, Pedersen O (2008) Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 358: 580-591.
- Gæde P, Oellgaard J, Carstensen B, Rossing P, Lund-Andersen H, et al. (2016) Years of life gained by multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: 21 years follow-up on the Steno-2 randomised trial. Diabetologia 59: 2298-2307.
- Rawshani A, Rawshani A, Franzén S, Sattar N, Eliasson B, et al. (2018) Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med 379: 633-644.
- (2024) Cardiovascular Disease and Risk Management: Standards of Care in Diabetes-2024. Diabetes Care 47: S179-s218.
- Khunti K, Ceriello A, Cos X, De Block C (2018) Achievement of guideline targets for blood pressure, lipid, and glycaemic control in type 2 diabetes: A meta-analysis. Diabetes Res Clin Pract 137: 137148.
- Chen TK, Knicely DH, Grams ME (2019) Chronic Kidney Disease Diagnosis and Management: A Review. Jama 322: 1294-1304.
- (2021) 6. Glycemic Targets: Standards of Medical Care in Diabetes-2021. Diabetes Care 44: S73-s84.
- (2002) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 106: 3143-3421.
- De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, et al. (2003) European guidelines on cardiovascular disease prevention in clinical practice: third joint task force of European and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of eight societies and by invited experts). Eur J Cardiovasc Prev Rehabil 10: S1-s10.
- Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M (1998) Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 339: 229-234.
- Kannel WB, McGee DL (1979) Diabetes and cardiovascular risk factors: the Framingham study. Circulation 59: 8-13.
- Bittner V, Bertolet M, Barraza Felix R, Farkouh ME, Goldberg S, et al. (2015) Comprehensive Cardiovascular Risk Factor Control Improves Survival: The BARI 2D Trial. J Am Coll Cardiol 66: 765-773.
- Lavie CJ, Milani RV, Ventura HO (2009) Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol 53: 1925-1932.
- (2013) Ministerio de Salud Pública. 2° Encuesta nacional de factores de riesgo de enfermedades no transmisibles.
- Zoungas S, Chalmers J, Neal B, Billot L, Li Q, et al. (2014) Follow-up of blood-pressure lowering and glucose control in type 2 diabetes. N Engl J Med 371: 1392-1406.
- (1998) Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 352: 837-853.
- Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, et al. (2000) Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. Bmj 321: 412-419.
- Turnbull FM, Abraira C, Anderson RJ, Byington RP, Chalmers JP, et al. (2009) Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia 52: 2288-2298.
- Fox CS, Matsushita K, Woodward M, Bilo HJ, Chalmers J, et al. (2012) Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet 380: 1662-1673.
- Zoungas S, de Galan BE, Ninomiya T, Grobbee D, Hamet P, et al. (2009) Combined effects of routine blood pressure lowering and intensive glucose control on macrovascular and microvascular outcomes in patients with type 2 diabetes: New results from the ADVANCE trial. Diabetes Care 32: 2068-2074.
- Tancredi M, Rosengren A, Svensson AM, Kosiborod M, Pivodic A, et al. (2015) Excess Mortality among Persons with Type 2 Diabetes. N Engl J Med 373: 1720-1732.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.