Antiplatelet Drug Application in Dental Clinical Practice. Efficacy, Safety, and Guidelines: A Systematic Review
by Gianna Dipalma1, Angelo Michele Inchingolo1, Fabio Piras1, Irma Trilli1, Roberto Vito Giorgio1, Claudio Carone1, Antonio Mancini1, Andrea Palermo2, Alessio Danilo Inchingolo1, Francesco Inchingolo1*
1Department of Interdisciplinary Medicine, University of Bari “Aldo Moro”, 70124 Bari, Italy
2College of Medicine and Dentistry, Birmingham B4 6BN, UK
*Corresponding author: Francesco Inchingolo, Department of Interdisciplinary Medicine, University of Bari “Aldo Moro”, 70124 Bari, Italy
Received Date: 4 May 2024
Accepted Date: 08 May 2024
Published Date: 10 May 2024
Citation: Dipalma G, Inchingolo AM, Piras F, Trilli I, Giorgio RV, et al (2024) Antiplatelet Drug Application in Dental Clinical Practice. Efficacy, Safety, and Guidelines: A Systematic Review. Ann Case Report. 9: 1795. DOI: https://doi.org/10.29011/2574-7754.101795
Abstract
Background: Antiplatelet (APL) therapy (TH) plays a crucial role in preventing thrombotic (TRB) events in patients with cardiovascular diseases. However, its application in dental clinical practice remains a topic of debate due to concerns regarding bleeding (BL) complications during invasive procedures (PRC).
Objective: This systematic review aims to evaluate the efficacy and safety of APL drugs in dental PRCs, assess the risk of BL complications, and examine existing guidelines for managing patients on APL TH.
Methods: A comprehensive search was conducted in PubMed, Scopus and Web of Science for studies published from January 1, 2004 up to January 2024. Eligible studies included randomized controlled trials, observational studies, and guidelines evaluating the use of APL drugs in dental PRCs. Data on efficacy outcomes (e.g., prevention of TRB events), safety outcomes (e.g., BL complications), and adherence to guidelines were extracted and synthesized.
Results: A total of 28 studies were included in the review, comprising randomized controlled trials, observational studies, and clinical guidelines. The findings suggest that discontinuation of APL TH before dental PRCs may increase the risk of TRB events without significantly reducing BL complications. However, the evidence regarding the risk of BL associated with dental PRCs in patients on APL TH is inconclusive. Existing guidelines vary in their recommendations for managing patients on APL TH, highlighting the need for standardized protocols.
Conclusion: APL TH is essential for preventing TRB events in high-risk patients, and its discontinuation before dental PRCs may not be warranted in most cases. However, further research is needed to clarify the risk of BL complications associated with dental PRCs in patients on APL TH and to develop evidence-based guidelines for managing these patients in dental clinical practice. Standardized protocols considering both efficacy and safety outcomes are crucial for ensuring optimal patient care.
Keywords: Antiplatelet; Antithrombotic; Dentistry; Risk of Bleeding; NAO; TAO.
Abbreviations: ACO: anticoagulant; APL: antiplatelet; AS: aspirin; BL: bleeding; EX: extraction; POP: postoperative; PRC: procedure; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PROSPERO: The International Prospective Register of Systematic Reviews; SU: surgery; TH: therapy; TRB: thrombotic; TRT: treatment;
Introduction
Dentistry treats a wide range of oral health issues, from simple cleanings and cavity fillings to more complex PRCs like periodontal surgery (SU) and dental implants [1–3]. The control of BL is an ongoing concern during these interventions, particularly in patients receiving invasive treatments (TRT) or those with systemic disorders. This is the point at which antiaggregants play a very important function [4–8]. Antiaggregants are essential components of TRT strategies for a variety of cardiovascular diseases [9]; these include Aspirin (AS) (acetylsalicylic acid), Ticagrelor, and Clopidogrel, which are often recommended drugs [10–14]. Their primary function is to prevent platelets clumping together, which keeps blood clots from forming and causing TRB events including strokes and heart attacks [15–18]. However, the implications of APL TH extend beyond the cardiovascular system, impacting dental practice in significant ways. These drugs work in a variety of ways, frequently by going after important enzymes or receptors involved in platelet activation and aggregation as shown in the figure 1 [19–22]. For example, AS irreversibly acetylates the active site of COX enzymes, particularly COX-1 and COX-2, inhibiting their activity. COX enzymes are responsible for converting arachidonic acid into prostaglandin H2 (PGH2), a precursor molecule in the synthesis of various prostanoids, including prostaglandins and thromboxane A2 (TxA2), a powerful platelet aggregator. So, by inhibiting COX, AS disrupts the synthesis of prostaglandins involved in inflammation, pain perception, fever regulation, and platelet aggregation [23–26]. Similarly, medications such as Ticagrelor and Clopidogrel interfere with ADP-mediated platelet activation by targeting ADP receptors on platelets[27–31]. More in details, Ticagrelor works by reversibly blocking a specific receptor on platelets called P2Y12, thereby preventing platelets from clumping together and forming clots in the blood vessels [32–34], while Clopidogrel is a prodrug that requires metabolic activation in the liver to produce its active form, which then irreversibly blocks the P2Y12 receptor [35]. Anyway, antiaggregants lessen the chance of clot formation by interfering with these pathways, which is an important factor to take into account during dental operations where BL management is critical [36–39]. Another important point to underline it’s represented by the two different types of available antiaggregations such as monoTH and double antiaggregation. The first consists of the administration of a single APL drug, mainly AS, but also ticlopidine or clopidogrel. This regimen is generally used in primary prevention and secondary prevention [40–42]. In the second case, there is the simultaneous administration of two APL drugs, generally AS + Clopidogrel, or AS + Ticlopidine, to prevent early thrombosis of coronary stents after their implantation for the entire period necessary for their endothelialization (for the first month after bare metal stent, for the first 12 months after drug-eluting stent [43].
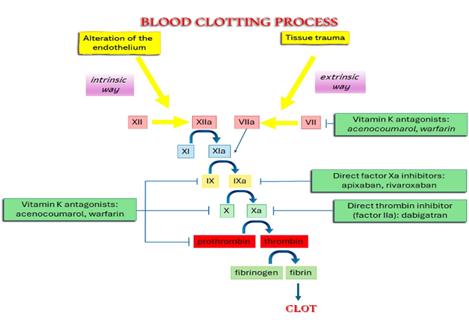
Figure 1: Blood clotting process.
In the context of dentistry, the use of antiaggregants carries significant implications for patient care [35,44]. For examples, patients on APL TH for conditions as coronary artery disease, atrial fibrillation, or those who have undergone cardiac stent placement, may present unique challenges during dental interventions due to their increased susceptibility to BL [45–47]. Consequently, dental practitioners must adopt strategies to minimize BL while ensuring optimal TRT outcomes [48–51]. Prior of a dental PRC, dentists should assess patients' medication history and consult with their physicians to determine whether APL TH should be modified or temporarily discontinued before invasive dental PRCs to reduce the risk of BL complications [52–54]. During dental PRCs, if patients is on APL TH, dentists may employ local hemostatic measures, such as local pressure and hemostatic agents, to minimize BL during the TRTs and elective dental PRCs should be scheduled at times when platelet function (Figure 2) is likely to be at its lowest, such as in the morning [55]. In postoperative (POP) setting, dentists should provide appropriate instructions, including advice on maintaining good oral hygiene and avoiding trauma to the surgical site to reduce the risk of BL complications. Furthermore, patients may also be instructed to resume their APL TH as soon as possible after the PRC [56].
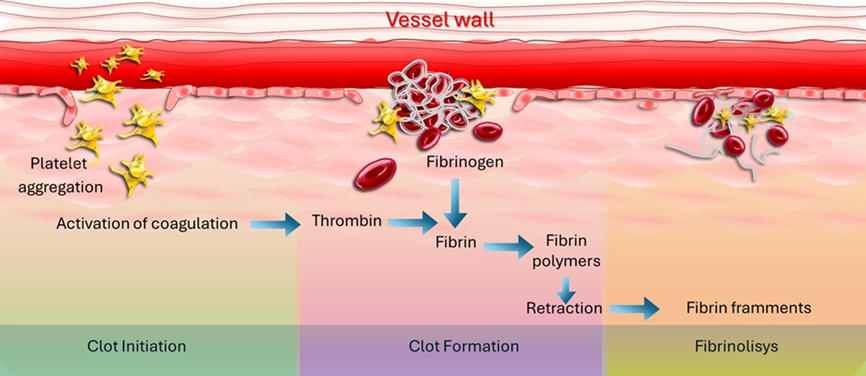
Figure 2: Clot initiation to fibrinolisys.
In this review we discuss the most update knowledge’s regarding the clinical use of antiaggregants in dentistry, focusing on the guidelines of best clinical practice together with detailed information about the data published in literature. Finally we try to hypothesize future improvements to reduce the actual risks still present in dental medicine.
Materials and Methods
Protocol and Registration
This review was carried out in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, and it was registered under the number CRD42024543233 on PROSPERO (The International Prospective Register of Systematic Reviews) [57].
Search Processing
We limited our search to English-language papers published between January 1, 2004, and April 12, 2024, in PubMed, Scopus and Web of Science that were relevant to our topic. In the search approach, the Boolean keywords "antiplatelet AND dentistry" were used. We selected these phrases because they most accurately reflected our investigation's aim, which was to gain additional insight into the interaction between APL drugs and dentistry TH (Table 1).
|
Articles screening strategy |
KEYWORDS: “A”: antiplatelet; “B”:antithrombotic; “C”: oral surg*; “D”: tooth; “E”: dent* |
|
Boolean Indicators: “A” AND “C”; “A” AND “D”; “A” AND “E”; “B” AND “C”; “B” AND “D”; “B” AND “E” |
|
|
Timespan: January 1, 2004, to April 12, 2024 |
|
|
Electronic databases: Pubmed; Scopus; Web of Science. |
Table 1: Indicators for database searches.
Inclusion Criteria
Three reviewers evaluated all relevant papers based on the following chosen criteria: (1) solely human subjects studies; (2) complete text; and (3) scientific studies evaluating the management of APL drugs during clinical dental practices. The following process was used to construct the PICO model:
• Criteria: Application in the present study;
• Population: Human subjects;
• Intervention: dentistry TRT;
• Comparison: Control group; anticoagulant (ACO) group; heparin group; local hemostatic agents;
• Outcome: Evaluation of antiplatelet drugs during dentistry TRT;
• Study design: Clinical Trials.
Exclusion Criteria
Articles written in languages other than English, ineligible study designs, ineligible outcome measures, ineligible populations, case studies, reviews, and animal studies were among the exclusion criteria.
Data Processing
Author disagreements on the choice of articles were addressed and settled.
Article Identification PRC
The appropriateness evaluation was done independently by two reviewers, F.I. and F.P. An additional manual search was conducted to increase the number of articles available for full-text analysis. English-language articles that met the inclusion criteria were taken into consideration, and duplicates and items that didn't qualify were marked with the reason they weren't included.
Study Evaluation
The article data were independently evaluated by the reviewers using a special electronic form designed according to the following categories: authors, year of study, aim of the study, materials and methods, and results.
Quality Assessment
Two reviewers, F.P. and P.A., evaluated the included papers' quality using the ROBINS-I tool. In order to evaluate the possibility of bias in the outcomes of non-randomized trials comparing the health impacts of two or more therapies, ROBINS-I was created. Each of the seven evaluated points was given a bias degree. F.I., the third reviewer, was consulted in case of disagreement until a consensus was reached. The reviewers were instructed on how to use the ROBINS-I tool and adhered to the guidelines in order to assess the potential for bias in seven different domains: confounding, participant selection, intervention classification, deviations from intended interventions, missing data, outcome measurement, and choice of reported results. Discussion and consensus were used to settle any differences or conflicts amongst reviewers in order to improve the assessments' objectivity and uniformity. In situations when agreement could not be reached, the final decision was made by a third reviewer. An extensive assessment of potential biases in the non-randomized studies included in this study was made possible by the use of ROBINS-E for bias assessment. It contributed to the overall evaluation of the caliber and dependability of the results by pointing out the evidence base's advantages and disadvantages. The writers of this review were able to reach more informed interpretations and conclusions based on the facts at hand by taking the risk of bias into account.
Results
A total of 161 papers were obtained from the databases Web of Science (83), PubMed (382), and Scopus (158). This resulted in 419 articles after eliminating duplicates (204). 315 entries were eliminated after their titles and abstracts were examined. The writers were able to successfully obtain the remaining 104 papers and confirm their eligibility. 79 items were eliminated as a result of this process because they were off topic. The qualitative analysis of the 25 final articles is included in this study (Figure 3). Each study's findings were presented in Table 2.
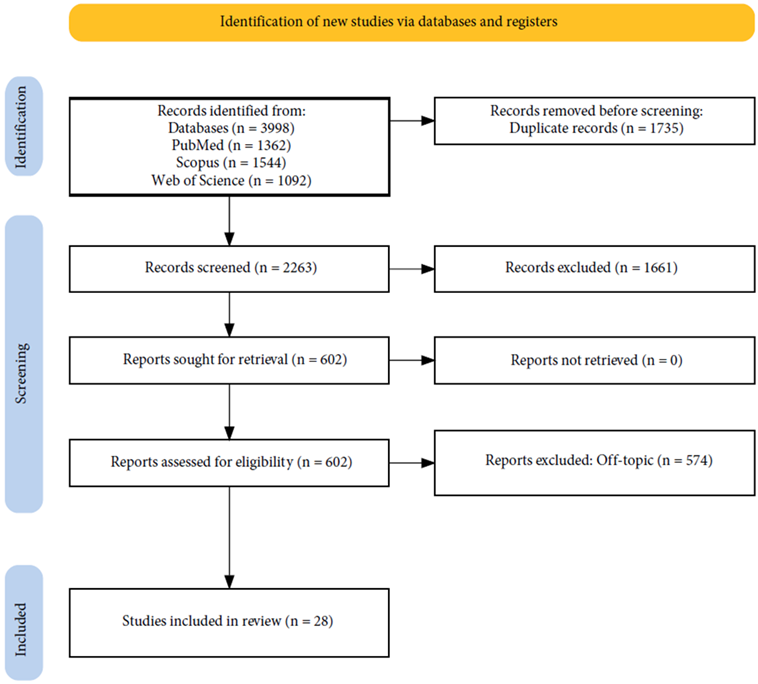
Figure 3: PRISMA flowchart of the literature search and article inclusion process.
|
Authors and years |
Type of the study |
Aim of the study |
Material and methods |
Results |
|
Sunu et al, 2021 [58] |
Observational study |
To evaluate the BL pattern after routine dental extraction (EX) among patients on low dose long term AS TH. |
The study included 104 subjects aged 30-65 who continued AS intake during EX. Dental EX was performed under local anaesthesia without stopping AS TH. |
87% of patients experienced mild BL (<20 ml) and 13% had moderate BL (20-30 ml). The mean blood loss for the total population was 16.15 ± 3.5 ml. |
|
Buchbender et al, 2021 [60] |
Prospective cohort study |
To investigate the occurrence and severity of POP BL following dentoalveolar SU in patients with uninterrupted ACO TH (AT). |
Patients receiving AT (vitamin K antagonist (VK), direct oral ACOs (DOAC), or APL TH (APT)) and undergoing surgical interventions (classified as A, B, or C) were studied between 2019 and 2021. A control group of healthy, non-anticoagulated individuals (CG) was included. |
The study included 195 patients, with 95 in the AT group and 100 in the CG. POP BL was significantly higher in the AT group compared to the CG (p = 0.000), with a significant correlation with surgical intervention class C (p = 0.013) and severity class 1a BL (p = 0.044). |
|
Eapen et al, 2017 [62] |
Comparative study |
To evaluate POP BL in patients on low-dose AS TH by comparing two groups: one with withdrawal and the other without withdrawal of AS regimen before dental EX. |
The study included 80 patients on low-dose AS TH, divided into two groups of 40 each. Group I (control) stopped AS 5 days before EX, while Group II (test) continued AS TH. Data were analysed using the independent t-test with 80% power. |
The mean pre-operative BL time was significantly different between the control (87.75 s) and test (95.75 s) groups (p < 0.05). Similarly, the mean pre-operative clotting time was significantly different between the control (228.63 s) and test (246.25 s) groups (p < 0.05). |
|
Lewandowski et al, 2021 [44] |
Retrospective cohort study |
To assess the effectiveness of TachoSil fibrin-collagen patches in stopping and preventing secondary post-EX BL in patients undergoing chronic APL TH. |
Medical records of 153 patients on chronic APL TH undergoing tooth EX were retrospectively examined. The largest group comprised 74 patients using AS and clopidogrel as dual APL TH. TachoSil fibrin-collagen patches and stitches were applied to all EX wounds. |
Primary BL was successfully stopped in all patients within 20-30 minutes post-EX. Secondary BL occurred in 4.9% of patients, which was managed by applying pressure dressings soaked in tranexamic acid. Secondary BL occurred on the second- or third-day post-EX in eight cases. |
|
Kaura et al, 2022 [98] |
Comparative observational study |
To assess the risk of BL in patients on single and dual APL TH undergoing dental implants. |
65 patients undergoing dental implant placement were divided into two groups: Group I (48 patients) on single APL (AS) and Group II (17 patients) on dual APL (AS and Clopidogrel). BL was evaluated intra-operatively and POPly. |
Significant differences in BL severity, assessed using the Visual Analog Scale (VAS), were noted between Group I and Group II both intra-operatively (P = 0.000) and POPly within 24 hours (P = 0.004). However, POP complications after 24 hours were non-significant (P = 0.277). |
|
Hoda et al, 2021 [104] |
Observational study |
To establish a protocol for dental EXs in patients on APL TH (APT) by assessing BL outcomes. |
100 patients undergoing dental EX were assessed after obtaining detailed case histories. Preoperative BL time was evaluated, and patients with normal BL time underwent SU under local anaesthesia. Local haemostatic measures were employed post-EX. |
In patients on mono APL TH, BL occurred in 16 patients after 1 hour but ceased by 24-48 hours (q = 32, P < 0.001). For patients on dual APL TH, BL occurred in 10 patients after 1 hour and in 1 patient after 24 hours, with no BL at 48 hours (q = 16.545, P < 0.001). |
|
Martinez-Moreno et al, 2021 |
Retrospective clinical study |
To evaluate BL complications in anticoagulated and APL-treated patients following simple dental EXs over a 4-year period. |
The study analysed 147 clinical records of patients undergoing simple dental EXs from October 2015 to September 2019. Of these, 63 patients were on APL TH, 83 were anticoagulated, and 1 patient was on both. Within the anticoagulated group, 70 patients took classic ACOs, and 14 took new oral ACOs (NOACs). |
Among 418 dental EXs, five severe BL complications occurred in three patients (2.11%). Four complications were in patients treated with NOACs (1.68%), and one occurred in a patient anticoagulated with acenocoumarol (0.42%; p = 0.003). |
|
Babaji and Rishal, 2017 [86] |
Comparative observational study |
To evaluate the necessity of discontinuing dual APL TH in patients undergoing dental EXs. |
150 patients scheduled for dental EX were divided into two groups: Group I (75 patients) on dual APL TH and Group II (75 patients) who discontinued APL TH one week before EX. BL time (BT) was recorded before EX. |
No active BL was observed in either group at 1 hour or 24 hours POPly. After 24 hours, no BL was reported in 73 patients in Group I and 78 patients in Group II. |
|
Tanimoto et al, 2022 |
Retrospective cohort study |
To evaluate the outcomes of tooth EX in older adult patients undergoing antiTRB TH and establish evidence-based approaches for such PRCs according to relevant guidelines. |
The study included 165 patients (184 cases) receiving antiTRB TH undergoing outpatient tooth EX. Medical records were analysed to gather data on patient demographics, clinical characteristics, and EX PRC details. |
Warfarin was used in 25 patients (26 cases), direct oral ACOs (DOACs) in 26 patients (33 cases), and APL drugs in 91 patients (101 cases). Dual APL TH with concomitant ACOs was administered to 15 patients (16 cases), and drug TH was suspended in five cases. |
|
Sadhasivam et al, 2016 [66] |
Prospective cohort study |
To evaluate the risk of significant BL following dental EXs and assess the necessity of discontinuing APL TH. |
Three hundred patients requiring dental EX were included, with 200 patients on APL TH. Patients were divided into three groups: Group 1 continued APL TH, Group 2 had TH interrupted, and Group 3 comprised healthy patients not on APL TH. Pre-operative BL and clotting times were determined. |
The mean BL time in Groups 1, 2, and 3 was 1 minute and 32 seconds, 1 minute and 25 seconds, and 1 minute and 27 seconds, respectively. Prolonged immediate post-EX BL occurred in 9% of Group 1 and 15% of Group 2, with none in Group 3. BL after 1 hour was present in 9% of Group 2, controlled with gelatine sponge. |
|
Shahzad et al, 2021 [141] |
Comparative observational study |
To compare POP BL in tooth EX with and without stopping APL drugs. |
Patients were divided into two groups: Group A, tooth EX without discontinuation of APL TH, and Group B, tooth EX with discontinuation of APL TH with consent from treating physician/cardiologist. |
Group A had a mean age of 55.08 years, and Group B had a mean age of 52.92 years. After 1-hour, active BL was 12% in Group A and 6% in Group B (non-significant, p=0.271). After 24 hours, there was no BL in 42% of Group A and 58% of Group B, with oozing in 34% of Group A and 26% of Group B, and active BL in 24% of Group A and 16% of Group B (non-significant, p=0.271). |
|
Sanchez-Palomino et al, 2015 |
Prospective observational study |
To evaluate the efficacy of a protocol for performing dental EXs in patients receiving dual APL TH. |
Thirty-two patients undergoing dental EXs were included. Variables evaluated included collagen-epinephrine fraction, collagen-adenosine diphosphate fraction, surgical surface, post-surgical measures, and adverse effects. Alveolar sutures and gauzes impregnated with tranexamic acid were applied as post-surgical measures. |
Collagen/epinephrine fraction was 264.53±55.624 seconds and collagen/ADP fraction was 119.41±44.216 seconds, both higher than normal. No patients experienced POP BL, hematoma, or infection due to the post-surgical measures. |
|
Gupta et al, 2018 [127] |
Prospective comparative study |
To study the effects of low-dose AS on BL after dental EXs, compare perioperative blood loss between patients on AS TH and healthy patients, and discuss measures for controlling POP BL. |
The study included 100 patients aged 30 to 60 years, divided into a test group (50 patients on daily low-dose AS) and a control group (50 patients not on APL TH). All EX PRCs were performed on an outpatient basis under local anaesthesia. |
Intraoperative blood loss was similar in both groups, and there was no excessive POP BL. Only a few patients in each group required haemostatic measures, with slightly more needed in the test group. |
|
Kumar et al, 2021 [79] |
Prospective cross-sectional study |
To assess the risk of BL in patients continuing APL medication during minor oral surgical PRCs such as tooth EX, third molar EX, biopsy, and alveoloplasty. |
The study evaluated haemostasis steps, time to arrest BL, and correlation between these factors in patients on APL TH (Group A: AS, Group B: AS and clopidogrel) and healthy patients (Group C). |
Level 1 haemostatic measures were required for 64.5% of patients, Level 2 for 34.0%, and Level 3 for 1.5%. Statistically significant differences were found between groups in terms of local haemostatic measures (P ≤ 0.001). |
|
Y. Brancaccio et al, 2020 |
Randomized clinical trial |
This study aimed to evaluate the clinic efficacy of four local haemostatics in patients undergoing oral APL TH after multiple dental EXs without drug interaction. |
The study involved 102 patients with oral APL agents requiring multiple dental extrusions. After SU, the alveoli were casually systolic with a single suture, haemostatic tappet (HEM), advanced platelets fibrin (A-PRF+), and leucocytes fibrin (L-PRF). Primary issues included POP blood flow, wound coverage index, and potential complications. |
Both A-PRF+ and L-PRF have shown reduced blood pressure compared to the single suture, while only L-PRF has shown reduced full-body vigilance compared to the control site. |
|
S. Cakarer et al, 2013 |
Randomized clinical trial |
This study was designed to assess the effects of the alternative haemostatic agent, ABS, on blood pressure following dental splints. |
The study comprised 25 individuals who needed teeth EXs as a component of anti-TRB TH. Two groups were created out of them: one took ABS, and the other served as a control. |
Patients receiving anti-TRB TH and having an INR of 4.0 appear to benefit from the ABS as a haemostatic agent because it considerably reduces BL during intervention. |
|
Y. Morimoto et al, 2009 [73] |
Retrospective study |
The management of oral TH patients is viewed retrospectively as part of their haemostatic TRT. |
155 periodontics PRCs have been performed on 139 patients, who have gone on to take conventional anti-TRB medications. Compression, suture, and insertion of oxidized cellulose are used as local haemostatic measures. When haemostasis was difficult, stick and/or electrocauterization were used to stop the BL. |
The ablation can be performed safely in patients on warfarin TH (INR <4,0) and/or APL TH. When the patient has an INR below 3.0, dental SU can be performed with appropriate local anaesthesia. |
|
A. Canigral et al, 2010 |
Prospective observational study |
This study investigates how BL appears after routine dental SU, assesses how anti-TRB drugs affect BL risk, and verifies the validity of a clinical BL assessment method. |
Nearly one-third of the 99 patients in the research suffered BL, indicating the necessity for haemostatic TH. The Multiplate System® was used to evaluate BL symptoms in the patients. |
For elderly patients, the safety of oral SU is improved when APL TH—specifically, acetylsalicylic acid and clopidogrel—is combined with platelet function testing. |
|
Shin-Yu Lu et al, 2018 |
Randomized clinical trial |
This study aimed to examine management of dental EX in patients on warfarin and APL TH. |
In the research involving 1331 patients, the effectiveness of warfarin, APL medication, type of tooth EX, and incidence of POP BL were compared between patients receiving APL TH, warfarin, and a control group. |
In the warfarin’s group, POP BL was unrelated to INR or type of tooth EX and was higher than in the APL and control groups. Gel-foam impregnated with tranexamic acid powder was effective in managing BL. |
|
A. Shenoy et al, 2021 |
Prospective study |
The aim of this study is to compare the blood loss that occurs after a single tooth EX in patients who stop their medication and in those who continue their APL TH during the perioperative period. |
Eighty-five of the 170 patients receiving APL TRT remained in the perioperative phase after being split into two groups. Under local anaesthetic, a single tooth was extracted, and the gauze dough was left in place for sixty minutes. |
There are no statistically significant differences in post-stroke blood counts between patients who stopped taking APL TH and those who continued it. |
|
J. Sui et al, 2014 |
Retrospective study |
This study attempted to assess the morbid and thromboembolic risks of patients following AVK and/or AAP TRT while taking the operatorial management perspective into consideration. |
Retrospective analysis was done on the dossiers, which included information on POP problems, pre-operative INR, anti-TRB TH type and adjustments, and epidemiological data. |
INR, avulsions, and recurrence of thromboembolic events decreased in 37 patients under AVK, 41 under AAP, 10 with bi-TH AAP, and 5 under AVK-AAP, according to the study. |
|
Y. Morimoto et al, 2009 |
Observational study |
The study looked at the risk factors that affect patients using oral anti-TRB medication following tooth EXs in terms of when POP BL starts. |
382 patients underwent a total of 443 tooth EXs, all while receiving standard anti-TRB medication and using local haemostatic agents. |
With a median duration of 3 days, 94.1% of 17 patients experienced POP BL. 80% of patients receiving warfarin medication needed extensive local haemostatic measures, whereas patients receiving APL TH only needed compression to achieve haemostasis. |
|
J. Huang et al, 2022 |
Retrospective case-control study |
The purpose of this study was to investigate blood loss rates and risk variables for blood loss in individuals receiving anti-TRB medication following tooth EXs. |
Patients who received oral anti-TRB medications were included in the trial, and local haemostatic measurements and ECG monitoring were used during dent EXs. Both univariate and multivariate analyses were used to assess risk variables for POP morbidity. |
The study discovered a substantial difference between the two groups: 27 patients who used anti-TRB medicines and 9 patients who did not; age and the number of extracts teeth were significant risk factors for post-EX blood loss. |
|
S. Ohba et al, 2014 |
Randomized clinical trial |
The purpose of this study was to develop a regimen for patients undergoing minor oral SU and anti-TRB medication, as well as to identify risk factors for POP morbidity. |
A total of 102 patients were involved, who were then subjected to 142 minor oral surgical interventions while receiving anti-TRB TH. |
POP morbidity was substantially correlated with the length of active partial activated TH (APTT), particularly in patients receiving warfarin alone or in conjunction with an APL medication. |
|
T. Hasegawua et al, 2017 |
Retrospective study |
The purpose of this study was to investigate the multivariate associations between morbidity and POP risk variables in patients receiving oral anti-TRB TRT. |
With a median age of 72.2 ± 11.7 years, the study included 122 male and 118 female patients who had traditional anti thrombectomy TH. Preoperative blood tests, the use of preoperative antibiotics or not, FANS supplements, the total number of extracted teeth, and the kind of surgical TRT were additional variables. |
POP haemorrhage was substantially correlated with preoperative antibiotic administration, elevated international normalized prothrombin time (PT-INR), and greater tooth EX. |
|
R. Pippi et al, 2021 |
Prospective study |
The study is to examine the efficacy of local hemo-TH protocols, blood flow incidence, and safety index in addition to identifying variables associated with surgical operations, patients, and anti-TRB TRTs as indicators of blood flow. |
Patients with dentitional extrusions without anti-TRB TRT were studied using Fisher's test to determine the relationship between blood supply and haemostatic material type, using a multivariate logistic regression. |
After 254 PRCs were examined, the incidence of blood clots was 15.75%; only 2.34% of patients had serious blood clots. There was a favourable correlation between the number of tooth quadrants involved and the pre-surgical antibiotic TRTs. |
|
Sang-Hoon Kang et al, 2021 |
Randomized clinical trial |
The present study aimed to assess the risk of BL after tooth EX in patients with thrombocytopenia. |
The study divided patients into groups with platelet counts between 150k and 250k and examined 220 thrombocytopenia patients having tooth EXs. It also compared BL issues that occurred before and after the EX. |
Ninety of the 220 participants in the research had normal platelet counts, whereas 130 had thrombocytopenia. Five patients experienced BL problems, and 7.7% of them had thrombocytopenia. By platelet count, there was no discernible variation in the incidence of post-EX BL across the patient groups. |
|
M. AlSheef et al, 2021 |
Randomized clinical trial |
This study aims to investigate the incidence of POP BL following dental EXs in adult patients taking anti-TRB medication. |
According to a retrospective study conducted in Saudi Arabia on 539 patients between the ages of 18 and 93, those who were BL were treated as outpatients using local haemostatic TRTs. |
In EX sessions, POP BL is uncommon. Patients on warfarin have the highest risk (3.88%), and women, particularly those taking more recent ACO drugs, have the highest rate. |
Table 2: A descriptive item selection summary.
Quality Assessment and Risk of Bias of Included Articles
The risk of bias in the included studies is reported in Figure 4. Regarding the bias due to confounding most studies have a high risk. The bias arising from measurement is a parameter with low risk of bias. Many studies have low risk of bias due to bias in selection of participants. Bias due to post exposure cannot be calculated due to high heterogeneity. The bias due to missing data is low in many studies. Bias arising from measurement of the outcome is low. Bias in the selection of the reported results is high in most studies. The final results show that 14 studies have low risk of bias, 3 have a very high risk of bias and 8 have high risk of bias.
Figure 4: Bias assessment.
Discussion
BL Risk in Dental EX among Patients on Low-Dose AS TH:
The observational study by Sunu et al. set out to investigate the risk of BL during dental EXs in patients taking low-dose AS, a medication often paused pre-SU due to concerns about BL [58]. A cohort of 104 individuals, aged 30-65, who maintained their AS regimen during the EX process, was examined. The amount of POP BL was measured using a combination of weighing gauze pre- and POPly and assessing the total volume of fluid collected in the suction jar [59]. The findings revealed that the majority of patients, constituting 87% of the sample, experienced only mild BL (less than 20 ml), while 13% encountered moderate BL (ranging from 20 to 30 ml). On average, the total blood loss across the entire study population was quantified at 16.15 ml with a standard deviation of 3.5 ml [60]. In conclusion, the study suggests that undergoing routine dental EXs while continuing low-dose AS TH does not significantly increase the risk of post-EX haemorrhage. Thus, it supports the notion that patients can safely maintain their AS intake during such dental PRCs without encountering notable BL complications [61].
The comparative study of Eapen et al. aimed to determine whether low-dose AS TH needs to be discontinued before routine dental EX [62]. Dividing patients into two groups, one withdrawing AS and the other not, the researchers compared POP BL outcomes. They included 80 patients on low-dose AS, with 40 in each group [63]. A single surgeon conducted atraumatic EXs. Analysis showed significant differences in pre-operative BL and clotting times between the groups, but no patients experienced prolonged POP BL except for one in the non-withdrawal group [64]. The study suggests that dental EXs in patients on low-dose AS can be safely performed without stopping the TH, potentially offering a simpler and safer approach to dental PRCs for such patients.
Discontinuation of APL TH increases the risk of TRB complications whereas its continuation is believed to increase the risk of prolonged post-EX BL [65]. The aim of this cohort study by Sadhasivam et al. is to investigate the risk of BL after dental EXs in patients on APL TH [66]. Three hundred patients were included, with 200 on APL TH. They were divided into three groups: those continuing TH, those with interrupted TH, and healthy patients. BL was monitored at various intervals post-EX. Results showed that BL times were similar across groups. Prolonged immediate BL occurred in 9% of Group 1 and 15% of Group 2, with no instances in Group 3. However, BL was manageable in all cases and no significant BL occurred beyond 1-hour post-EX [67]. The study concludes that dental EXs can be safely performed in patients on APL TH, mitigating the risk of thromboembolic events associated with discontinuation of TH.
POP BL Risks in Dental SU Patients on Blood-Thinning Medications:
The prospective cohort study (Buchbender et al.) investigated POP BL risks in dental SU patients taking different blood-thinning medications: direct oral ACOs DOACs, APL, or vitamin K antagonists VKAs [68]. POP BL events were monitored and compared among the different medication groups, it aimed to guide clinicians in managing such patients during dental PRCs [69]. The findings provide insights into minimizing POP BL complications for patients on these medications undergoing dental SU, contributing to safer and more informed TRT decisions.
M. AlSheef's research focuses on the management of patients who take anti-TRB medications during dental EXs [70]. The study examined the risk of emphysema following SU in patients who had continued anti-TRB TH throughout dental EXs. The results showed that, in a study involving 539 patients with 840 observations, only 0.1% of patients had experienced POP complications [71]. This indicates the effectiveness of emotional loss management strategies. Contrarily to other antithrombogenic medications, warfarin has been linked to a higher risk of blood loss, with blood loss being more common among female patients [72]. This study provides important information for clinical practice, suggesting that local empathic agents could lessen the risk of haematic POP death in patients receiving anti-TRB TH.
The effects of oral SU visits and dental TRTs on individuals taking anti-TRB medications, such as warfarin and periodontics aggregates, are examined in this article by Morimoto et al. Anti-TRB medication interruptions prior to these surgeries typically increase the risk of TRB events and mortality [73]. During oral SU operations, it is advisable to administer a dose of warfarin and/or antibiotics to reduce these risks. When anti-TRB medication is continued during tooth EXs, studies reveal no discernible difference in the incidence of POP BL, as long as the normalized international ratio (PT-INR) is kept within specific bounds [74,75]. Analysing 139 patients undergoing periodontics TRTs while maintaining anti-TRB TH reveals a localized anaesthesia with no statistically significant differences in the incidence of post-TRT haemorrhages [76]. Patients on warfarin and/or ACO TH have not demonstrated any significant BL complications. Additionally, the study illustrates local haemostatic techniques utilized in TRT, including blood pressure management, collagen injection, sutures, and electrocoagulation [77]. According to the report, individuals receiving anti-TRB TRT may safely undergo oral SU operations if they follow the right blood control protocols.
Dental TRT in patients on APL drug TH is a long-standing debate. Discontinuation of medication increases the risk of TRB complications, whereas continuation leads to increased POP BL [78]. This cross-sectional study by Kumar et al. addresses the ongoing debate regarding dental TRT in patients undergoing APL TH, balancing the risks of TRB events with the potential for increased POP BL [79]. The aim was to evaluate BL risk in patients continuing APL medication during minor oral surgical PRCs. PRCs included various EXs, biopsy, and alveoloplasty [80]. Results showed that out of 200 patients, most required Level 1 haemostatic measures, with fewer needing Level 2 or 3 measures. Statistical analysis revealed significant differences among the groups. Importantly, no POP BL occurred within 24 hours for any group [81]. The study concludes that minor oral surgical PRCs can be safely performed in patients on single or dual APL TH when appropriate local haemostatic measures are applied.
Effectiveness of TachoSil Fibrin-Collagen Patches in Managing Post-EX BL for Patients on Chronic APL TH:
In the study by Lewandowski et al., patients undergoing chronic APL TH, which increases BL risks during surgeries like dental PRCs, were studied to assess the effectiveness of TachoSil fibrin-collagen patches in managing post-EX BL [82]. The majority were on dual AS and clopidogrel TH. Following tooth EX, all patients had primary BL stopped within 20-30 minutes, with successful wound coagulation. Secondary BL occurred in 4.9% of cases but was effectively managed with tranexamic acid-soaked pressure dressings [83]. The findings suggest that TachoSil patches effectively control BL and reduce secondary BL risks, offering a valuable solution for safer dental PRCs in patients on chronic APL TH.
The rising frequency of surgical PRCs in older adults on anti-TRB TH necessitates careful measures for safe TRT [84]. The cohort study by Tanimoto et al. aimed to assess tooth EX outcomes in such patients and establish an evidence-based approach aligned with guidelines [85]. The study involved 165 patients (184 cases) undergoing outpatient tooth EX while on anti-TRB TH. Medical records provided data on patient characteristics and EX PRC details. Warfarin was used in 25 patients (26 cases), while direct oral ACOs (DOACs) and APL drugs were administered to 26 (33 cases) and 91 (101 cases) patients, respectively. Fifteen patients (16 cases) received dual APL TH with concurrent ACOs, and drug TH was suspended in five cases [86]. Post-EX BL occurred in 14 cases, accounting for 7.1% of all cases. Notably, patients on DOACs who had their drug administration suspended required only suturing [87]. In conclusion, the study suggests a tendency toward the need for local haemostatic agents in patients on DOACs, reinforcing the importance of adhering to guidelines when performing tooth EX in patients on anti-TRB TH [88,89].
The Shin-Yu Lu study included 1363 patients who were undergoing tooth EXs [90]. A control group consisted of 1088 patients who were not receiving anti-TRB TH. A total of 243 patients receiving antithrombogenic TH have been divided into ACO and warfarin’s groups. There were 183 patients in the antiaggregant group, of which 125 took AS, 42 clopidogrel, and 16 combined therapies. The warfarin’s group consisted of sixty patients, of whom thirty-two were substitutes for warfarin with heparin and the other twenty-eight were ambulatory patients not receiving warfarin TH [91].
The dental PRCs are carried out using local anaesthesia with 2% lidocaine and 0.025 percent epinephrin. The EX was deemed complicated when the tooth was extracted using an aggressive surgical method. The conventional EX was achieved using gel foam and gauze compression [92]. The patients have been observed for POP blood loss, dressing compression, and expert assistance [93]. The patients were given the option of a 24-hour phone follow-up or a 7-day clinic follow-up to ascertain whether they needed professional assistance, whether their blood pressure was appropriately controlled in the case of a blood clot, and other related details [94]. There are no significant differences between the groups for the distribution of tests, the age, the number or type of tests, the dose of warfarin, or the INR. POP haemorrhage was higher in warfarin’s groups, although the differences were not statistically significant. The majority of patients have had adequate local comfort [95]. The results suggest that pre-operative suspension of warfarin and ACO medications may carry a remote but deadly risk of thromboembolism. The therapeutic levels of warfarin (INR <4) or the platelet antiaggregant TH should not be stopped before the majority of dental exams, if at all possible [96,97].
BL Risks in Patients on Single or Dual APL TH Undergoing Dental Implants:
According to the study by Kaura et al., APL drugs, like Clopidogrel and AS, play a crucial role in preventing secondary cardiac and cerebrovascular events [98]. However, managing patients requiring dental implants while on these medications poses a dilemma, as interrupting TRT increases TRB risks but raises BL concerns [99]. This research study aimed to evaluate BL risks in patients on single or dual APL TH undergoing dental implants. Sixty-five patients underwent dental implant placement, with 48 on single APL (AS) and 17 on dual TH (AS and Clopidogrel). BL was assessed both during and after SU [100,101].Results showed significant differences in BL severity between the groups intra-operatively (P = 0.000) and within 24 hours POPly (P = 0.004) based on the Visual Analog Scale (VAS). However, complications beyond 24 hours post-SU were non-significant (P = 0.277). In conclusion, dental implants can be safely placed in patients on single APL TH without discontinuation [102]. For those on dual TH, continued use is associated with mild to moderate BL risk. Collaboration with the treating cardiologist is essential before performing any dental SU in patients on APL [103].
Patients with ischemic heart disease often receive APL TH (APT). The observational study by Hoda et al. aims to establish a reliable protocol for dental EXs in such patients [104]. One hundred patients underwent dental EX after thorough case assessments, with BL time evaluated preoperatively [105]. Patients with normal BL times underwent SU under local anaesthesia, with local haemostatic measures applied post-EX. Patients were monitored for 30 minutes post-SU, with follow-up at 24-48 hours. Results revealed BL in 16 patients with mono APL TH after 1 hour, resolving by 24-48 hours. For dual APT patients, BL occurred in ten after 1 hour and one after 24 hours, also resolving by 48 hours, with statistical significance [106]. Discussion emphasizes the benefits of continuing APT for patients needing dental EX, outweighing POP BL risks. Concluding, APT is vital for preventing cardiovascular events, with minimal impact on BL during routine dental EXs [107].
The study conducted by Ylenia Brancaccio evaluated the effectiveness of four different pain management agents after dental examinations [108]. The goal was to ascertain whether local aestheticians could improve the patients' quality of life without interfering with their medication [109]. In a multicentric randomised clinical trial, four non-adjacent structural alveoli were treated with four different haemostatic PRCs: suture singular (control group), suture superior (HEM), fibrin rich in haemostasia advanced (A-PRF+), and leucocyte and fibrin rich in hemostasia inferior (L-PRF). The follow-up was conducted for two weeks following the intervention [110]. The results have shown that, in comparison to the control group, the L-PRF group had a much smaller number of partially covered sites. Furthermore, A-PRF+ and L-PRF had significantly reduced blood flow in comparison to the group with single-suture [111]. There are no differences in the risk of BL in patients receiving single or double APL TH. The incomplete analysis of the emotional flow revealed that only the L-PRF group had reduced the emotional flow in comparison to the control group [112]. The study concludes by recommending against stopping APL TH before to dental EXs and by suggesting that L-PRF and A-PRF may improve coagulation stability and reduce blood flow after SU [113].
Protocol for Dental EXs in Patients with Ischemic Heart Disease on APL TH:
The clinical study by Martinez-Moreno et al. aimed to assess BL complications in patients undergoing dental EXs while on ACO and/or APL TH over a four-year period [114]. Out of 147 patient records studied, 63 were on APL TH, 83 were on ACO TH, and one was on both. Among anticoagulated patients, 70 were on classic ACOs and 14 on new oral ACOs (NOACs). The study found five severe BL complications out of 418 dental EXs (2.11%). Notably, four of these complications occurred in patients treated with NOACs (1.68%), and one in a patient on acenocoumarol (0.42%). Overall, BL complications were low, with the highest incidence observed in patients on NOACs, followed by classic ACOs, and no complications in APL-treated patients [115]. The study of S. Cakarer introduces the Ankaferd blood stopper (ABS), a traditional product made of pepper that is used as an emetic [116]. L'ABS has shown that can improve the haemostasia if not interfering with the anti-TRB TRT. The mechanism of action of the ABG involves the formation of a protein network that facilitates the aggregation of red blood cells and aids in haemostasis [117]. 25 patients who were undergoing dental EXs as part of anti-TRB TH participated in the study; they were divided into two groups: one group treated for ABS, and the other group was in charge of controlling it [118]. As compared to the control group, the use of ABS has significantly reduced the amount of time needed for POP blood transfusions and has not required interruptions or reductions in anti-TRB TH, thereby confirming its safety and effectiveness [119]. The data analysis has shown that the use of the ABT has enabled more thorough and quick assessments, even in cases where a patient has experienced a brief episode of emotional loss following SU that has been successfully managed with the use of the ABT [120].
The study concludes by suggesting that ABS may be a safe and effective option for managing the aesthetic loss in dental EXs of patients on anti-TRB TH without the need to stop or reduce ACO medication [121]. The risk of BL after minor oral SU in 102 individuals receiving anti-TRB TRT was investigated in S. Ohba's study [122]. The majority of patients were elderly and used APL or warfarin, frequently both at once. The data showed that patients receiving a combination of warfarin and APL had a higher incidence of POP haemorrhage. Contrary to past practices, recent research indicates that ACO or antiaggregant medication may not be required for a number of dental PRCs. But the strategy might be different for more intrusive or dangerous TRTs, like intricate tooth EXs [123]. The outcomes demonstrated that POP BL was well controlled and did not result in serious side effects. In contrast to patients treated with a single anti-TRB medication, patients treated with a combination of these medications exhibited a slightly higher risk of POP BL [124]. The risk of thrombosis vs haemorrhage must be carefully weighed by clinicians, taking into account the SU type, patient condition, and anti-TRB medication being utilized. According to recent findings, many patients may experience safety and effectiveness from continuing anti-TRB TH during minor oral SU if it is handled appropriately [120].
Assessment of BL Complications in Patients Undergoing Dental EXs on Anticoagulant and/or APL TH:
Dual APL TH consists of administering APL (antiaggregant) drugs (clopidogrel and AS) to prevent TRB processes, as a preventative measure in patients with acute coronary disease, or in patients subjected to percutaneous coronary intervention. Aim of the study by Sanchez-Palomino et al. is to assess the effectiveness of a dental EX protocol in patients on dual APL TH [125]. Thirty-two patients undergoing dental EXs were included, and various variables were evaluated, including BL parameters and post-surgical measures. Sutures and gauzes impregnated with tranexamic acid were applied post-SU. Results showed that patients had higher-than-normal BL parameters but experienced no POP BL, hematoma, or infection due to the post-surgical measures ADDIN ZOTERO_ITEM CSL_CITATION {"citationID":"IbPQuBBO","properties":{"formattedCitation":"[116]","plainCitation":"[116]","noteIndex":0},"citationItems":[{"id":367,"uris":["http://zotero.org/groups/5505857/items/7GNMY3JU"],"itemData":{"id":367,"type":"article-journal","abstract":"Clear and removable tooth aligners for orthodontics treatments have become an increasingly popular alternative to fixed appliances. Even if protocols suggest removing aligners before eating or drinking, most patients retain them when they drink beverages. Alterations in the material during the daily use could determine a reduction in the application forces, affecting the desired orthodontic movement; the knowledge of how this material reacts when subjected to different aging processes is mandatory to establish the predictability of the orthodontic treatment. According to this, the aim of the present study was to assess a new objective approach, coupling spectroscopic and chemometric tools, to evaluate the changes occurring in Invisalign® aligners, the most widely used brand, exposed in vitro to coffee, tea, Coca Cola® and UV radiation for 24 and 48 h. In particular, ATR-FTIR spectroscopy was utilized to characterize, at the molecular level, the chemical and color modifications in the surfaces of the appliances; the obtained data were submitted to PCA and one-way ANOVA and Tukey’s multiple comparison test. Moreover, a colorimetry analysis was carried out to evaluate any changes in color and transparency. Coffee and tea samples displayed the major color changes between the tested groups. The differences highlighted in the spectral features of coffee, tea and UV-treated samples were mainly ascribable to color and transparency changes, because the chemical properties remained unaltered [126]. Conclusion is that dental EX is safe for patients on dual APL TH when using these measures.
The comparative study by Gupta et al. aimed to investigate the impact of low-dose AS on BL after tooth EX and compare perioperative blood loss between patients on AS TH and those not on APL TRT [127]. Additionally, it sought to discuss measures for controlling POP BL if necessary. A total of 100 patients aged 30 to 60 years were divided into two groups: one on daily low-dose AS and the other not on any APL TH [128]. All EXs were outpatient PRCs under local anaesthesia, with post-EX BL monitored at various intervals [129]. Results showed similar intraoperative blood loss between the groups, with no excessive POP BL observed. Only a few patients required haemostatic measures, primarily in the form of enhanced local interventions [130]. The study concludes that routine tooth EX in patients on long-term low-dose AS can be safely performed with appropriate haemostatic measures if needed.
J. Huang carried out a study to assess blood loss following SU in individuals using oral anti-TRB medications [131]. Patients from the dental aesthetics department of the West China Hospital of Stomatology between March 2020 and December 2021 were included in the study. Anaesthesiology was used to organize the PRCs, which were then followed by laboratory and radiologic testing. Doctors with experience carried out and attentively supervised the EXs . Following the intervention, individuals underwent local aesthetics and were monitored for any possible problems [132]. The incidence of POP blood loss was greater in patients receiving anti-TRB medication, according to the results. The number of extracts and age were found to be important risk factors for haemorrhage after SU [116]. Particularly in elderly patients and those with multiple extracts, the study offers proof that dental aesthetics is safe without interfering with anti-TRB medication.
Effectiveness of Dental EX Protocol in Patients on Dual APL TH:
The research by Babaji and Rishal aimed to assess the necessity of discontinuing dual APL TH in patients undergoing dental EXs [86]. One hundred and fifty patients undergoing dental EX were divided into two groups: Group I included 75 patients on dual APL TH, and Group II comprised 75 patients who had discontinued APL TH one week prior to EX BL time (BT) was recorded before and after EX, with both groups receiving local anaesthesia and undergoing a single molar tooth EX. POPly, no active BL was observed in either group after 1 hour or 24 hours [54] [133]. The study concluded that there was no significant difference in BT between the groups, suggesting that APL TH, whether monoTH or dual TH, need not be altered or discontinued before minor oral surgical PRCs. Most POP BL can be effectively managed with local haemostatic measures [134].
Sang-Hoon Kange's study examined the relationship between thrombocytopenia and haemorrhage-related complications after orthodontic EXs to assess the risk of blood haemorrhages in patients following the PRC [135]. The clinical records of patients diagnosed with thrombocytopenia who underwent dental EXs at a hospital between 2001 and 2019 are being examined. Dental EXs are performed for a variety of circumstances, including residual tooth decay, severe cavities, dental fractures, and infection. POP complications are managed with local anaesthetic agents, sutures, and Compression [136]. Out of 220 patients, 130 had thrombocytopenia, while 90 had normal peripheral blood pressure. Complications following SU are observed in 11 patients (5,0%), 10 (7,7%) in the thrombocytopenia group, and 1 (1,1%) in the control group. The analysis did not reveal any significant differences between the two groups, however there was a higher incidence of POP complications in the thrombocytopenia group. Therefore, surgeons should carefully consider the risk of complications following SU and use appropriate anaesthetics during examinations [137].
The focus of T. Hasegawua's study is on the multivariate relationships between risk factors and POP blood loss in patients receiving anti-TRB TH [138]. Included in the study were 122 male patients and 118 female patients, who were analysed for age, gender, comorbidity, anti-TRB TH, and other related factors. Numerous haemostatic methods were used during tooth EX, and the incidence of POP BL is approximately 25.7%, with 6.5% of cases resulting in severe BL [139]. The statistical analysis has found that the use of antibiotics before to the intervention, an increase in the PT-INR value, and a higher number of tooth EXs are significant factors associated with POP blood loss. Even though the PT-INR value was significant, its predictive ability was deemed to be imprecise [135]. A potential risk indication has been identified as a PT-INR value greater than 2.09. The use of antibiotics prior to SU has been linked to an increase in the risk of blood clotting after SU, but no significant correlation has been seen with non-steroidal anti-inflammatory drugs or APL TH [140]. The findings have helped identify significant risk factors for the patient's POP blood loss following tooth EX.
Impact of Low-Dose AS on BL after Tooth EX:
A significant percentage of people who see a dentist are on APL TRT, and the rest of them have stopped taking these medications for 3 to 7 days prior to dental SU to avoid unnecessary BL and the possibility of adverse TRB cases. This observational study by Shahzad et al. aimed to compare POP BL in tooth EX among patients continuing APL TH and those who discontinued it [141]. Patients were divided into two groups: one continuing TH (Group A) and the other discontinuing TH (Group B) with consent from their treating physician/cardiologist. Post-EX, BL was assessed at 1 hour and 24 hours. Results showed no significant difference in active BL at 1 hour between the two groups (Group A: 12%, Group B: 6%, p=0.271). However, after 24 hours, Group B had less BL and active BL than Group A (no BL: Group A: 42%, Group B: 58%; oozing: Group A: 34%, Group B: 26%; active BL: Group A: 24%, Group B: 16%, p=0.271). Mean BL was also lower in Group B (p=0.041). The study concludes that continuing ACO TH does not significantly impact BL during tooth EX [142].
Management of Dental PRCs in Patients on Anti-TRB TH:
The focus of J. Sui's study is on the use of anti-aggregates (AAP) and anti-vitamin K (AVK) medications in patients who are at risk for tooth erosions [143]. These medications are essential for preventing thromboembolic risk associated with certain diseases, but they may also raise risk during the POP period. In order to assess the risk of haemorrhage as best as possible in relation to orthodontic interventions, they are categorized according to their potential for haemorrhage [144]. Interventions of low to moderate risk can be performed in an outpatient setting, while high risk interventions, such as multiple avulsions or oral SU, are best handled in an inpatient setting. Prior to intervention, TRTs with AVK and/or AAP were discontinued to maintain an acceptable International Normalized Ratio (INR). A method has been implemented to regulate blood coagulation and local haemostasis, using resorb able haemostatic agents and suturing mucosal tissue [145]. The patient is monitored for any thromboembolic complications, and the ACO TRT is gradually resumed. The study included 93 patients who were undergoing dental examinations, demonstrating the effectiveness of perioperative management with a low risk of thromboembolic complications.
The impact of anti-TRB TH on tooth EXs in individuals receiving anti-TRB TRT was the main topic of Y. Morimoto's study [146]. The investigators examined clinical information from 382 patients who received different anti-TRB therapies, such as antiaggregant mono-TH, combined warfarin and platelets’ TH, and warfarin mono-TH. Many variables were found, such as the patient's features, the kind of dent EX, the presence of acute inflammation, the anti-TRB TH regimen, INR values, and the type of extracts. Findings indicated that 3.9% of EXs had BL after SU. Most patients had INR levels above 3.0, and the majority of cases happened within the first six days following the intervention [147]. A variety of local haemostatic PRCs, such as hematomectomy, compression, and suturing, were utilized to control blood loss following SU. Acute inflammation and surgical EX were found to be important risk factors for increased risk of BL following SU. Nonetheless, there were no discernible variations in the frequency of BL according to the kind of anti-TRB medication [148]. The research highlights the significance of proficiently handling patients subjected to anti-TRB medication during the EX process, especially in situations involving surgical EX or acute inflammation.
Relationship between Thrombocytopenia and POP BL in Orthodontic EXs:
170 patients treated with low-dose APL medications, such as AS or clopidogrel, needed to have one tooth extracted, according to a study by Archana Shenoy [104]. The patients had at least ten years of TH. They have been divided into two groups: one has stopped using antidepressant medication five days prior to the intervention, while the other has continued taking it with the doctor's approval [149]. Local haemostatics have been used during the EX to regulate blood pressure and pain. Following the PRC, the patients' POP blood flow was monitored, and they were reassessed after 15 to 60 minutes and 24 hours. The results have demonstrated an effective management of the POP blood flow with no statistically significant differences between the groups. According to the study's findings, maintaining APL TH throughout dental PRCs is safe and effective in preventing blood loss and lowering the risk of cardiovascular complications.
A prospective observational study conducted by Aranza-Canigral involved 99 patients undergoing dental TRTs for complex orthopaedic conditions [150]. All patients underwent orthodontic PRCs in accordance with standard clinical practice protocols. Specifically, patients receiving paroxetine TH were kept under observation during the orthodontic intervention, while patients receiving ACO TH monitored intravenous blood pressure (IVR), ensuring a healthy balance between the risk of haemorrhage and the need for orthodontic TRT [151]. Tests on POP blood were conducted using a clinical-objective method that defined three blood levels: mild, moderate, and severe, depending on the duration of blood loss and the necessary haemostatic measurements. Out of the 99 dental interventions performed, the majority involved benign entities; nevertheless, some moderately managed cases with localized measures within an hour after the intervention were also observed [152]. According to the study, adding new blood tests to pre-operative care for patients with complex oral and dental problems may improve the effectiveness and safety of surgical PRCs.
Multivariate Relationships between Risk Factors and POP Blood Loss in Patients on Anti-TRB TH:
In order to determine potential risk factors for POP BL in patients undergoing tooth EXs while receiving anti-TRB medication, R. Pippi conducted a study [153]. The researchers employed local anaesthetic regimens and performed surgical interventions. Preliminary and multivariate analyses were performed on the data to assess the safety index and the incidence of POP BL in relation to age, sex, number of EXs, anti-TRB TH, and other clinics [154]. The use of more local anaesthetics may have a detrimental effect on POP safety, although the use of ACOs did not significantly raise the risk of BL after EX, according to the results [155]. Additionally, the study discovered that pre-operative antibiotic use did not significantly enhance the risk of BL and that post-EX haemorrhage was more common among individuals undergoing EXs in the higher quadrants. Anti-TRB medication did not appear to have a substantial effect on blood ejection-related POP problems [156].
Conclusion
In conclusion, the studies reviewed shed light on the BL risks associated with various anti-TRB therapies during dental PRCs. Whether it's low-dose AS, single or dual APL TH, or ACO TRT, each regimen poses its own set of considerations for clinicians. Understanding the nuances of these risks is crucial for informed decision-making in dental EXs and implant PRCs. Moreover, the impact of low-dose AS on POP BL after tooth EX highlights the need for personalized approaches to patient care. Multivariate analyses underscore the complex interplay of risk factors contributing to POP blood loss in patients on anti-TRB TH. Moving forward, continued research and clinical vigilance will be essential in optimizing outcomes and ensuring patient safety in this population.
Author contributions: F.I. contributed to the first draft, approved the final version, and take responsibility for the accuracy or reported findings. G.D., A.M.I., F.P., I.T., R.V.G., C.C., A.M., A.P. and A.D.I. contributed to the draft and proved the final version.
Conflict of interest: The authors declare that they have no competing interests related to this manuscript.
References
- Kay, E. (2023) Dentistry’s Need for a Strong Evidence Base. Evid Based Dent 24: 97.
- Chiappelli, F. (2019) Evidence-Based Dentistry: Two Decades and Beyond. J Evid Based Dent Pract 19: 7–16.
- Pihlstrom, B.L, Curran, A.E, Voelker, H.T, Kingman, A. (2012) Randomized Controlled Trials: What Are They and Who Needs Them? Periodontol 2000 59: 14–31.
- Wójcik, S, Mocny-Pachońska, K, Bisch-Wójcik, S, Balicz, A, Morawiec, T. (2022) Perioperative Management of Dental Surgery Patients Chronically Taking Antithrombotic Medications. Int J Environ Res Public Health 19: 16151.
- Jiménez-García, N, de la Torre Lima, J, García Alegría, J. The Role of Aspirin as Antiaggregant Therapy in Primary Prevention. An Update. Med Clin (Barc) 2019, 153, 326–331.
- Hink, U, Voigtländer, T. (2020) Necessity of Antiaggregation and Anticoagulation and Its Prognostic Impact: A Cardiologist’s View. Visc Med 36: 264–273.
- Lordan, R, Tsoupras, A, Zabetakis, I. (2022) Investigation of Platelet Aggregation in Atherosclerosis. Methods Mol Biol 2419:333–347.
- Lelli, N, Rizkallah, R, Ferrari, P, Pedretti, S, Cariani, E, Trenti, T. (2017) Proposal of a “Gradient Model” to Evaluate Residual Platelet Activity on Antiplatelet Therapy: A Pilot Study. Thromb Res 150: 19–21.
- Morales Vidal, S.G, Ruland, S. Platelet Antiaggregants in Stroke Prevention. Neurol Clin 2013, 31, 633–657.
- Soodi, D, VanWormer, J.J, Rezkalla, S.H. (2020) Aspirin in Primary Prevention of Cardiovascular Events. Clin Med Res 18: 89–94.
- Maree, A.O, Fitzgerald, D.J. (2007) Variable Platelet Response to Aspirin and Clopidogrel in Atherothrombotic Disease. Circulation 115: 2196–2207.
- Wang, D, Yang, X.-H, Zhang, J.-D, Li, R.-B, Jia, M, Cui, X.-R. (2018) Compared Efficacy of Clopidogrel and Ticagrelor in Treating Acute Coronary Syndrome: A Meta-Analysis. BMC Cardiovasc Disord 18: 217.
- Guerbaai, R.-A, Mahata, I, Maréchaux, S, Le Jemtel, T.H, Ennezat, P.-V. (2019) Is Ticagrelor Worth Its High Cost and Side-Effects? Acta Cardiol 74: 93–98.
- Herbert, J.-M, Savi, P. (2003) P2Y12, a New Platelet ADP Receptor, Target of Clopidogrel. Semin Vasc Med 3: 113–122.
- Silva, M.V.F, Dusse, L.M.S, Vieira, L.M, Carvalho, M. das G. (2013) Platelet Antiaggregants in Primary and Secondary Prevention of Atherothrombotic Events. Arq Bras Cardiol 100: e78-84.
- Education Technology in Orthodontics and Paediatric Dentistry during the COVID-19 Pandemic: A Systematic Review – PubMed.
- Isacco, C.G, Ballini, A, De Vito, D, Nguyen, K.C.D, Cantore, S, Bottalico, L, Quagliuolo, L, Boccellino, M, Di et al. (2021) Rebalancing the Oral Microbiota as an Efficient Tool in Endocrine, Metabolic and Immune Disorders. Endocr Metab Immune Disord Drug Targets 21: 777–784.
- Inchingolo, A.D, Inchingolo, A.M, Malcangi, G, Avantario, P, Azzollini, D, et al. (2022) Effects of Resveratrol, Curcumin and Quercetin Supplementation on Bone Metabolism-A Systematic Review. Nutrients 14: 35199.
- Miciak-Ławicka, E, Begier-Krasińska, B, Tykarski, A, Krasiński, Z. (2018) Does the Timing of Aspirin Administration Influence Its Antiplatelet Effect – Review of Literature on Chronotherapy. Kardiochir Torakochirurgia Pol 15: 125–129.
- Inchingolo, A.D, Malcangi, G, Semjonova, A, Inchingolo, A.M, Patano, A, et al. (2022) Oralbiotica/Oralbiotics: The Impact of Oral Microbiota on Dental Health and Demineralization: A Systematic Review of the Literature. Children (Basel) 9: 1014.
- Campanella, V, Syed, J, Santacroce, L, Saini, R, Ballini, A, Inchingolo, F. (2018) Oral Probiotics Influence Oral and Respiratory Tract Infections in Pediatric Population: A Randomized Double-Blinded Placebo-Controlled Pilot Study. Eur Rev Med Pharmacol Sci 22: 8034–8041.
- Boccellino, M, Di Stasio, D, Dipalma, G, Cantore, S, Ambrosio, P, et al. (2019) Steroids and Growth Factors in Oral Squamous Cell Carcinoma: Useful Source of Dental-Derived Stem Cells to Develop a Steroidogenic Model in New Clinical Strategies. Eur Rev Med Pharmacol Sci 23: 8730–8740.
- Christiansen, M, Grove, E.L, Hvas, A.-M. (2021) Contemporary Clinical Use of Aspirin: Mechanisms of Action, Current Concepts, Unresolved Questions, and Future Perspectives. Semin Thromb Hemost 47: 800–814.
- Ornelas, A, Zacharias-Millward, N, Menter, D.G, Davis, J.S, Lichtenberger, L, et al (2017) Beyond COX-1: The Effects of Aspirin on Platelet Biology and Potential Mechanisms of Chemoprevention. Cancer Metastasis Rev 36: 289–303.
- Maspero, C, Fama, A, Cavagnetto, D, Abate, A, Farronato, M. (2019) Treatment of Dental Dilacerations. J Biol Regul Homeost Agents 33: 1623–1627.
- Lanteri, V, Cossellu, G, Farronato, M, Ugolini, A, Leonardi, R, et al (2020) Assessment of the Stability of the Palatal Rugae in a 3D-3D Superimposition Technique Following Slow Maxillary Expansion (SME). Sci Rep 10: 2676.
- Minervini, G, Franco, R, Marrapodi, M.M, Di Blasio, M, Isola, G, Cicciù, M. (2023) Conservative Treatment of Temporomandibular Joint Condylar Fractures: A Systematic Review Conducted According to PRISMA Guidelines and the Cochrane Handbook for Systematic Reviews of Interventions. Journal of Oral Rehabilitation 50: 886–893.
- Minervini, G, Franco, R, Marrapodi, M.M, Fiorillo, L, Cervino, G, Cicciù, M. Post‐traumatic Stress, Prevalence of Temporomandibular Disorders in War Veterans: Systematic Review with Meta‐analysis. Journal of Oral Rehabilitation 2023.
- Minervini, G, Franco, R, Marrapodi, M.M, Di Blasio, M, Ronsivalle, V, et al (2023) Children Oral Health and Parents Education Status: A Cross Sectional Study. BMC Oral Health 23: 787.
- Cicciù, M, Minervini, G, Franco, R, Marrapodi, MM, Fiorillo, L, Cervino, G.(2023) The Association between Parent Education Level, Oral Health, and Oral-Related Sleep Disturbance. An Observational Crosssectional Study. EUROPEAN JOURNAL OF PAEDIATRIC DENTISTRY 1.
- Minervini, G, Franco, R, Marrapodi, M.M, Almeida, L.E, Ronsivalle, V, Cicciù, M. (2023) Prevalence of Temporomandibular Disorders (TMD) in Obesity Patients: A Systematic Review and Meta-Analysis. Journal of Oral Rehabilitation 50: 1544–1553.
- Stewart, L.C, Langtry, J. a. A. (2010) Clopidogrel: Mechanisms of Action and Review of the Evidence Relating to Use during Skin Surgery Procedures. Clin Exp Dermatol 35: 341–345.
- Coloccia, G, Inchingolo, A.D, Inchingolo, A.M, Malcangi, G, Montenegro, V, et al. (2021) Effectiveness of Dental and Maxillary Transverse Changes in Tooth-Borne, Bone-Borne, and Hybrid Palatal Expansion through Cone-Beam Tomography: A Systematic Review of the Literature. Medicina (Kaunas) 57: 288.
- Arrigoni, R, Ballini, A, Santacroce, L, Cantore, S, Inchingolo, A, Inchingolo, F, et al (2022) Another Look at Dietary Polyphenols: Challenges in Cancer Prevention and Treatment. Curr Med Chem 29: 1061–1082.
- Sánchez-Palomino, P, Sánchez-Cobo, P, Rodriguez-Archilla, A, González-Jaranay, M, et al (2015) Dental Extraction in Patients Receiving Dual Antiplatelet Therapy. Med Oral Patol Oral Cir Bucal 20: e616-620.
- Saccomanno, S, Mummolo, S, Giancaspro, S, Manenti, R.J, Mastrapasqua, R.F, et al (2021) Catering Work Profession and Medico-Oral Health: A Study on 603 Subjects. Healthcare (Basel) 9: 582.
- Quinzi, V, Tecco, S, Nota, A, Caggiati, E, Mummolo, S, Marzo, G. (2020) Mesial Rotation of the Upper First Molar: Association with Anterior Dental Crowding in Mixed and Permanent Dentition. Applied Sciences 10: 5301.
- Marchetti, E, Mummolo, S, Mancini, L, Quinzi, V, Pontieri, E, Marzo, G, Campanella, V. Decontamination in the Dental Office: A Comparative Assessment of a New Active Principle. Dental Cadmos 2021.
- Piancino, M.G, Di Benedetto, L, Matacena, G, Deregibus, A, Marzo, G, Quinzi, V. (2019)Paediatric Orthodontics Part 3: Masticatory Function during Development. Eur J Paediatr Dent 20: 247–249.
- Schreuder, W.H, Peacock, Z.S. (2015) Antiplatelet Therapy and Exodontia. J Am Dent Assoc 146: 851–856.
- Mauprivez, C, Khonsari, R.H, Razouk, O, Goudot, P, Lesclous, P, Descroix, V. (2016) Management of Dental Extraction in Patients Undergoing Anticoagulant Oral Direct Treatment: A Pilot Study. Oral Surg Oral Med Oral Pathol Oral Radiol 122: e146–e155.
- Inchingolo, F, Inchingolo, A.M, Latini, G, Ferrante, L, Trilli, I, Del Vecchio, G, et al (2023) Oxidative Stress and Natural Products in Orthodontic Treatment: A Systematic Review. Nutrients 16: 113.
- Minervini, G, Marrapodi, M.M, Cicciù, M. (2023) Online Bruxism‐related Information: Can People Understand What They Read? A Cross‐Sectional Study. J of Oral Rehabilitation 50: 1211–1216.
- Lewandowski, B, Myszka, A, Migut, M, Czenczek-Lewandowska, E, Brodowski, R. (2021) Analysing the Effectiveness of Topical Bleeding Care Following Tooth Extraction in Patients Receiving Dual Antiplatelet Therapy-Retrospective Observational Study. BMC Oral Health 21: 31.
- Gaudy, J.F, Ankri, A, Tager, F, El Haddioui, A, Bravetti, P, Lafont, A, et al (2005) [Anticoagulants and dental extractions]. Arch Mal Coeur Vaiss 98: 859–866.
- Inchingolo, F, Inchingolo, A.M, Latini, G, Palmieri, G, Di Pede, C, Trilli, I, Ferrante, L, et al. (2023) Application of Graphene Oxide in Oral Surgery: A Systematic Review. Materials (Basel) 16: 6293.
- Inchingolo, A.M, Malcangi, G, Costa, S, Fatone, M.C, Avantario, P, et al. (2023) Tooth Complications after Orthodontic Miniscrews Insertion. International Journal of Environmental Research and Public Health 2023, 20.
- Variability in Platelet Response to the Antiplatelet Agents Aspirin and Clopidogrel: Mechanisms, Measurement, and Clinical Relevance - PubMed Available online: https://pubmed.ncbi.nlm.nih.gov/19258834/ (accessed on 2 May 2024).
- Inchingolo, A.D, Dipalma, G, Inchingolo, A.M, Malcangi, G, Santacroce, L, et al. (2021) The 15-Months Clinical Experience of SARS-CoV-2: A Literature Review of Therapies and Adjuvants. Antioxidants (Basel) 10: 881.
- Polymers | Free Full-Text | Poloxamer-Based Hydrogel as Drug Delivery System: How Polymeric Excipients Influence the Chemical-Physical Properties.
- Correlation between Dental Vestibular-Palatal Inclination and Alveolar Bone Remodeling after Orthodontic Treatment: A CBCT Analysis – PubMed.
- van Diermen, D.E, Aartman, I.H.A, Baart, J.A, Hoogstraten, J, van der Waal, I. (2009) Dental Management of Patients Using Antithrombotic Drugs: Critical Appraisal of Existing Guidelines. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107: 616–624.
- Maspero, C, Abate, A, Cavagnetto, D, Fama, A, Stabilini, A, Farronato, G, Farronato, M. (2019) Operculectomy and Spontaneous Eruption of Impacted Second Molars: A Retrospective Study. J Biol Regul Homeost Agents 33: 1909–1912.
- Farronato, M, Baselli, G, Baldini, B, Favia, G, Tartaglia, G.M. 3D Cephalometric Normality Range: Auto Contractive Maps (ACM) Analysis in Selected Caucasian Skeletal Class I Age Groups. Bioengineering (Basel) 2022, 9: 216.
- Gröbe, A, Fraederich, M, Smeets, R, Heiland, M, Kluwe, L, Zeuch, J, Haase, M, et al. Postoperative Bleeding Risk for Oral Surgery under Continued Clopidogrel Antiplatelet Therapy. Biomed Res Int 2015, 2015: 823651.
- Lillis, T, Ziakas, A, Koskinas, K, Tsirlis, A, Giannoglou, G. Safety of Dental Extractions during Uninterrupted Single or Dual Antiplatelet Treatment. Am J Cardiol 2011, 108, 964–967.
- Page, M.J, McKenzie, J.E, Bossuyt, P.M, Boutron, I, Hoffmann, T.C, Mulrow, C.D, et al. (2021) The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. PLOS Medicine 18: e1003583.
- Sunu, V.S, Roshni, A, Ummar, M, Aslam, S.A, Nair, R.B, Thomas, T. (2021) A Longitudinal Study to Evaluate the Bleeding Pattern of Patients on Low Dose Aspirin Therapy Following Dental Extraction. J Family Med Prim Care 10: 1399–1403.
- Ferrazzano, G.F, Sangianantoni, S, Mitrano, R.L, Ingenito, A, Alcidi, B, Cantile, T. (2019) Assessing Changes in Oral Health-Related Quality of Life and Body Growth in 3-5 Years Old Children Following Dental Treatment under General Anaesthesia Due to Severe Dental Caries. Eur J Paediatr Dent 20, 214–218.
- Kyriakaki, I, Karanikola, T, Lillis, T, Kontonasaki, E, Dabarakis, N. (2019) Effect of Direct Oral Anticoagulant Dabigatran on Early Bone Healing: An Experimental Study in Rats. J Adv Periodontol Implant Dent 15: 86–92.
- Ferrazzano, G.F, Cantile, T, Sangianantoni, G, Ingenito, A, Rengo, S, Alcidi, B, Spagnuolo, G. (2019) Oral Health Status and Unmet Restorative Treatment Needs (UTN) in Disadvantaged Migrant and Not Migrant Children in Italy. Eur J Paediatr Dent 20: 10–14.
- Eapen, B.V, Baig, M.F, Avinash, S. (2017) An Assessment of the Incidence of Prolonged Postoperative Bleeding After Dental Extraction Among Patients on Uninterrupted Low Dose Aspirin Therapy and to Evaluate the Need to Stop Such Medication Prior to Dental Extractions. J Maxillofac Oral Surg 16: 48–52.
- Ferrazzano, G.F, Sangianantoni, G, Cantile, T, Amato, I, Orlando, S, Ingenito, A. (2012) Dental Enamel Defects in Italian Children with Cystic Fibrosis: An Observational Study. Community Dent Health 29: 106–109.
- Knowledge and Awareness of Chronic Bronchitis and Its Oral Manifestation among Dental Students and Practitioners – PubMed.
- Ferrazzano, G.F, Salerno, C, Sangianantoni, G, Caruso, S, Ingenito, A, Cantile, T. (2020) The Effect of Dental Treatment under General Anesthesia on Quality of Life and Growth and Blood Chemistry Parameters in Uncooperative Pediatric Patients with Compromised Oral Health: A Pilot Study. Int J Environ Res Public Health 17: 4407.
- Sadhasivam, G, Bhushan, S, Chiang, K.C, Agarwal, N, Vasundhar, P.L. (2016) Clinical Trial Evaluating the Risk of Thromboembolic Events During Dental Extractions. J Maxillofac Oral Surg 15: 506–511
- Statman, B.J. (2023) Perioperative Management of Oral Antithrombotics in Dentistry and Oral Surgery: Part 2. Anesth Prog 70: 37–48.
- Buchbender, M, Schlee, N, Kesting, M.R, Grimm, J, Fehlhofer, J, Rau, A. (2021)A Prospective Comparative Study to Assess the Risk of Postoperative Bleeding after Dental Surgery While on Medication with Direct Oral Anticoagulants, Antiplatelet Agents, or Vitamin K Antagonists. BMC Oral Health 21: 504.
- Zhou, M.X, Viozzi, C.F, Heneberk, O, Lee, S.K, Klarich, K.W, Salinas, T.J. (2024) Oral Health Clearance Outcomes for Cardiovascular Surgery. Mayo Clin Proc Innov Qual Outcomes 8: 121–130.
- AlSheef, M, Gray, J, AlShammari, A. (2022) Risk of Postoperative Bleeding Following Dental Extractions in Patients on Antithrombotic Treatment. Saudi Dent J 33: 511–517.
- Nota, A, Caruso, S, Cantile, T, Gatto, R, Ingenito, A, Tecco, S, Ferrazzano, G.F. Socioeconomic Factors and Oral Health-Related Behaviours Associated with Dental Caries in Preschool Children from Central Italy (Province of Ascoli Piceno). Biomed Res Int 2019: 7981687.
- Della Corte, A, Bancone, C, Spadafora, A, Borrelli, M, Galdieri, N, Quintiliano, et al (2017) Postoperative Bleeding in Coronary Artery Bypass Patients on Double Antiplatelet Therapy: Predictive Value of Preoperative Aggregometry. Eur J Cardiothorac Surg 52: 901–908.
- Morimoto, Y, Niwa, H, Minematsu, K. (2009) Hemostatic Management for Periodontal Treatments in Patients on Oral Antithrombotic Therapy: A Retrospective Study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108: 889–896.
- Lukács, D, Stáczer, N, Vajta, L, Olasz, L, Joób-Fancsaly, Á, Szalma, J. (2016) [Dental and oral surgical treatment of medication-induced bleeding patients: Audit of the national guideline in Hungary]. Orv Hetil 157: 1722–1728.
- Malcangi, G, Patano, A, Morolla, R, De Santis, M, Piras, F, Settanni, V, Mancini, A, et al. (2023) Analysis of Dental Enamel Remineralization: A Systematic Review of Technique Comparisons. Bioengineering 10: 472.
- Severino, M, Caruso, S, Ferrazzano, G.F, Pisaneschi, A, Fiasca, F, Caruso, S, et al (2021) Prevalence of Early Childhood Caries (ECC) in a Paediatric Italian Population: An Epidemiological Study. Eur J Paediatr Dent 22, 189–198.
- Giudice, A, Esposito, M, Bennardo, F, Brancaccio, Y, Buti, J, Fortunato, L. (2019) Dental Extractions for Patients on Oral Antiplatelet: A within-Person Randomised Controlled Trial Comparing Haemostatic Plugs, Advanced-Platelet-Rich Fibrin (A-PRF+) Plugs, Leukocyte- and Platelet-Rich Fibrin (L-PRF) Plugs and Suturing Alone. Int J Oral Implantol (Berl) 12: 77–87.
- Di Stasio, D, Romano, A, Gentile, C, Maio, C, Lucchese, A, Serpico, R, et al (2018) Systemic and Topical Photodynamic Therapy (PDT) on Oral Mucosa Lesions: An Overview. J Biol Regul Homeost Agents 32: 123–126.
- Kumar, A, Rao, A, Nimkar, A, Mahajani, M, Suvvari, R.K, Bhanot, R. (2023) Evaluating the Need of Continuing the Antiplatelet Drug Therapy in Patients Undergoing Minor Oral Surgical Procedures. J Pharm Bioallied Sci 13: S80–S83.
- Minervini, G, Lucchese, A, Perillo, L, Serpico, R, Minervini, G. (2015) Unilateral Superior Condylar Neck Fracture with Dislocation in a Child Treated with an Acrylic Splint in the Upper Arch for Functional Repositioning of the Mandible. Cranio 35: 337–341.
- Hua, W, Huang, Z, Huang, Z. (2021) Bleeding Outcomes After Dental Extraction in Patients Under Direct-Acting Oral Anticoagulants vs. Vitamin K Antagonists: A Systematic Review and Meta-Analysis. Front Pharmacol 12: 702057.
- Lewandowski, B, Myszka, A, Migut, M, Czenczek-Lewandowska, E, Brodowski, R. (2021) Analysing the Effectiveness of Topical Bleeding Care Following Tooth Extraction in Patients Receiving Dual Antiplatelet Therapy-Retrospective Observational Study. BMC Oral Health 21: 31.
- Contaldo, M, Della Vella, F, Raimondo, E, Minervini, G, Buljubasic, M, Ogodescu, A, Sinescu, C, Serpico, R. Early Childhood Oral Health Impact Scale (ECOHIS): Literature Review and Italian Validation. Int J Dent Hyg 2020, 18, 396–402.
- Minervini, G, Franco, R, Marrapodi, M.M, Fiorillo, L, Cervino, G, Cicciù, M. Economic Inequalities and Temporomandibular Disorders: A Systematic Review with Meta-Analysis. J Oral Rehabil 2023, 50, 715–723.
- Clinical Study of Medically Compromised Patients Undergoing Tooth Extraction While Receiving Antithrombotic Therapy - Tanimoto - 2022 - Oral Science International - Wiley Online Library.
- Babaji, P, Rishal, Y. Clinical Evaluation of Role of Dual Antiplatelet Therapy on Bleeding after Dental Extraction. Contemp Clin Dent 2018, 9, 41–44.
- Prevalence of Temporomandibular Disorders in Subjects Affected by Parkinson Disease: A Systematic Review and Metanalysis - Minervini - 2023 - Journal of Oral Rehabilitation.
- Rathi, S, Chaturvedi, S, Abdullah, S, Rajput, G, Alqahtani, N.M, et al (2023) Clinical Trial to Assess Physiology and Activity of Masticatory Muscles of Complete Denture Wearer Following Vitamin D Intervention. Medicina (Kaunas) 59: 410.
- Inchingolo, A.D, Carpentiere, V, Piras, F, Netti, A, Ferrara, I, Campanelli, M, et al. (2018)Orthodontic Surgical Treatment of Impacted Mandibular Canines: Systematic Review and Case Report. Applied Sciences 12: 8008.
- Lu, S.-Y, Lin, L.-H, Hsue, S.-S. (2018) Management of Dental Extractions in Patients on Warfarin and Antiplatelet Therapy. J Formos Med Assoc 117: 979–986.
- Moscarella, E, González, S, Agozzino, M, Sánchez-Mateos, J.L.S, Panetta, C, et al (2012) Pilot Study on Reflectance Confocal Microscopy Imaging of Lichen Planus: A Real-Time, Non-Invasive Aid for Clinical Diagnosis. J Eur Acad Dermatol Venereol 26: 1258–1265.
- Sammartino, G, Dohan Ehrenfest, D.M, Carile, F, Tia, M, Bucci, P. (2011) Prevention of Hemorrhagic Complications after Dental Extractions into Open Heart Surgery Patients under Anticoagulant Therapy: The Use of Leukocyte- and Platelet-Rich Fibrin. J Oral Implantol 37: 681–690.
- Contaldo, M, Poh, C.F, Guillaud, M, Lucchese, A, Rullo, R, Lam, S, et al (2013). Oral Mucosa Optical Biopsy by a Novel Handheld Fluorescent Confocal Microscope Specifically Developed: Technologic Improvements and Future Prospects. Oral Surg Oral Med Oral Pathol Oral Radiol 116: 752–758.
- Contaldo, M, Itro, A, Lajolo, C, Gioco, G, Inchingolo, F, Serpico, R. (2020) Overview on Osteoporosis, Periodontitis and Oral Dysbiosis: The Emerging Role of Oral Microbiota. Applied Sciences 10: 6000.
- Uz, B, Guven, G.S, Isik, A, Kuyumcu, M.E, Bektas, O, Eliacik, E, Aksu, S, Goker, H, Buyukasik, Y, Sayinalp, N, et al. Long-Term Sustained Hemorrhage Due to Bone Marrow Biopsy Successfully Treated with Topical Ankaferd Hemostat in a Bleeding-Prone Patient with Secondary Amyloidosis. Clin Appl Thromb Hemost 2013, 19, 338–340.
- Radiosurgery-Assisted Gingival Displacement: A Proof of Concept Technique to Enhance the Efficiency of Intraoral Digital Impression – PubMed.
- Inchingolo, A.D, Gargiulo, C.I, Malcangi, G, Ciocia, A.M, Patano, A, Azzollini, D, et al. (2022) Diagnosis of SARS-CoV-2 during the Pandemic by Multiplex RT-rPCR hCoV Test: Future Perspectives. Pathogens 11: 1378.
- Kaura, S, Rai, R, Satia, G, Budhiraja, N, Mohan, B. (2022) Assessment of Bleeding in Patients on Antiplatelets Undergoing Dental Implants. J Maxillofac Oral Surg 21: 260–264.
- Contaldo, M, Fusco, A, Stiuso, P, Lama, S, Gravina, A.G, Itro, A, et al. (2021) Oral Microbiota and Salivary Levels of Oral Pathogens in Gastro-Intestinal Diseases: Current Knowledge and Exploratory Study. Microorganisms 9, 1064.
101. Inchingolo, A.M, Fatone, M.C, Malcangi, G, Avantario, P, Piras, F, et al. (2022) Modifiable Risk Factors of Non-Syndromic Orofacial Clefts: A Systematic Review. Children (Basel) 9: 1846.
102. Unusual Conditions Impairing Saliva Secretion: Developmental Anomalies of Salivary Glands – PubMed.
103. Paoletti, I, Fusco, A, Grimaldi, E, Perillo, L, Coretti, L, Di Domenico, M, et al. (2013) Assessment of Host Defence Mechanisms Induced by Candida Species. Int J Immunopathol Pharmacol 26: 663–672.
104. Hoda, Md.M, Navaneetham, R, Sham, M.E, Menon, S, Kumar, V, Archana, S.(2021) Assessment of Postoperative Bleeding after Dental Extractions in Patients Who Are On Antiplatelet Therapy: A Prospective Study. Ann Maxillofac Surg 11: 75–79.
106. Bacci, C, Schiazzano, C, Zanon, E, Stellini, E, Sbricoli, L. Bleeding Disorders and Dental Implants: Review and Clinical Indications. J Clin Med 2023, 12, 4757.
108. Brancaccio, Y, Antonelli, A, Barone, S, Bennardo, F, Fortunato, L, Giudice, A. (2021) Evaluation of Local Hemostatic Efficacy after Dental Extractions in Patients Taking Antiplatelet Drugs: A Randomized Clinical Trial. Clin Oral Investig 25: 1159–1167.
109. Di Spirito, F, Amato, A, Di Palo, M.P, Contaldo, M, D’Ambrosio, F, Lo Giudice, R, Amato, M. Oral Lesions Following Anti-SARS-CoV-2 Vaccination: A Systematic Review. Int J Environ Res Public Health 19: 10228.
111. Romano, A, Santarelli, A, Lajolo, C, Della Vella, F, Mascitti, M, Serpico, R, Contaldo, M. Analysis of Oral Mucosa Erosive-Ulcerative Lesions by Reflectance Confocal Microscopy. J Biol Regul Homeost Agents 2019, 33, 11-17. DENTAL SUPPLEMENT.
113. Crincoli, V, Anelli, M.G, Quercia, E, Piancino, M.G, Di Comite, M. (2019) Temporomandibular Disorders and Oral Features in Early Rheumatoid Arthritis Patients: An Observational Study. Int J Med Sci 16: 253–263.
114. Martínez-Moreno, E, Martínez-López, F, Rodríguez-Lozano, F.J, Oñate-Sánchez, R.E. (2021) Bleeding Complications in Anticoagulated and/or Antiplatelet-Treated Patients at the Dental Office: A Retrospective Study. Int J Environ Res Public Health 18:1609.
115. Crincoli, V, Di Comite, M, Guerrieri, M, Rotolo, R.P, Limongelli, L, Tempesta, A, Iannone, F, Rinaldi, A, Lapadula, G, Favia, G. Orofacial Manifestations and Temporomandibular Disorders of Sjögren Syndrome: An Observational Study. Int J Med Sci 2018, 15, 475–4834.
116. Çakarer, S, Eyüpoğlu, E, Günes, Ç.Ö, Küseoğlu, B.G, Berberoğlu, H.K, Keskin, C. Evaluation of the Hemostatic Effects of Ankaferd Blood Stopper during Dental Extractions in Patients on Antithrombotic Therapy. Clin Appl Thromb Hemost 2013, 19, 96–99.
117. Crincoli, V, Scivetti, M, Di Bisceglie, M.B, Pilolli, G.P, Favia, G. Unusual Case of Adverse Reaction in the Use of Sodium Hypochlorite during Endodontic Treatment: A Case Report. Quintessence Int 39, e70-73.
118. Crincoli, V, Ballini, A, Fatone, L, Di Bisceglie, M.B, Nardi, G.M, Grassi, F.R. (2016) Cytokine Genotype Distribution in Patients with Periodontal Disease and Rheumatoid Arthritis or Diabetes Mellitus. J Biol Regul Homeost Agents 30: 863–866.
119. McDonald, J.W, Ali, M. (1983) Recovery of Cyclooxygenase Activity after Aspirin in Populations of Platelets Separated on Stractan Density Gradients. Prostaglandins Leukot Med 12: 245–252.
120. Giorgini, E, Sabbatini, S, Conti, C, Rubini, C, Rocchetti, R, Fioroni, M, Memè, L, Orilisi, G. (2021) Fourier Transform Infrared Imaging Analysis of Dental Pulp Inflammatory Diseases. Oral Dis 23: 484–491.
121. Memè, L, Notarstefano, V, Sampalmieri, F, Orilisi, G, Quinzi, V. (2021) ATR-FTIR Analysis of Orthodontic Invisalign® Aligners Subjected to Various In Vitro Aging Treatments. Materials (Basel) 14: 818.
122. Papadiochos, I, Strantzias, P, Bourazani, M, Derila, A, Petsinis, V. A (2024) “Tie-Over” Hemostatic Approach in Emergency Department: An Alternative Option for Recurrent Episodes of Postoperative Intraoral Hemorrhage. J Maxillofac Oral Surg 23: 402–408.
124. Ueda, K, Inokoshi, M, Kubota, K, Yamaga, E, Minakuchi, S. (2023) Factors Influencing Postoperative Bleeding after Dental Extraction in Older Adult Patients Receiving Anticoagulation Therapy. Clin Oral Investig 28: 22,
125. Sánchez-Palomino, P, Sánchez-Cobo, P, Rodriguez-Archilla, A, González-Jaranay, M, et al (2015) Dental Extraction in Patients Receiving Dual Antiplatelet Therapy. Med Oral Patol Oral Cir Bucal 20: e616-620.
127. Gupta, R, Dugal, A, Sane, V.D, Hiwarkar, S, Khandelwal, S, Iyengar, A. (2018) Effect of Low-Dose Aspirin on Bleeding Following Exodontia: A Prospective Clinical Study. J Maxillofac Oral Surg 17: 350–355.
128. Tatullo, M, Marrelli, M, Scacco, S, Lorusso, M, Doria, S, Sabatini, R, Auteri, P, et al (2012) Relationship between Oxidative Stress and “Burning Mouth Syndrome” in Female Patients: A Scientific Hypothesis. Eur Rev Med Pharmacol Sci 16: 1218–1221.
129. Chuai, Y, Dai, B, Liu, X, Hu, M, Wang, Y, Zhang, H. (2023) Association of Vitamin K, Fibre Intake and Progression of Periodontal Attachment Loss in American Adults. BMC Oral Health 23: 303.
131. Huang, J, Liu, J, Shi, H, Wu, J, Liu, J, Pan, J. (2022) Risk Factors for Bleeding after Dental Extractions in Patients Receiving Antithrombotic Drugs - A Case Control Study. J Dent Sci 17: 780–786.
132. Ballini, A, Cantore, S, Farronato, D, Cirulli, N, Inchingolo, F, Papa, F, et al. (2015) Periodontal Disease and Bone Pathogenesis: The Crosstalk between Cytokines and Porphyromonas Gingivalis. J Biol Regul Homeost Agents 29: 273–281.
133. Inchingolo, F, Ballini, A, Georgakopoulos, P.G, Inchingolo, A.D, Tsantis, S, et al (2018). IMMEDIATE IMPLANT PLACEMENT BY USING BONE-ALBUMIN ALLOGRAFT AND CONCENTRATED GROWTH FACTORS (CGFS): PRELIMINARY RESULTS OF A PILOT STUDY. Oral & Implantology 11: 31–40.
135. Kang, S.-H, Kang, M.-J. (2021) The Incidence of Postoperative Hemorrhage after Tooth Extraction in Patients with Thrombocytopenia. J Korean Assoc Oral Maxillofac Surg 47: 190–196.
137. Cantore, S, Ballini, A, De Vito, D, Martelli, F.S, Georgakopoulos, I, Almasri, M, et al.(2017) Characterization of Human Apical Papilla-Derived Stem Cells. J Biol Regul Homeost Agents 31: 901–910.
138. Hasegawa, T, Yanamoto, S, Tachibana, A, Kojima, Y, Koyama, Y, Maeda, M, Komori, T, (2019) Japanese Study Group of Cooperative Dentistry with Medicine (JCDM) The Risk Factors Associated with Postoperative Hemorrhage after Tooth Extraction: A Multi-Center Retrospective Study of Patients Receiving Oral Antithrombotic Therapy. Oral Maxillofac Surg 21: 397–404.
139. Ballini, A, Santacroce, L, Cantore, S, Bottalico, L, Dipalma, G, Topi, S, et al (2019) Probiotics Efficacy on Oxidative Stress Values in Inflammatory Bowel Disease: A Randomized Double-Blinded Placebo-Controlled Pilot Study. Endocr Metab Immune Disord Drug Targets 19: 373–381.
140. Santacroce, L, Charitos, I.A, Ballini, A, Inchingolo, F, Luperto, P, et al (2020) The Human Respiratory System and Its Microbiome at a Glimpse. Biology (Basel) 9: 318.
141. Qureshi, I, Shahzad, M, Bashir, U, Jalbani, B.A, Memon, A.S, Shams, S. (2021) Comparison of Postoperative Bleeding with and without Discontinuing the Antiplatelet Drugs (Aspirin, Clopidogrel) after Tooth Extraction. Journal of Pharmaceutical Research International 2021: 145–151.
143. Sui, J, Devoize, L, Gonnu-Levallois, S, Mulliez, A, Baudet-Pommel, M, Barthélémy, I, Dang, N.P.(2015)[Retrospective study on bleeding and thromboembolic complications related to tooth extraction, in 93 patients usually treated by antithrombotic therapy]. Rev Stomatol Chir Maxillofac Chir Orale 116: 5–11.
144. Kalemaj, Z, Marino, M.M, Santini, A.C, Tomaselli, G, Auti, A, et al. (2022) Salivary microRNA Profiling Dysregulation in Autism Spectrum Disorder: A Pilot Study. Front Neurosci , 1:, 945278.
146. Morimoto, Y, Niwa, H, Minematsu, K. (2011) Risk Factors Affecting Postoperative Hemorrhage after Tooth Extraction in Patients Receiving Oral Antithrombotic Therapy. J Oral Maxillofac Surg 69: 1550–1556.
147. Villanueva, J, Salazar, J, Alarcón, A, Araya, I, Yanine, N, Domancic, S, et al (2019) Antiplatelet Therapy in Patients Undergoing Oral Surgery: A Systematic Review and Meta-Analysis. Med Oral Patol Oral Cir Bucal 24: e103–e113.
149. Rapone, B, Ferrara, E, Qorri, E, Dipalma, G, Mancini, A, Corsalini, M, Fabbro, M.D, Scarano, A, Tartaglia, G.M, et al (2022) The Impact of Periodontal Inflammation on Endothelial Function Assessed by Circulating Levels of Asymmetric Dimethylarginine: A Single-Blinded Randomized Clinical Trial. J Clin Med 11: 4173.
150. Cañigral, A, Silvestre, F.-J, Cañigral, G, Alós, M, Garcia-Herraiz, A, Plaza, A. (2010)Evaluation of Bleeding Risk and Measurement Methods in Dental Patients. Med Oral Patol Oral Cir Bucal 15: e863-868.
152. Nautiyal, M, Sekaran, K, Sekaran, S, Rengasamy, G, Veeraraghavan, V.P, et al (2023) Molecular Docking Analysis of Indole Based Diaza-Sulphonamides with JAK-3 Protein. Bioinformation 19: 74–78,
154. Gaballah, K, Hassan, M. (2022) Knowledge and Practice of Dentists Managing Patients on Antithrombotic Medications: A Cross-Sectional Survey. Eur J Dent 16: 775–780.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.