Arthroscopic Tenotomy Results in Complete Resolution of Snapping Popliteus Tendon Syndrome After Total Knee Arthroplasty-A Case Report
by Alexander K. Bishop, Chase E. McIntosh, Michael V. Jablonski, Bruce A. Levy*
Orlando Health Jewett Orthopedic Institute, Orlando, Florida, USA
*Corresponding Author: Bruce A. Levy, Orlando Health Jewett Orthopedic Institute, Orlando, Florida, USA
Received Date: 16 July 2025
Accepted Date: 23 July 2025
Published Date: 25 July 2025
Citation: Bishop AK, McIntosh CE, Jablonski MV, Levy BA (2025) Arthroscopic Tenotomy Results in Complete Resolution of Snapping Popliteus Tendon Syndrome After Total Knee Arthroplasty-A Case Report. J Surg 10: 11389 https://doi.org/10.29011/2575-9760.011389
Abstract
Introduction: Snapping Popliteus Tendon Syndrome (STPS) is a rare complication following Total Knee Arthroplasty (TKA) characterized by painful, palpable and audible snapping in the lateral knee. Our case demonstrates complete resolution of SPTS with exclusively diagnostic and therapeutic popliteus tendon sheath injection followed by arthroscopic popliteus tendon tenotomy.
Case Presentation: We present the case of a 60-year-old female 5 weeks status post TKA who presents with SPTS despite following postoperative rehabilitation protocol. Palpable snapping was elicited on the posterolateral aspect of the knee upon passive ROM examination. The patient had complete relief following ultrasound guided tendon sheath injection for 3 weeks, followed by arthroscopic tenotomy which demonstrated clear trapping of the popliteus tendon in the arthroplasty components.
Results: The patient reported 85% improvement in all symptoms by 2 weeks, return to significant physical activity by 8 weeks, and continued complete resolution of snapping sensation and pain at final follow up, 10 months postoperatively.
Conclusions: Isolated arthroscopic popliteus tenotomy offers a minimally invasive, anatomy-preserving treatment for SPTS postTKA and does not lead to rotatory instability of the components. The application of dynamic ultrasound with guided injection is a strong diagnostic tool for dynamic tendon pathology.
Keywords: Arthroscopic Tenotomy; Popliteus Tendon; Snapping Popliteus Tendon Syndrome (SPTS); Tendon Sheath Injection; Total Knee Arthroplasty (TKA)
Introduction
Painful snapping sensations on the lateral side of the knee following Total Knee Arthroplasty (TKA) are rare but clinically significant and may impair postoperative function and patient satisfaction. One uncommon source of such symptoms is Snapping Popliteus Tendon Syndrome (SPTS), in which the popliteus tendon subluxates or impinges during knee movement, producing a palpable or audible snap and consequent pain [1-3]. Although SPTS has been documented in pediatric and athletic populations, its presentation after TKA is exceptionally rare [15]. The popliteus muscle is essential for initiating knee flexion by internally rotating the tibia to release the joint from full extension. The tendon runs obliquely through the posterolateral corner, inserting into the lateral femoral condyle [3]. When impinged, particularly in altered biomechanics following TKA, the tendon may “snap” over adjacent structures or the implant components, creating a reproducible popping sensation accompanied by lateral knee pain [6,7]. We report a unique case of a patient who presented with post-TKA snapping due to SPTS that achieved complete symptom resolution with isolated arthroscopic popliteal tenotomy. This case supports the role of dynamic diagnostic assessment and highlights a minimally invasive solution for a complex and rare post-TKA condition.
Case Presentation
The patient is a 60-year-old female with past medical history significant for previous arthroscopic meniscus repair, with a Body Mass Index (BMI) of 22.02 kg/m2 who presents with painful incapacitating lateral knee snapping which began 5 weeks post right TKA MAKOplasty. The patient states that the posterolateral snapping in her right knee occurs as the knee goes from flexion to full extension. The symptoms are reproducible when squatting, exacerbated by ambulation, and worse at night. The patient has been compliant with postoperative physical therapy and takes antiinflammatory medications to manage her symptoms but denies any significant improvement in her painful knee snapping.
Clinical Findings
On clinical examination, the right knee demonstrated full extension to 125 degrees of flexion. During active Range Of Motion (ROM), palpable snapping was elicited on the posterolateral aspect of the knee at the level of the popliteus. Upon inspection, the patient had a non-antalgic gait, no effusion, and no malalignment of the lower limb. Additionally, there was no knee ligamentous instability, proximal tibia-fibula joint instability, joint line tenderness, or biceps femoris tenderness.
Diagnostic Test Findings
Standard radiographs taken 6 weeks status post right TKA demonstrated anatomic positioning of the components with a well centered patellar button and no signs of loosening or early complications, specifically no evidence of tibial baseplate overhang or femoral component oversizing (Figures 1a,1b,1c).
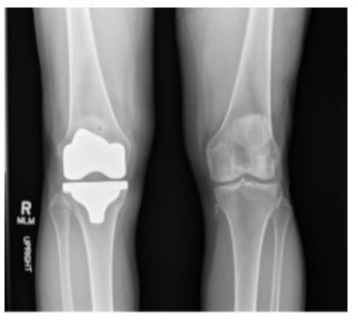
Figure 1a: Anteroposterior view.

Figure 1b: Lateral view.
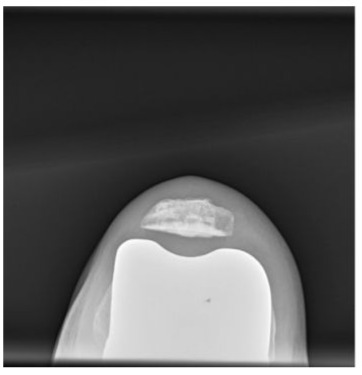
Figure 1c: Sunrise view.
A diagnostic dynamic ultrasound was performed which confirmed the diagnosis of SPTS clearly visualizing the popliteus tendon snapping in the posterolateral side of the knee and reproducing the patient’s symptoms. The tendon was noted to be otherwise normal with some thickening and signs of tendinosis. At that time, the popliteus tendon sheath was subsequently injected with 2mL 0.2% lidocaine, and 1cc of 40mg/mL Kenalog for both diagnostic and therapeutic purposes. The patient was seen again 5 weeks status post popliteus sheath injection and reported 3 weeks of near-complete pain relief after the injection, including reduced snapping frequency. Given the symptom improvement with the popliteus tendon sheath injection, the patient was deemed a viable candidate for arthroscopic versus open popliteus tenotomy. The patient elected to proceed with surgical treatment accordingly.
Surgical Intervention
The right knee ROM was measured passively under anesthesia and found to be 0 to 130 degrees. Snapping of the popliteus was felt posterolaterally, as well as significant crepitation through knee range of motion going from flexion into extension. Attention was turned to arthroscopy. Standard anterolateral and anteromedial portals were established with blunt trocars and smooth cannulas (Pivot TM). Extreme care was taken to avoid any iatrogenic damage to the TKA components. Under direct visualization, an accessory mid-lateral portal was then established in the region of the femoral insertion of the popliteus tendon, which sits in the anterior aspect of the popliteus socket in the distal lateral femur (Figures 2a,2b).
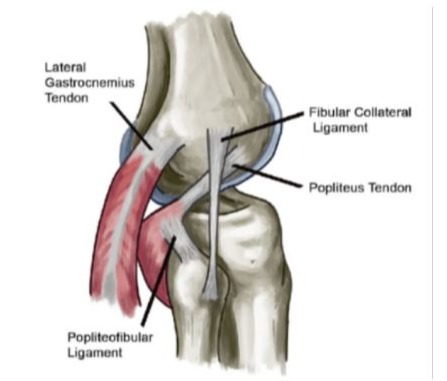
Figure 2a: Anatomical rendering of the origin of the popliteus tendon on the distal lateral femur.
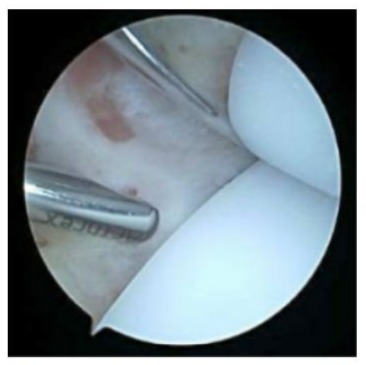
Figure 2b: Arthroscopic view from the anteromedial portal. Shaver seen on left through the anterolateral portal. Creation of accessory mid-lateral portal with needle.
With the scope in the anterolateral portal, the popliteus tendon was readily identified. The tendon was significantly frayed with partial thickness tearing at the level of the tibial component. The source of the snapping became readily apparent as a portion of the tendon was clearly trapped between the polyethylene spacer and the posterior aspect of the femoral component (Figures 3a,3b).
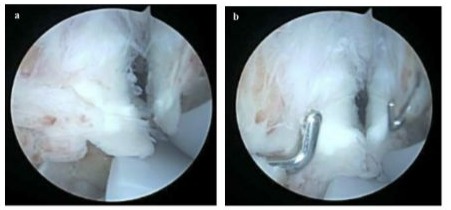
Figures 3a, 3b: View from anterolateral portal showing the probe through the accessory mid-lateral portal. Popliteus tendon is visualized originating from the lateral femur. The thickened popliteus tendon with excess tissue is seen becoming trapped in the femoral component causing the snapping sensation.
The popliteal hiatus was then identified, and several small loose bodies were removed (Figure 4a). Complete tenotomy of the popliteus tendon was performed with careful debridement down the posterior aspect of the tibia to ensure no further snapping would occur from tendon remnants (Figure 4b). A small amount of scar tissue was debrided posteriorly behind the polyethylene implant from the accessory anterolateral portal.
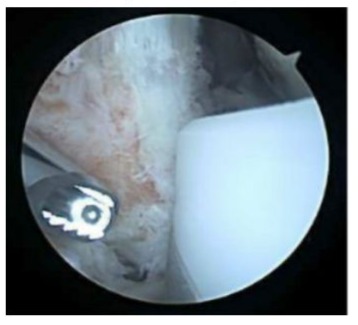
Figure 4a: View of popliteus tendon post tissue debridement. Shaver is seen through the accessory mid-lateral portal.
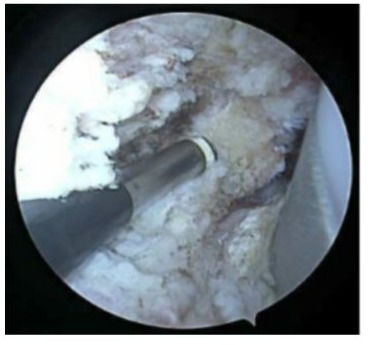
Figure 4b: View from the anterolateral portal showing the remaining muscle-tendon junction of the popliteus tendon after complete tenotomy from its femoral attachment. Radiofrequency device seen through the mid lateral portal. Also note, no evidence of tibial baseplate prominence.
Post tenotomy, a thorough ROM assessment was performed and confirmed complete resolution of all snapping and crepitation from the posterolateral region of the knee.
Results
Follow-up and Outcome
The complete patient timeline is summarized in Table 1 from onset of symptoms post TKA through arthroscopic tenotomy and follow-up protocol.
|
Comprehensive Patient Timeline |
|
|
Time Since TKA |
Encounter |
|
5 weeks |
First complaint of right knee pain and popping. X-ray and CT obtained |
|
6 weeks |
Diagnostic ultrasound with tendon sheath injection |
|
Reported 3 weeks of complete cessation of symptoms |
|
|
3 months |
Arthroscopic popliteus tenotomy |
|
Time Since Arthroscopic Tenotomy |
|
|
3 months |
Diagnostic ultrasound documenting resolution of snapping |
|
10 months |
Final post operative visit with complete resolution of all symptoms |
All clinical parameters showed continued improvement throughout the postoperative period. A second diagnostic ultrasound was performed 3 months postoperatively and documented complete resolution of the preoperative snapping. At final follow up, the patient also noted complete resolution of the painful posterolateral knee snapping and denied any knee instability symptoms. Additionally, clinical examination demonstrated no evidence of posterolateral knee instability with a negative dial test at 30 and 90 degrees as well as a negative posterolateral rotatory drawer test.
Post-operative Milestones & Subjective Results | |
Postoperative Time Point | Milestones & Subjective Findings |
Weeks | • 85% improvement of all symptoms |
• Expected postoperative residual symptoms | |
Weeks | • Continued significant improvement |
• Patient able to walk 6+ miles without complications | |
Weeks | • Current pain is rated a 2/10 |
• Patient has returned to pre-operative activity level including 100 squats and 100 lunges | |
• Ultrasound demonstrates no continued snapping | |
Months | • Complete resolution of snapping sensation |
• Pain rated a 0/10 | |
• No perceived instability | |
Table 2: Summarizes the patient’s progression through the postoperative period.
Discussion
SPTS is an uncommon and likely underdiagnosed cause of lateral knee snapping and pain, particularly in the post-TKA population [8]. Most reported cases have involved younger non-arthroplasty patients, often with anatomical variants or mechanical subluxation of the tendon over the lateral femoral condyle [1-7]. In the setting of TKA where altered joint mechanics and soft tissue tensioning may exacerbate dynamic impingements, the popliteus can become a source of persistent pain and snapping despite adequate postoperative recovery measures. However, this diagnosis is rarely considered in the postoperative differential, and literature addressing SPTS after TKA remains sparse. In contrast, Fabella syndrome has been more frequently cited in the TKA literature as a cause of posterolateral pain or neuropathic symptoms, particularly due to mechanical impingement against the prosthesis or compression of the common peroneal nerve [1,8-10]. Consequently, many reported cases of lateral knee pain after TKA focus on fabella excision as the primary treatment strategy [9,11]. However, the presence of fabella does not inherently confirm it as the primary pain generator, especially in patients with concurrent or dynamic snapping or mechanical symptoms. This lack of specificity demonstrates why diagnostic dynamic ultrasounds can provide significant clinical utility in determining the origin of the snapping. In our case, it was clearly documented that the popliteus, not the fabella, was the source of the patient’s snapping. The lidocaine injection into the popliteus tendon sheath alleviated the patient’s pain confirming the popliteus tendon as the source. Our case uniquely demonstrates that arthroscopic popliteal tenotomy alone was sufficient to resolve all symptoms, despite the continued presence of the fabella.
This also confirmed that the popliteus tendon was the dominant driver of pain and snapping in this patient. The fabella, although potentially contributing to discomfort, did not require resection, challenging the assumption that fabella excision is always necessary in such cases. Furthermore, this case underscores the therapeutic and diagnostic value in both ultrasonography with tendon sheath injection and arthroscopy in assessing dynamic lateral knee pain and mechanical symptoms. As Ryu et al [5]. and Finsterwald et al [8]. have shown, all-arthroscopic management of SPTS is feasible and effective given appropriate consideration of popliteal tendon impingement. Our patient represents a novel instance of this technique being applied successfully in the context of TKA, where surgical anatomy and implant positioning can complicate both diagnosis and treatment. Overall, this report adds to the growing recognition of SPTS as an important, but often overlooked, source of post-TKA lateral knee pain and snapping. It emphasizes the need for widespread adoption of dynamic assessment such as ultrasonography with tendon sheath injection and selective intervention including arthroscopic tenotomy, rather than reflexive fabella excision. Early identification and targeted arthroscopic tenotomy may offer a durable, low morbidity solution for appropriately selected patients.
Conclusion
This case highlights the importance of a thorough diagnostic approach to evaluate rare complications such as SPTS after TKA. Further, it demonstrates the application of a dynamic ultrasound with guided injection as a confirmatory test for dynamic tendon pathology. Isolated arthroscopic popliteus tenotomy offers a minimally invasive, anatomy-preserving treatment for SPTS postTKA and does not lead to rotatory instability of the components.
References
- Su S, Lu Y, Chen Y, Li Z (2019) A symptomatic cyamella in the popliteus tendon causing snapping knee: a case report and literature review. BMC Musculoskelet Disord 20: 495.
- Shukla DR, Levy BA, Kuzma SA, Stuart MJ (2014) Snapping popliteus tendon within an osteochondritis dissecans lesion: an unusual case of lateral knee pain. Am J Orthop (Belle Mead NJ) 43: E210-E213.
- Hancioglu S, Bilgin E (2022) A rare cause of lateral snapping knee in a 14-year-old female patient: popliteus tendon. Acta Chir Orthop Traumatol Cech 89: 230-233.
- Krause DA, Stuart MJ (2008) Snapping popliteus tendon in a 21-yearold female. J Orthop Sports Phys Ther 38: 191-195.
- Ryu JH, Lee SW, Lee DH (2022) An all-arthroscopic surgery technique for snapping popliteal tendon syndrome: a case report and literature review. Medicine (Baltimore) 101: e31347.
- Mariani PP, Mauro CS, Margheritini F (2005) Arthroscopic diagnosis of the snapping popliteus tendon. Arthroscopy 21: 888-892.
- Crites BM, Lohnes J, Garrett WE (1998) Jr. Snapping popliteal tendon as a source of lateral knee pain. Scand J Med Sci Sports 8: 243-244.
- Finsterwald MA, Lu V, Andronic O, Prosser GH, Yates PJ, et al. (2023) Popliteal tendon impingement as a cause of pain following total knee arthroplasty: a systematic review. Arthroplasty 5: 45.
- Lai G, Zhuang Z, Yuan G, Sun Y, Cao J, et al. (2025) All-arthroscopic resection of fabella syndrome following total knee arthroplasty: a case report and literature review. BMC Musculoskelet Disord 26: 162.
- Kimura T, Tanikawa H, Hasegawa T (2019) Late onset of the fabella syndrome after total knee arthroplasty. Case Rep Orthop 2019: 5219237.
- Diaz CC, Agarwalla A, Forsythe B (2021) Fabella syndrome and common peroneal neuropathy following total knee arthroplasty. Case Rep Orthop 2021: 7621844.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.