Atypical Deep-Seated Lipomatous Tumors of the Shoulder: A Case Series
by Giuseppe Porcellini1, Valentina Passarino1*, Alberto Brigo1, Andrea Giorgini2, Gian Mario Micheloni2, Alessandro Donà1, Rocco Bonfatti1, Luigi Tarallo1
1University of Modena and Reggio Emilia, Modena, Italy
2Shoulder Team Forlì, Forlì, Italy
*Corresponding Author: Valentina Passarino, Department of Orthopedics and Traumatology, University of Modena and Reggio Emilia, 41124 Modena, Italy
Received Date: 13 June 2025
Accepted Date: 19 June 2025
Published Date: 21 June 2025
Citation: Porcellini G, Passarino V, Brigo A, Giorgini A, Micheloni GM, et al. (2025) Atypical Deep-Seated Lipomatous Tumors of the Shoulder: A Case Series. J Surg 10: 11353 https://doi.org/10.29011/2575-9760.011353
Abstract
Lipomas are common subcutaneous tumors composed of adipose tissue, often encapsulated by a thin layer of fibrous tissue. They typically do not cause symptoms or problems but in some cases they can result in pain or functional limitations. In these cases, surgical removal should be considered but it is important to evaluate the adjacent vascular and nerve structure. The purpose of this study is to report the surgical treatment and the outcomes of surgical procedure on symptomatic lipomas. We present the cases of ten patients who were treated for shoulder lipomas. The most common symptoms were pain and shoulder functional limitation. The definitive diagnostic test was MRI. All patients underwent surgical excision of the tumors. In three cases the external compression of the nervous structures caused paralysis of the involved structures. At the end of follow up all patients experienced complete healing and full recovery of shoulder mobility. In our experience, sensory-motor deficits related to nerve structure compression have alwayscresolved within a few months.
Keywords: Lipoma; Nerve compression; Sensory-motor deficit; Shoulder; Surgical excision
Introduction
Lipomas are benign mesenchymal tumors and represent the most common type of soft tissue tumors [1]. Lipomas can occur at any age, but they are most commonly found in individuals between 40 and 70 years of age. There does not appear to be a significant gender predisposition. These tumors can arise in various anatomical locations, with the most common sites being the thigh, followed by the shoulder [2]. The etiopathogenesis of lipomas remains not fully understood. Some researchers suggest a genetic predisposition as a key factor in their development, while others hypothesize that trauma may play a central role [3]. Additionally, studies have found an association between lipomas and conditions such as diabetes mellitus and dyslipidemia [4]. Diagnosis of lipoma is typically made through a physical examination. Imaging studies (such as CT or MRI) or a biopsy may be needed to confirm the diagnosis and assess the nature of the lesion. Is important to consider differential diagnosis with malignant formations. A lipoma grows slowly and is benign. A liposarcoma is a malignant tumor that also originates from fat cells. Liposarcomas grow rapidly and they can invade surrounding tissues and spread to other parts of the body. Liposarcomas are rarer and more aggressive than lipomas [5]. The differential diagnosis is typically clinical, supported by ultrasound or Magnetic Resonance Imaging (MRI). Lipomas on MRI typically have well-defined, regular margins and homogeneous in appearance. Liposarcomas, on the other hand, tend to have irregular or indistinct margins and may invade surrounding tissues. A biopsy is rarely required, but may be performed if the tumor exhibits atypical features.
In cases where lipomas cause pain and functional limitations, surgical removal may be necessary. However, their removal is not always straightforward. In some cases, lipomas can compress or infiltrate adjacent nerve structures. During surgical removal, it is important to avoid causing iatrogenic damage. Therefore, it is crucial to assess the potential involvement of nerves before surgery using electromyography and sometimes during the surgery with electrostimulation. In this study, we analyzed ten cases of atypical shoulder lipomas. All patients presented with symptomatic lipomas, resulting in pain, functional limitations, reduced range of motion (ROM) in the shoulder and impact on quality of life. All patients were treated with surgical excision, which remains the treatment of choice for symptomatic lipomas, as well as for cosmetic reasons.
Case Presentation
In this article, we report ten cases of patients who underwent surgery for shoulder lipomas between 2019 and 2024. The patients were consecutively treated at the following hospital facilities: Policlinico di Modena, Ospedale Civile di Sassuolo, and Ospedale Civile di Baggiovara. The patients were aged between 42 and 59 years. All patients reported pain or functional limitations, which prompted them to seek evaluation by an orthopedic specialist. Following physical examination and imaging investigations, the presence of a shoulder lipoma was diagnosed. All patients underwent imaging studies. Before the surgical procedure all the patients underwent MRI. This was crucial for evaluating the soft tissues, identifying the lipoma’s margins and boundaries, and assessing its relationship with surrounding structures. In some cases, the borders of the lipoma were poorly defined, making it difficult to determine the extent of infiltration into the surrounding muscles. In all cases in which there was involvement of nerve structures or symptoms that raised suspicion of nerve involvement, electromyography of the adjacent nerve structures was performed to assess their potential involvement. The characteristics of the ten patients are summarized in Table 1.
|
SEX |
AGE |
LOCATION |
INVOLVED NERVE STRUCTURES |
DIMENSION |
HISTOLOGICAL DIAGNOSIS |
HOSPITAL |
|
|
1 |
F |
47 |
Sovraspinatus |
Suprascapular nerve |
7x7 cm |
lipoma |
Ospedale civile di Sassuolo |
|
2 |
F |
59 |
Between the subscapularis and pectoralis minor |
Musculocutaneous nerve |
12x8 cm |
lipoma |
Ospedale civile di Baggiovara |
|
3 |
M |
56 |
Between the trapezius and rhomboid muscles |
Accessory nerve |
fibrolipoma |
Ospedale civile di Sassuolo |
|
|
4 |
F |
42 |
Anterior portion of the shoulder |
lipoma |
Policlinico di Modena |
||
|
5 |
F |
56 |
Biceps brachii |
13x7 cm |
lipoma |
Ospedale civile di Baggiovara |
|
|
6 |
M |
57 |
Inferior pole of scapula |
6.8x5 cm |
elastofibroma |
Ospedale civile di Baggiovara |
|
|
7 |
F |
53 |
Inferior pole of scapula |
lipoma |
Ospedale civile di Baggiovara |
||
|
8 |
M |
58 |
Inferior pole of scapula |
lipoma |
Ospedale civile di Baggiovara |
||
|
9 |
M |
56 |
Inferior pole of scapula |
lipoma |
Ospedale civile di Baggiovara |
||
|
10 |
F |
48 |
Inferior pole of scapula |
lipoma |
Ospedale civile di Baggiovara |
Here we report the 3 most representative cases out of the 10 listed in Table 1.
Case 1
A 47 years old female patient with a large masse that was clinically palpable into the supraspinatus fossa. She reported neuropatic shoulder pain and weakness of the supraspinatus and infraspinatus muscles during clinical examination. The MRI revealed a lipoma that compressed the suprascapular nerve. A surgical procedure of mass excision was proposed. The lipoma was found to be 7x7 cm. It was sent to anatomic pathology, where it was identified as a lipoma (Figure 1).
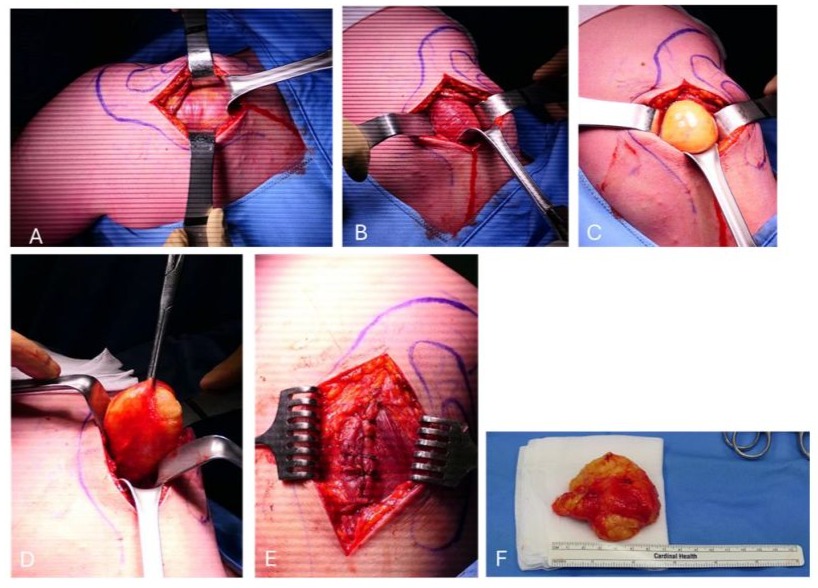
Figure 1: The different steps of the surgical removal of one of the reported cases are shown. A.Resection of the trapezius; B. Resection of supraspinatus; C. The lipoma was clearly visible; D. The excised and removed lipoma; E. Muscular plane closure; F. Lipoma was misured 7x7 cm.
At the hospital discharge the patient was suggested to early begin a rehabilitation program and take N-Acetyl-carnitine supplementation for suprascapular nerve recovery. At one month follow up the patient had a complete passive range of motion but was still weak in active forward flexion, abduction and external rotation, 4 out of 5 of the Medical Research Council scale (MRC). Fully recovery of the supraspinatus and infraspinatus was assessed one month later with recovery of strength (5/5 MRC) in all planes movements and resistance symmetrical to the opposite shoulder.
Case 2
A 59 years old female patient reported lymphedema of the upper limb, weakness of the elbow flexors and hypoesthesia of the lateral forearm. The patient underwent MRI and was evaluated by a vascular surgeon who suggested the surgical excision of the lipoma, since the symptoms were probably due to axillary vessels and muscolocutaneus nerve compression. In Figure 2 the MRI images of this patient are reported, shown in the coronal plane(A), assial plane (B).
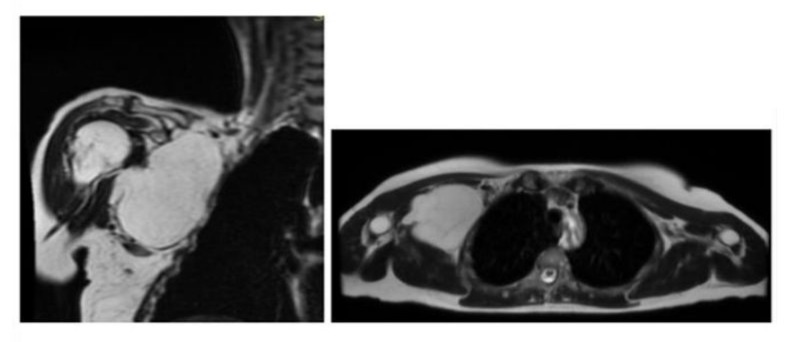
Figure 2: A. Coronal plane; B. Assial plane.
A large mass was excised from the right infraclavicular pectoralis minor intermuscular plane (Figure 3). A lipomatous nodular formation measuring 12x8x6cm.
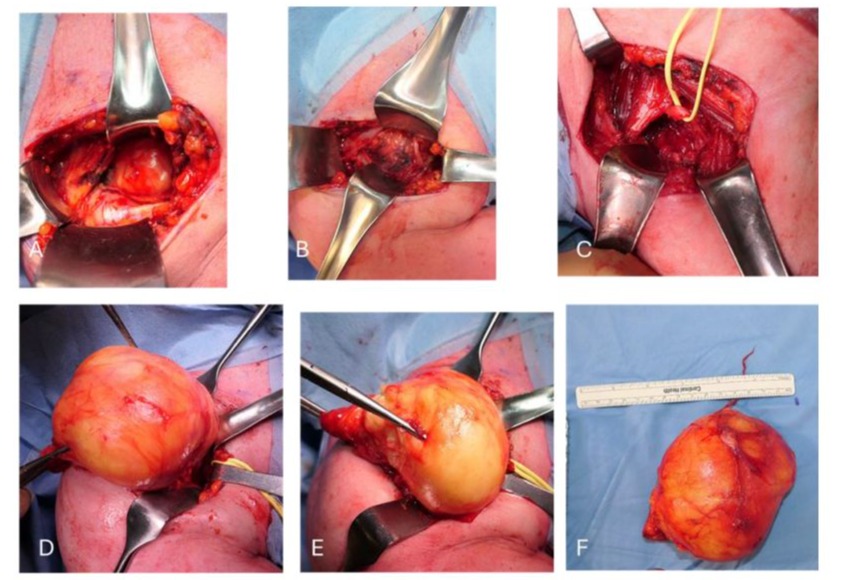
Figure 3: The different steps of the surgical removal of one of the reported cases are shown. A,B. Infraclavicular and pectoralis minor intermuscolar plane; C. Isolation of cephalic vein; D,E. Excision of the lipoma, F. Lipomatous nodular formation measuring 12x8x6cm.
Case 3
A 56 years old male patient presented a lipoma at the scapular level. After performing MRI and electromyography of the accessory nerve, the patient underwent surgery. Intraoperative electrostimulation of the accessory nerve and its branches was performed, with the presence of a neurosurgeon (Figure 4).
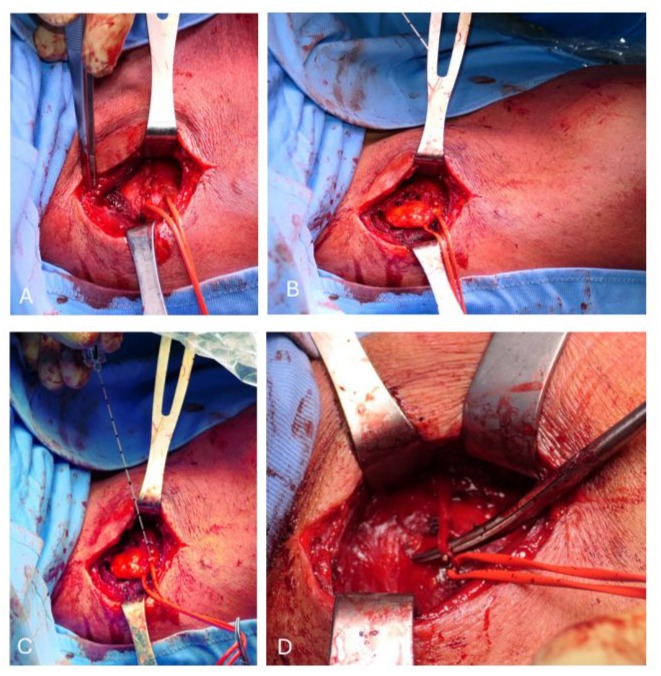
Figure 4: The different steps of the surgical removal of one of the reported cases are shown. A,B. Dissection proceeded through the planes between the trapezius and rhomboid muscles, where the accessory nerve and its branches were identified and isolated. These structures were protected throughout the surgery. C. Intraoperative electrostimulation of the accessory nerve and its branches. D. Neuroma of the accessory nerveThe fibrolipoma was then isolated and completely removed. Additionally, a neuroma of the accessory nerve was removed.
Discussion
In this article, we presented ten cases of shoulder lipomas that caused significant discomfort to patients. The average age of the patients was in accordance with that found in the literature [2]. In all cases the problem was not only cosmetic but mainly the presence of pain and functional limitation because of the lipoma. In all cases, this led to a specialist examination and a secondlevel examination such as MRI. The MRI results confirmed the diagnosis and guided the decision to proceed with surgical excision. The excisions involved complete removal of the lipomas and their capsules. In some cases, electromyography was performed to evaluate the adjacent nerve structures, which were in fact giving symptoms in some cases. In one case, intraoperative nerve stimulation was necessary to avoid iatrogenic damage. This is an important aspect to evaluate when planning a lipoma removal surgery; the adjacent nerve and vascular structures must be studied and has to be considered. In one case, with a lipoma at the inferior pole of the scapula, a hematoma formed in the cavity previously occupied by the lipoma in the postoperative period. The patient was then returned to the operating room to drain the hematoma, with a drain kept in place for 2 days. In all cases, after surgical removal, patients fully recovered shoulder mobility. In all cases where there was nerve involvement, symptoms regressed within 6 months after surgery. For all we know, no recurrence of the lipoma was reported by the patients.
Conclusions
Atypical shoulder lipomas are benign tumors. The diagnosis is typically confirmed by MRI. If the lipomas are asymptomatic, they may not require treatment. However, when they cause pain or functional limitations, surgical removal is often recommended, followed by histological examination. Before proceeding with the removal of the lipoma, it is important to assess the relationship with the nervous and vascular structures to avoid iatrogenic injuries. It is advisable to perform an electromyography to assess the relationship with the adjacent nerve structures and their involvement. Sometimes, it may be necessary to use intraoperative nerve stimulation methods for the affected nerves. In the cases where treatment is necessary, surgical excision has proven to be the most effective option. In all treated cases, resolution of functional limitations and other issues, such as those related to vascular or nerve compression caused by the lipoma, was achieved. In cases where there was nerve involvement, the pain stabilized a few months after the surgery.
References
- Murphey MD, Carroll JF, Flemming DJ, Pope TL, Francis HG, et al. (2004) From the archives of the AFIP: benign musculoskeletal lipomatous lesions. Radiographics 24: 1433-1466
- Nishida J, Morita T, Ogose A, Okada K, Kakizaki H, et al. (2007) Imaging characteristics of deep-seated lipomatous tumors: intramuscular lipoma, intermuscular lipoma, and lipoma-like liposarcoma. J Orthop Sci 12: 533-541.
- Copcu E (2003) Can intramuscular lipoma have a post-traumatic origin? Br J Dermatol 149: 1084-1085.
- Ramos-Pascua LR, Guerra-Álvarez OA, Sánchez-Herráez S, Izquierdo-García FM, Maderuelo-Fernández JÁ (2013) Lipomas intramusculares: bultos benignos grandes y profundos. Revisión de una serie de 51 casos [Intramuscular lipomas: Large and deep benign lumps not to underestimated. Review of a series of 51 cases]. Rev Esp Cir Ortop Traumatol 57: 391-397.
- Johnson CN, Ha AS, Chen E, Davidson D (2018) Lipomatous Softtissue Tumors. J Am Acad Orthop Surg 26: 779-788.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.