Are Flexible Ureteroscopes (FURS) Equivalent in Deflection when an Anatomical Deformation is Applied? an Ex Vivo Comparative Study of 10 FURS
by Rawad Abou Zahr1,2, Bogdan Buhas1, Jean Baptiste Beauval1, Guillaume Ploussard1, Ambroise Salin1, Christophe Almeras1*
1Department of Urology UROSUD, La Croix du Sud Hospital, Quint Fonsegrives, France
2Department of Urology, Sainte Anne Saint Rémi Hospital, CHIREC group, Brussels, Belgium
*Corresponding author: Christophe Almeras, Department of Urology UROSUD, La Croix du Sud Hospital, Quint Fonsegrives, France
Received Date: 09 July 2025
Accepted Date: 14 July 2025
Published Date: 16 July 2025
Citation: Zahr RA , Buhas B, Beauval JB, Ploussard G, Salin A, et al. (2025) Are Flexible Ureteroscopes (FURS) Equivalent in Deflection when an Anatomical Deformation is Applied? an Ex Vivo Comparative Study of 10 FURS. J Surg 10: 11382 https://doi.org/10.29011/2575-9760.011382
Abstract
Background/Objectives: Flexible Ureteroscopy (FURS) has become indispensable in endoscopic urological practice. The aim of the study was to determine if FURS were equivalent in terms of deflection when put in anatomical conditions.
Methods : A comparative ex vivo study was conducted on 10 different flexible ureteroscopes. Deflection was assessed both before and after the introduction of a 272 μm laser fiber and a 1.5 Fr Nitinol stone basket. Measurements were taken under manufacturer settings and under reproduced anatomical constraints, applied using a 12–14 Fr Access Sheath (AS), respecting a ratio FURS/ AS<0,75. Deflection angles were measured using AutoCAD 2022©. Additional parameters recorded for comparison included handle weight, working (mobile) length, circular diameter, deflection height at 180°, tip-to-shaft distance at full deflection, and maximum reach from the deflection point.
Results: The FURS tested were not equivalent in terms of deflection under reproduced anatomical constraints. A significant deflection loss was found between the FURS tested with a range of +11°/-75° that can be affected by the insertion of a device (basket/ laser fiber) into the working channel. According to the endoscopes employed, we observed two different bending shapes (round or deported) with very heterogenous characteristics that may change the ability to reach calyceal locations, particularly the more complex ones.
Conclusions: This study demonstrates significant variability in deflection stability and quality, particularly under anatomical constraints. These differences are critical considerations for preoperative device selection to optimize procedural success and also evaluate the reliability of the new devices that are appearing on the market.
Keywords: Anatomical Conditions; Bending; Comparative; Deflection; Flexible Ureteroscopy; Urinary Stones
Abbreviations: FURS: Flexible Ureteroscopy; AS: Access Sheath; ESWL: Extracorporeal Shockwave Lithotripsy; PCNL: Per Cutaneaous nephrolithotomy; SuFURS: Single Use FURS; ReFURS: Reusablefurs; RAC: Reproduced Anatomical Constraints
Introduction
Urolithiasis is one of the most frequent pathologies affecting the urinary tract. Incidence of urinary stones is constantly increasing in industrialized countries and their prevalence in France and is estimated at 10% in the general population. Renal colic represents 1 to 2% of the reasons for consultation in emergency departments [1]. The treatment of urinary stones is based on parameters such as number, size (and nowadays volume), composition, and location [2]. Owing to its stone-free rates reaching up to 90% [3,4], its minimally invasive nature and the thriving technical improvements of the devices (LASERs, baskets, access sheathes, vision quality [5,6], miniaturization, suction), Flexible Retrograde Ureteroscopy (FURS) is seeing a steady increase in its clinical indications in the treatment of renal stones to the detriment of other techniques (ESWL, PCNL) and despite a primary higher cost [7,8] that could be nevertheless balanced by its cost effectiveness [9]. Ureteroscopes, whether reusable or single-use are commercialized based on their vision quality as well as their deflection ability. The commercial information given by the companies concerning each ureteroscope is measured in straight industrial conditions. The introduction of a LASER fiber or a basket in the working channel alters the bending quality of FURS [10-13] and a deflection loss may also be observed during difficult procedures with deformation of the shaft [14] secondary to sharp angles. The aim of our study was to compare the deflection angles of various commercially available ureteroscopes and to quantify the deflection loss following the introduction of a laser fiber and a stone basket, both under standard manufacturer conditions and simulated anatomical constraints. The secondary endpoint was to compare the industrial characteristics (tip-shaft caliber, working channel, handle weight). This information is essential for endourologists to make informed decisions when selecting a flexible ureteroscope (FURS), taking into account both economic and operative factors [15]. It is particularly relevant given the increased risk of treatment failure in cases involving complex lower pole anatomy (such as a steep infundibulopelvic angle (<30°), a long (>30 mm) or narrow (<5 mm) infundibulum [16,17]) as well as in anatomically challenging scenarios like horseshoe kidney, pelvic kidney, or urinary diversions.
Materials and Methods
Eight single use FURS (suFURS) and 2 reusable FURS (reFURS) were tested and compared ex vivo (Table 1). All the devices were brand new. Deflection for each ureteroscope was measured both before and after the introduction of a 272 μm laser fiber (Rocamed©) and a 1.5 Fr Nitinol stone basket (Stonewrapper©, Asept InMed), under both the manufacturer’s standard (straight) conditions and Reproduced Anatomical Constraints (RAC).
RAC were simulated on a resin platform by applying targeted curvatures-mimicking the typical angulation and torsion of the human ureter-using controlled bends on a 12–14 Fr Coloplast© access sheath, respecting an endoscope/access sheath ratio < 0,75 according to Fang’s publication [18].

Figure 1: Ex vivo simulation model of anatomical constraints
Pictures were taken in each different situation from the same angle on graph paper. The pictures were then integrated in AutoCad 2022©, which is a program used to create and design precise 2D and 3D models in architectural design. The deflection angles were then measured, and deflection loss was calculated based on the initial deflection measured in industrial or RAC. The measures were taken twice in each different condition to limit a bias of evaluation and a third measure was taken in case of unequal results.Other parameters measured for comparison were handle weight, Mobile Length (ML), Circular Diameter (CD), height at 180° of deflection (H180), tip-shaft distance in full deflection (T-SD) and Maximum Reach from Deflection Point (MR) (Figure 2). The measures of the mobile part of the ureteroscope (ML, CD, H180, T-SD and MR) represent the ability of reaching extreme low locations and acute angles in an active way.
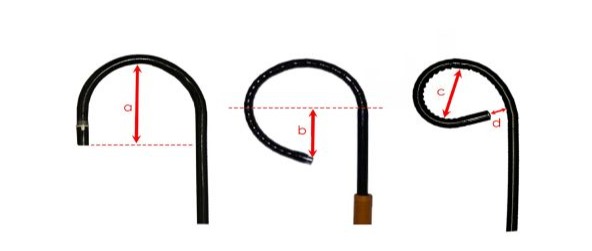
Figure 2: The different parameters measured of the mobile part of FURS.
a. Height at 180° vision; b. maximum reach from deflection point; c. circular diameter; d. Tip-shaft in full deflection
Results
Findings and measurements are presented in Table 1.
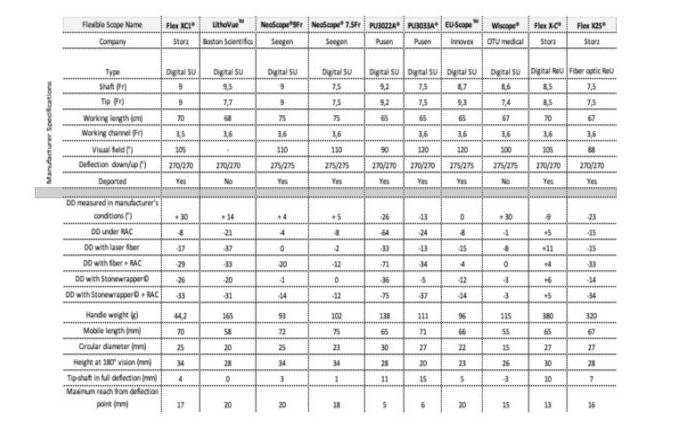
Table 1: Characteristics of 8 single use and 2 reusable uretero-renoscopes.
URS: uretero-renoscope; SU: single use; ReU: reusable; DD: Deflexion difference in comparison with déflection in manufacturer’s conditions ; RAC: roproduced anatomic constraints
An illustration of loss in deflection when a laser fiber and a stone basket is introduced is shown in our Figure 3.
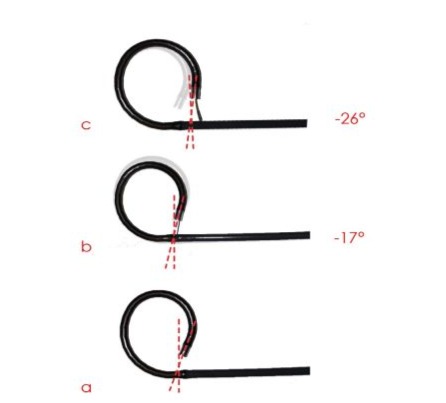
Figure 3: Example of deflection loss.
A.in manufacturer’s conditions; b. upon introducing a laser fiber; c. upon introducing a stone basket Two ureteroscopes had a bend with a round shape instead of a deported deflection bend Figure 4.
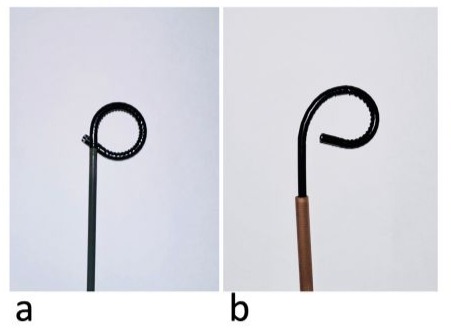
Figure 4: Different bending shapes a: round deflection; b: deported deflection
Primary Endpoint
A loss of deflection was observed when anatomical constraints were applied, which further increased following the insertion of a disposable instrument, such as a laser fiber or stone basket. We observed a substantial variation in deflection loss among the ureteroscopes included in our study, ranging from an increase of 11° to a decrease of 75°.
Secondary Endpoints
We also noted a difference in caliber between the tip and the shaft in two FURS, the Lithoview© and the EU-Scope TM. All the FURS had the same working channel diameter of 3.6 Fr except for the Flex XC1 with a working channel of 3.5 Fr.Regarding other measures that were also compared, we noted a big range in the handle weight from 44g to 380g, and a difference up to 20 mm in Mobile Length (ML), 15 mm in Circular Diameter (CD) (measure (c) in Figure 2), 14 mm in height at 180° (H180) (measure (a) in Figure 2), between -3 and 15 mm of tip-shaft distance (T-SD) (measure (d) in Figure 2) and 15 mm (5-20 mm) in Maximum Reach at Deflection Point (MR) (measure (b) in Figure 2).
Discussion
Flexible ureteroscopes, whether reusable or single-use are commercialized based on their vision and illuminance quality [19,21], on their caliber, but also on their deflection ability. The deflection can be altered by the insertion of a disposable (LASER fiber or basket) in the working channel [10,13] (Figure 3), but also during difficult procedures with the deformation of the shaft [14] secondary to sharp angulation and deflection.In our comprehensive comparative analysis of 10 flexible ureteroscopes, we identified significant variability in deflection and bending characteristics particularly when anatomical constraints were simulated, and that was aggravated when an instrument (laser fiber or a stone basket) was inserted. While image quality, cost, and shaft caliber are often the primary concerns for urologists when selecting a Flexible Ureteroscope (FURS), this study highlights significant differences not only in their ability to maintain deflection but also in the design and features of the shaft’s mobile segment. These factors can greatly influence maneuverability and effectiveness in accessing and treating urinary stones.The measurements depicted in Figure 2 hold relevance within a clinical context: measurement (a) and (b) represent the depth that can be reached with the FURS, while (c) and (d) represent relevant measures in specific circumstances like stones in lateral and particularly medial calyces. Urologists have to get the knowledge of those features before choosing a ureteroscope, and should not only rely on the image quality nor the shaft’s caliber. Our study highlighted the two different bending shapes that are developed: round or deported. As the deported shape seems to be more fit for anatomy, a reverse vision may occur in some devices with excessive deflection on round bending shape (negative d values), that may mislead the urologist’s navigation in the upper tract. With the use of a Holmium laser, an excessive bending with a small curved diameter increases the risk of fiber breakage [22]. It is important to interpret the measurements from our study comprehensively, considering all parameters together to optimize preoperative planning based on factors such as stone location, steep infundibulopelvic angle, or narrow infundibulum. An interesting finding was that reFURS were not inferior in terms of deflection compared to suFURS nor in diameter size where the fiber optic scope Flex X2S® measured 7.5 Fr as well. Surprisingly, our results revealed a significant difference in deflection loss (from 0 to 75° (Table 1) due to the application of anatomical constraints among the different flexible ureteroscopes. The information provided by the manufacturers appears to be insufficient, as it is based solely on measures in straight industrial conditions. This deflection loss may be related to insufficient deflection-holding strength, which could compromise in vivo performance. Maintaining strong deflection ability has become increasingly important due to the trend toward miniaturization, which can sometimes come at the expense of durability, as well as the recent use of flexible and navigable access sheathes with suction that increases resistance on the shaft’s mobile segment [23]. Our study acknowledges several limitations that may impact the findings and conclusions. First it was an ex vivo study without irrigation flow (it could increase the adherence between the endoscope and the access sheath), second the experimental setup designed to simulate anatomical constraints may not fully capture the complexity and variability of human anatomy. The reproducibility of anatomical constraints poses a challenge, as slight variations in the experimental conditions could affect the accuracy of our findings. This study assessed mainly the physical properties of 10 FURS without considering the passive deflection that could occur in-vivo.
However, we can reasonably extrapolate that if a loss of deflection in simulated conditions is observed, it should increase with an additional applied deformation by passive deflection. Additionally, the selection of scopes and focusing on a specific set from available models, may limit the generalizability of our results to all ureteroscopes on the market. Especially with the exponential evolution in the development of suFURS with shafts < 7Fr, and additional channels designed for suction. These limitations underline the necessity for cautious interpretation of the results and suggest the need for further research to validate our conclusions in a broader clinical context.Evaluating the deflection performance of Flexible Ureteroscopes (FURS) and their ability to maintain deflection under anatomical constraints is essential for comparing the various models available on the market. If many studies already assessed the deflection and the impact of a tool (laser fiber/ basket) insertion in the working channel [11,13,19,20,24] , only one highlighted the positive role of a straight shaft on the quality of deflection [14]. This is to date the first study comparing 10 FURS in terms of deflection that reveals a significant disparity in stability and quality of deflection particularly when the shaft of the endoscope is subjected to anatomical constraints.
Conclusions
Technical considerations play a crucial role in the selection and utilization of FURS for the treatment of upper urinary tract stones. This ex vivo comparison of 10 disposable and reusable flexible ureteroscopes demonstrates significant variability in deflection stability and quality, particularly under anatomical constraints. These differences are critical considerations for preoperative device selection to optimize procedural success and also evaluate the reliability of the new devices that are appearing on the market. Patents
Author Contributions: Conceptualization, R Abou Zahr and C Almeras.; methodology, R abou Zahr and C Almeras.; software, R Abou Zahr; validation, JB Beauval, G Ploussard and A Salin; formal analysis, R Abou Zahr and B Buhas.; investigation, R Abou Zahr, B Buhas and C Almeras.; data curation, R Abou Zahr; writing-original draft R. Abou Zahr; writing—review and editing, C.Almeras; visualization, JB Beauval, G Ploussard and A Salin; supervision C Almeras
Funding: This research received no external funding
Institutional Review Board Statement: Not applicable
Informed Consent Statement: Not applicable
Data Availability Statement: The data used to support the findings of this report is included within the article and is owned by the corresponding author.
Acknowledgments: The authors take full responsibility for the content of this publication.
Conflicts of Interest: The authors do not report any conflict of interest.
References
- Daudon M, Haymann J-P, Estrade V (2023) 2022 Recommendations of the AFU Lithiasis Committee: Epidemiology, stone analysis and composition. Prog 33: 737-765.
- Almeras C (2023) Meria P; lithiasis committee of the French Association of Urology (CLAFU). 2022 Recommendations of the AFU Lithiasis Committee: Summary of indications. Prog Urol. 33: 901-910.
- Mager R, Kurosch M, Höfner T (2018) Clinical outcomes and costs of reusable and single-use flexible ureterorenoscopes: a prospective cohort study. Urolithiasis 46: 587-593.
- Geraghty R, Abourmarzouk O, Rai B (2015) Evidence for Ureterorenoscopy and Laser Fragmentation (URSL) for Large Renal Stones in the Modern Era. Curr Urol Rep 16: 54.
- Kam J, Yuminaga Y, Beattie K (2019) Single use versus reusable digital flexible ureteroscopes: A prospective comparative study. Int J Urol Off J Jpn Urol Assoc 26: 999-1005.
- Keller EX, Doizi S, Villa L, Traxer O (2019) Which flexible ureteroscope is the best for upper tract urothelial carcinoma treatment? World J Urol 37: 2325-2333.
- Talso M, Goumas IK, Kamphuis GM (2019) Reusable flexible ureterorenoscopes are more cost-effective than single-use scopes: results of a systematic review from PETRA Uro-group. Transl Androl Urol 8: S418-S425.
- Talyshinskii A, Gauhar V, Castellani D (2024) Single use flexible ureteroscopes: a review of current technologies and cost effectiveness analysis. Curr Opin Urol 34: 110-115.
- Wymer KM, Sharma V, Juvet T, Klett DE, Borah BJ (2021) Costeffectiveness of Retrograde Intrarenal Surgery, Standard and Mini Percutaneous Nephrolithotomy, and Shock Wave Lithotripsy for the Management of 1-2cm Renal Stones. Urology 156: 71-77.
- Tom WR, Wollin DA, Jiang R (2017) Next-Generation Single-Use Ureteroscopes: An In Vitro Comparison. J Endourol 31: 1301-1306.
- Dragos LB, Somani BK, Keller EX (2019) Characteristics of current digital single-use flexible ureteroscopes versus their reusable counterparts: an in-vitro comparative analysis. Transl Androl Urol 8: S359-S370.
- Magheli A, Semins MJ, Allaf ME, Matlaga BR (2012) Critical analysis of the miniaturized stone basket: effect on deflection and flow rate. J Endourol 26: 275-277.
- Teplitsky SL, Leong JY, Calio B (2021) Ergonomics in Endourology: Measurement of Force for Deflection in Contemporary Ureteroscopes. J Endourol 35: 215-220.
- Monga M, Dretler SP, Landman J (2002) Maximizing ureteroscope deflection: “play it straight.” Urology 60: 902-905.
- Geavlete B, Mareș C, Mulțescu R (2022) Hybrid flexible ureteroscopy strategy in the management of renal stones - a narrative review. J Med Life 15: 919-926.
- Karim SS, Hanna L, Geraghty R, Somani BK (2020) Role of pelvicalyceal anatomy in the outcomes of retrograde intrarenal surgery (RIRS) for lower pole stones: outcomes with a systematic review of literature. Urolithiasis 48: 263-270.
- Dragos LB, Somani BK, Sener ET (2017) Which Flexible Ureteroscopes (Digital vs. Fiber-Optic) Can Easily Reach the Difficult Lower Pole Calices and Have Better End-Tip Deflection: In Vitro Study on K-Box. A PETRA Evaluation. J Endourol 31: 630-637.
- Fang L, Xie G, Zheng Z, Liu W, Zhu J (2019) et al The Effect of Ratio of Endoscope-Sheath Diameter on Intrapelvic Pressure During Flexible Ureteroscopic Lasertripsy. J Endourol 33: 132-139.
- Marchini GS, Batagello CA, Monga M (2018) In Vitro Evaluation of Single-Use Digital Flexible Ureteroscopes: A Practical Comparison for a Patient-Centered Approach. J Endourol 32: 184-191.
- Lusch A, Abdelshehid C, Hidas G (2013) In vitro and in vivo comparison of optics and performance of a distal sensor ureteroscope versus a standard fiberoptic ureteroscope. J Endourol 27: 896-902.
- Kwok J-L, De Coninck V, Corrales M (2024) Illumination matters part I: comparative analysis of light sources and illumination in flexible ureteroscopy-fundamental findings from a PEARLS analysis. World J Urol 42: 355.
- Haddad M, Emiliani E, Rouchausse Y (2017) Impact of the Curve Diameter and Laser Settings on Laser Fiber Fracture. J Endourol 31: 918-921.
- Lua A, Tan LRL, Panthier F, Sierra A, Ventimiglia E, Solano C (2024) et al Optimal deflection techniques for flexible and navigable suction ureteral access sheaths (FANS): a comparative in vitro PEARLS analysis. World J Urol 42: 606.
- Monga M, Anderson KJ, Durfee W (2004) Physical properties of flexible ureteroscopes: implications for clinical practice. J Endourol 18: 462-465.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.