Awake Robot-Assisted Laparoscopic Prostatectomy under Neuraxial Anaesthesia and Intermediate Cervical Plexus Block
by Lorenzo Forasassi1, Francesco Marrone2*, Roberto Starnari3, Carmine Pullano4
1Senior Consultant, Unit of Anaesthesia, Villa Donatello Clinic, Florence, Italy
2Consultant, Unit of Anaesthesia and Intensive Care, Santo Spirito Hospital, Rome, Italy
3Senior Consultant, Department of Anesthesiology, IRCSS-INRCA, Ancona, Italy
4Senior Consultant, Unit of Anaesthesia, Villa Pia Clinic, Rome, Italy
*Corresponding author: Francesco Marrone, Consultant, Unit of Anaesthesia and Intensive Care, Santo Spirito Hospital, Rome, Italy
Received Date: 24 October 2024
Accepted Date: 28 October 2024
Published Date: 30 October 2024
Citation: Forasassi L, Marrone F, Starnari R, Pullano C (2024) Awake Robot-Assisted Laparoscopic Prostatectomy under Neuraxial Anaesthesia and Intermediate Cervical Plexus Block. Ann Case Report. 9: 2039. https://doi.org/10.29011/2574-7754.102039
Abstract
Prostate cancer is the most common cancer in men, with surgery being the primary treatment. Neuraxial anaesthesia for laparoscopic prostatectomy is a viable and safe approach, offering reduced postoperative pain and fewer minor complications compared to the same procedure under general anaesthesia. We report the case of a 77-year-old patient who underwent an ‘awake’ robotassisted laparoscopic prostatectomy using a combination of ultrasound-guided intermediate cervical plexus block and neuraxial (thoracic spinal) anaesthesia. A sacral erector spinae plane block was performed at the end of the procedure for postoperative pain management.
Keywords: Awake Robot-Assisted Laparoscopic Prostatectomy; Cervical Plexus Block; Phrenic Nerve.
Introduction
Modern surgery has been revolutionised by the laparoscopic approach, with its numerous advantages, across various specialties, from general surgery to gynecology and urology. The general anaesthesia is typically recommended for this type of surgery, even in patients with many comorbidities. To mitigate many of its effects, avoid the need for airway manipulation, and prevent the use of opioids in postoperative pain management, regional anaesthesia has also been proposed in selected cases
for laparoscopic procedures, allowing the patient to breathe spontaneously, only sedated during the surgery [1]. Prostate cancer is the commonest form of cancer in men, and surgery represents the mainstay of treatment for localised cancer in patients with good general health. A prospective comparative study revealed that laparoscopic radical prostatectomy under neuraxial anaesthesia is a feasible and safe procedure, with less postoperative pain and fewer minor complications than the same procedure under general anaesthesia, allowing muscle relaxation and respiratory mechanics without interfering with surgery [2]. Regional anesthesia, particularly neuraxial anesthesia, presents challenges that must be carefully considered, especially the risk of hypotension due to the need for extensive dermatomal coverage. For pelvic procedures, this coverage must extend from the sacral areas to C3-4 to include the phrenic nerve and prevent shoulder-tip pain, which can often worsen postoperative outcome [3].
Herein, we present the case of a patient who underwent ‘awake’ robot-assisted laparoscopic prostatectomy (RALP) for cancer, in which an intermediate cervical plexus block was added to prevent shoulder-tip pain without evidence of phrenic nerve paralysis and without complications. A sacral erector spinae plane block was performed at the end of the procedure for postoperative pain management.
Case Report
A 77-year-old patient (weight 73 Kg, height 177 cm, BMI 23 Kg.m-²), with a history of premature (extra-systolic) ventricular beats, under treatment with flecainide, ASA III, was scheduled for robot-assisted prostatectomy due to adenocarcinoma (Gleason score 6). With the patient’s written consent, a plan was devised for a combination of ultrasound-guided intermediate cervical plexus block and neuraxial (thoracic spinal) anaesthesia. Vital parameters were monitored. Three mg of intravenous midazolam were administered. Before the procedure blood pressure was 190/95 mmHg, SpO2 96%, and heart rate of 76.min-1. Under aseptic conditions, an intermediate cervical plexus block was performed by using an echogenic 50 mm needle (UltraplexTM, B.Braun, Melsungen AG, Germany), under ultrasound guidance (EDGE II, FUJIFILM-SonositeTM, Bothwell, WA),between the sternocleidomastoid muscle and prevertebral fascia and using 0.25% levobupivacaine 8 ml plus dexmedetomidine 10 mcg (Figure 1, a). The patient was then placed in a sitting position, and under sterile conditions, after 500 ml of intravenous crystalloid infusion, a spinal anaesthesia was performed at T9 level with a 25-gauge Quincke needle via paramedian approach, injecting 0.5% levobupivacaine 2,5 ml (12.5 mg) and 0.20% hyperbaric bupivacaine 2,5 ml (5 mg) [4]. Then, under monitoring of the vital parameters, the patient was repositioned supine. After 20 minutes, a sensory block (by pinprick test and ice) was ascertained up to T2 level. No significant hemodynamic variations occurred, except for a well-tolerated episode of bradycardia (40.min-1) that did not require medication. The patient was then introduced in the operating room, under standard monitoring, with oxygen administered via nasal cannulae at 5 L.min-1, and intravenous sedation was initiated with propofol infusion (0.5 mg.kg-1.h-1). No patient’s discomfort or hemodynamic complications were noted at the moment of surgical incision and pneumoperitoneum induction (12 mmHg). Trendelenburg position (28 degrees) caused no changes in consciousness and in hemodynamics. Capnometry was used to have a more reliable insight into the patient’s ventilation and diaphragmatic function was not involved as ultrasound check demonstrated.
The surgery lasted 120 minutes and it was uneventful. The patient, during the procedure, reported drowsiness (modified Ramsay Sedation score 3-4), and dry mouth. At the end of the operation, the patient was awake, mildly dysphonic due to hoarseness (which resolved spontaneously after three hours), with hypoesthesia in the lower limbs without motor deficits. At discharge from the operating room, blood pressure was 100/74 mmHg, SpO2 96%, and HR 55.min-1, with ALDRETE score of 9.
For the postoperative analgesia, with the patient’s informed consent, aseptically, a single-injection S1 median sacral erector spinae plane (ESP) block was performed under ultrasound guidance with the patient in lateral position, and using 80 mm echogenic needle. A solution comprising 0.25% levobupivacaine 30 ml plus dexamethasone 4 mg was injected (Figure 1, b). The patient was fed two hours after returning to the ward, mobilized in bed, and then standing after three hours.
In the following 24 hours postoperatively, the patient reported an NRS-score of 0 both at rest and during movement. He was given 1 g of intravenous paracetamol for discomfort at the surgical scars. The patient was discharged on the third day, without any complications (Clavien-Dindo 1) [5].
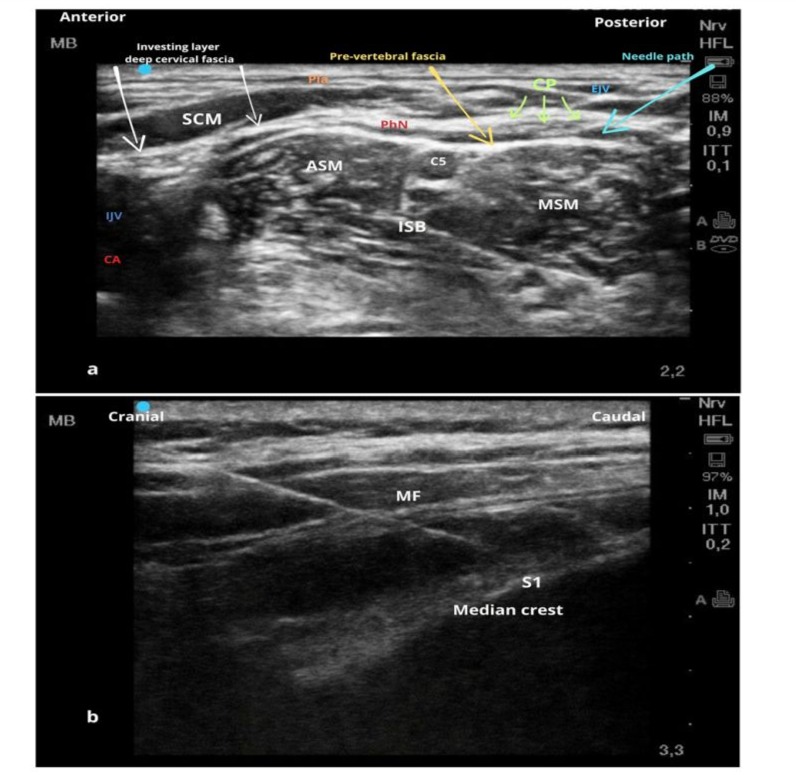
Figure 1: a: Cervical Plexus (transverse view). The cervical plexus emerges behind the posterior border of the sternocleidomastoid muscle. Branches of the cervical plexus can be seen superficial to the prevertebral fascia which covers the middle and anterior scalene muscles, and posterior to the sternocleidomastoid muscle. For the intermediate cervical plexus block, the injection is placed between the investing layer of the deep cervical fascia and the prevertebral fascia, the needle goes through the skin, platysma, and enveloping layer of the deep cervical fascia, with the tip placed next to the plexus. Pla, platysma muscle; SCM, sternocleidomastoid muscle; ASM, anterior scalene muscle; MSM, middle scalene muscle; EJV, external jugular vein; CP, cervical plexus; PhN, phrenic nerve; IJV, internal jugular vein; CA, carotid artery, ISB, Interscalene brachial plexus. b: Sacral Erector Spinae Plane (ESP) block involves the injection of local anaesthetic under the multifidus muscle plane, at median or intermediate sacral crest. MF, multifidus muscle.
Discussion
The intermediate cervical plexus block was first described in 2007 and involves the injection of local anaesthetic into the fascial plane between the sternocleidomastoid muscle and the prevertebral fascia at the C4 level [6]. It has been successfully used in thyroid, ear, and carotid surgery. Additionally, unlike the deep cervical block, the intermediate one does not cause diaphragmatic paresis [7] and if performed with low-concentration local anaesthetic (0,2 ml.Kg-1 of 0.25% ropivacaine) does not block the motor function of the phrenic nerve after thyroidectomy [8].
Our hypothesis of combining an intermediate cervical plexus block with a neuraxial technique during laparoscopy stems from the idea that this combination may prevent the activation of pain caused by irritation of the diaphragmatic peritoneum (related to the phrenic nerve). This, in turn, reduces the need for extensive neuraxial coverage, as it no longer needs to reach higher dermatomal levels.
Our plan, therefore, involved thoracic segmental spinal anaesthesia [9] (typically between T9 and T12), with local anaesthetic administered, at two different form of baricity both isobaric and hyperbaric to also target the more caudal nerve roots. In combination, an intermediate cervical block with a low concentration of local anaesthetic was used to achieve sensory blockade of the phrenic nerve, without causing diaphragmatic paralysis. The advantages of this technique are the ability to prevent shoulder pain, avoid a high spinal block, and potentially limit adverse cardiovascular effects.
The only side effects we encountered were an episode of bradycardia, likely related to the intrathecal administration of dexmedetomidine, along with dry mouth and transient dysphonia. Hemodynamics and respiratory function were never compromised. The patients did not experience motor weakness of the limbs. The limitations of this technique lie in the need to perform not only spinal (thoracic) anaesthesia but also an additional block, which requires technical expertise and can be challenging in certain anatomical conditions.
As it is not possible to completely exclude motor involvement of the phrenic nerve, careful monitoring of the patient is mandatory to ensure a prompt management of the airways and ventilation. And, patient-by-patient evaluation of the risks / benefits is pivotal. Interestingly, for the postoperative analgesia coverage, we placed the sacral ESP block, which was performed at the end of the surgical procedure.
Pain after RALP is typically mild to moderate, and no specific analgesic technique has convincingly demonstrated its superiority [10]. Fascial plane blocks and abdominal wall blocks, such as the transversus abdominal plane (TAP) block have been used for RALP. The subcostal TAP block has been shown to reduce immediate postoperative pain after RALP; however, there was no difference in pain scores leaving the post-anaesthetic care unit less than one hour later, nor was there a reduction 24-hour opioid consumption compared to standard management [11]. Another issue related to RALP is postoperative bladder spasm. Some evidence suggests that intrathecal bupivacaine/morphine may result in a modest reduction in patient-reported bladder spasms [12]. To eliminate the postoperative opioid consumption and to reduce bladder spasms and catheter-related discomfort [13], we placed a sacral ESP block at the end of the operation. This block, which has recently gained attention, has been described for covering the posterior roots of the sacral spinal nerves. Clinical experiences in various surgical contexts, along with anatomical studies [14,15] indicate that the volume of local anaesthetic can spread in a cephalic and anterior direction starting from the fascial plane beneath the sacral multifidus muscle, providing coverage in both the sacral and lumbar dermatomes. It is advisable to use an adequate volume of injectate, as with all fascial plane blocks, to achieve a dynamic hydro-dissection effect of the involved fascia. The main limitation of this block is the unpredictability of the extent of dermatomal coverage; however, in a multimodal postoperative pain management approach, this block has proven to be very useful in many contexts. Further studies are needed to better clarify all these approaches in the different surgical contexts.
Consent of Patient: This case report was published with the written consent of patient.
Funding: No external funding and no competing interests declared.
Authors’ contribution statement: the authors confirm contribution to the paper as follows: study conception and design: L. Forasassi, F. Marrone, C. Pullano; data collection: L. Forasassi, F. Marrone; analysis and interpretation of results: L. Forasassi, F. Marrone, R. Starnari, C. Pullano; draft manuscript preparation: F. Marrone and L. Forasassi.All authors reviewed the results and approved the final version of the manuscript.
References
- Bajwa SJ, Kulshrestha A. (2016) Anaesthesia for laparoscopic surgery: General vs regional anaesthesia. J Minim Access Surg 12:4-9.
- Alba S, Fimognari D, Crocerossa F, Acalone L, Pullano C, et al. (2023) Neuraxial anesthesia versus general anesthesia in patients undergoing three-dimensional laparoscopic radical prostatectomy: Preliminary results of a prospective comparative study. Asian J Urol 10:329-36.
- Tzovaras G, Fafoulakis F, Pratsas K, Georgopoulou S, Stamatiou G, et al. (2006) Laparoscopic cholecystectomy under spinal anaesthesia: A pilot study. Surg Endosc 20:580-2.
- Imbelloni L, Gouveia M, Ghorayeb N, Maluf N, Neto S (2021) Spinal anesthesia: much more than single shot of hyperbaric bupivacaine. Int J Anaesth Anesthesiol 8:122.
- Mitropoulos D, Artibani W, Biyani CS, Jensen JB, Roupret M, et al. (2018) Validation of the Clavien-Dindo Grading System in Urology by the European Association of Urology Guidelines Ad Hoc Panel. Eur Urol Focus 4:608-613.
- Pandit JJ, Satya-Krishna R, Gration P. (2007) Superficial or deep cervical plexus block for carotid endarterectomy: a systematic review of complications. Br J Anaesth 99:159-69.
- Opperer M, Kaufmann R, Meissnitzer M, Enzmann F, Dinges C, et al. (2022) Depth of cervical plexus block and phrenic nerve blockade: a randomized trial. Reg Anesth Pain Med 47:205-11.
- Kim, HY, Soh, EY, Lee, J, Kwon SH, Hur M, et al. (2020) Incidence of hemi-diaphragmatic paresis after ultrasound-guided intermediate cervical plexus block: a prospective observational study. J Anesth 34: 483-90.
- le Roux JJ, Wakabayashi K, Jooma Z. (2023) Defining the role of thoracic spinal anaesthesia in the 21st century: a narrative review. Br J Anaesth 130:e56-e65.
- Milliken D, Lawrence H, Brown M, Cahill D, Newhall D, et al. (2021) Anaesthetic management for robotic-assisted laparoscopic prostatectomy: the first UK national survey of current practice. J Robot Surg 15:335-41.
- Taninishi H, Matsusaki T, Morimatsu H. (2020) Transversus abdominis plane block reduced early postoperative pain after robot-assisted prostatectomy: a randomized controlled trial. Sci Rep 10:3761.
- Koning MV, Vlieger R, Teunissen AJW, Gan M, Ruijgrok EJ, et al. (2020) The effect of intrathecal bupivacaine/ morphine on quality of recovery in robot‐assisted radical prostatectomy: a randomised controlled trial. Anaesthesia 75:599–608.
- Olgun Keleş B, Tekir Yılmaz E, Altınbaş A. (2024) Comparison between the efficacy of sacral erector spina plane block and pudendal block on catheter-related bladder discomfort: A prospective randomized study. J Clin Med 13:3617.
- Diwan S, Garud R, Sancheti P. (2022) Deciphering the Mechanism of Continuous Sacral Erector Spinae Block: A Cadaveric Study. Turk J Anaesthesiol Reanim 50:471-3.
- Keleş BO, Salman N, Yilmaz ET, Birinci HR, Apan A, et al. (2024) Comparison of the median and intermediate approaches to the ultrasound-guided sacral erector spinae plane block: a cadaveric and radiologic study. Korean J Anesthesiol 77:156-63.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.