Anterior Cervical Spinal Cord Infarction from Cardioembolic Source Presenting with Respiratory Failure and Quadriplegia
by Shabna Mottemmal1, Adarsh Iyyavoo2, Nandakumar B Vittal3*,Pradumna P Singh3
1Residency Applicant, Kannur Medical College, Kerala, India
2High School Senior, Cambrian Academy, San Jose, California, USA
3Meharry Medical College at Nashville General Hospital; Nashville, TN 37208, USA
*Corresponding author: Nandakumar B Vittal, Associate Professor, Department of Internal Medicine, Division of Neurology, Meharry Medical College, 1005 Dr. DB.Todd Jr. Blvd, Nashville, TN-37208, USA
Received Date: 18 September 2023
Accepted Date: 22 September 2023
Published Date: 25 September 2023
Citation: Mottemmal S, Iyyavoo A, Vittal NB, Singh PP (2023) Anterior Cervical Spinal Cord Infarction from Cardioembolic Source Presenting with Respiratory Failure and Quadriplegia. Ann Case Report. 8: 1455. https://doi.org/10.29011/2574-7754.101455
Abstract
A 30-year-old man presented with acute respiratory distress, quadriplegia, and other neurologic symptoms, without evident cause on head CT. Subsequent brain MRI revealed bilateral cerebral infarcts, additionally cervical MRI showed T2 hyperintensity in the anterior spinal cord from C2-C6. There was no clear history of trauma and normal cerebral and cervical vascular imaging indicated no potential sources of vascular embolism. The patient’s acute presentation and atrial fibrillation suggests a cardiac source of thrombus for the cerebrospinal infarcts. The presented case of anterior spinal artery syndrome underscores the importance of considering stroke in acute neurological presentations, even with atypical symptoms.
Keywords: Respiratory Failure; Quadriplegia; Anterior Spinal Cord Infarction; Cervical Spinal Cord Infarction; Cardioembolism.
Introduction
Spinal cord infarction is not uncommon accounting for 1% of acute stroke hospitalizations [1]. Thoracic portion of the cord is involved mainly due to aortic pathologies and cardiac causes leading to systemic hypotension. Cervical anterior spinal cord infarct is rare and often caused by vertebral artery dissection related to trauma. Cardioembolic source is described for thoracic spinal cord infarct but not for cervical spinal cord infarct [2]. Symptoms in cervical spinal cord infarct can include sudden onset of severe neck pain, quadriparesis, sensory deficits, respiratory distress requiring mechanical ventilation, cardiac dysrhythmias and bowel or bladder dysfunction. Diagnosis involves medical history review, physical examination, and spinal cord and vascular imaging. MRI might not demonstrate the spinal cord infarct early on and imaging is done nonetheless to rule out other structural etiologies of myelopathy [3]. Treatment focuses on managing symptoms, mechanical ventilation and other supportive care measures while promoting rehabilitation. Prognosis depends on the location, extent of infarct and timeliness of the intervention [4,5]. Seeking immediate medical attention is crucial for proper diagnosis and appropriate management of spinal cord infarction. Many patients with spontaneous spinal cord infarct do not receive thrombolytics due to “atypical” presentation and lack of diagnosis that can be missed despite availability of spinal cord MRI imaging.
Case Report
We present the case of a 30-year-old previously healthy man who presented to the ER on a Sunday morning with acute onset difficulty breathing and weakness in his extremities. He spent most of Friday and Saturday with friends. Earlier that morning he had complained of neck pain and tingling in his hands, which prompted his roommate to bring him to the ER. He was able to walk into the ER, soon after he required assistance to stand up. He now reported, “I can’t move” and “I can’t breathe, I want oxygen”. This was followed by agitation, respiratory distress (Oxygen saturation at 31%) requiring intubation and mechanical ventilation. There was no history of trauma, recent surgical procedures, diabetes, hypertension, heart disease, other significant past medical conditions, and no recent travel history. His vital signs showed normothermia soon followed by hypothermia returning to normothermia (98-degree F; dropping to 94-degree F and 98-degree F over 3 hours), BP 160/98 (then 116/61; followed by 56 mm Hg systolic that improved with fluid boluses. Heart rate was 66/min and later 36/min improving to 80s (36-137 range); EKG showed alternating sinus rhythm and atrial fibrillation with rapid ventricular rate. On day 2 patient failed extubation due to very low tidal volume (80 ml). Chest CT did not show any pathology to explain respiratory failure. His exam revealed quadriplegia and this led to a neurology consultation. Neurological examination showed intact consciousness; he responded to loud verbal and physical stimulation with nods or head shaking. Eye movements initially showed dysconjugate gaze (this resolved in 24 hours), patient exhibited flaccid (0/5) quadriplegia, areflexia and down-going plantar response. He however managed to dislodge the endotracheal tube (ETT) with his tongue movements multiple times. He had normal sensation in his face; below his neck, he had decreased sensation to temperature and pain, but intact light touch and proprioception. Head CT did not show any acute abnormalities. Other investigations on admission revealed normal CBC, CMP; urine drug screen was positive for THC and negative for stimulants, blood EtOH level was < 3. Additional tests included CSF analysis with cell count of 7, normal protein and glucose. CSF culture later came back negative, and he had a normal sed rate (ESR). Brain MRI revealed numerous subcentimeter bilateral cerebellar, posterior temporal and occipital embolic infarcts (Figure 2 A- 2E and Figure 3). Magnetic Resonance Imaging of the cervical spine showed T2 hyperintensity in the territory of the anterior spinal artery extending from C2 to C6 (Figure 1). MRA of the head and neck were normal (Figure 4A and 4B). Transthoracic Echocardiography showed normal ejection fraction, no intracardiac structural abnormalities and no right to left shunt. Transesophageal echocardiography did not reveal any abnormalities in the proximal aorta. CT angiography of head and neck done few days later was normal as well indicating no occlusions or dissections (Figure 5A-5E). He received 1-gram intravenous solumedrol daily for five days based on initial cervical MRI findings in addition to aspirin started after MRI showed acute infarcts. His CSF also showed 14 oligo clonal bands (unclear significance likely secondary to acute ischemia). Hospital course – On day 3 he went into neurogenic shock and multiple episodes of vasovagal bradycardia (HR in the 40s) and demonstrated hemodynamic instability when he was being moved by nursing staff. His exam now showed intact cognition and normal cranial nerve examination. He developed ileus and had frequent episodes of bradycardia (Figure 6), fluctuating blood pressure all part of autonomic dysfunction causing the nurses to panic. He required transvenous pacemaker which was soon replaced with permanent pacemaker. After four weeks his tidal volume improved from 80 ml to 240 ml., he started to regain significant strength in his lower extremities to the point where he was able to stand up and walk up to 25 feet when his vital signs permitted. His upper extremities remained flaccid, areflexic except for his ability to close his hands to gently squeeze a soft ball. Repeat labs including spinal fluid showed similar findings including 14-oligoclonal bands, normal cell count, protein, and glucose. West Nile virus IgM, HTLV-1, HIV, HSV and CSF VDRL testing were all-negative. After eight weeks, his autonomic instability continued to improve and so did his participation in physical therapy sessions. He could now ambulate up to 100 feet using a special walker; however, he remained flaccid in his upper extremities and continued to need intermittent daily ventilator support due to tidal volume at ~300ml. Repeat MRI of his brain and spinal cord was placed on hold due to his pacemaker that requires many weeks for lead maturation.
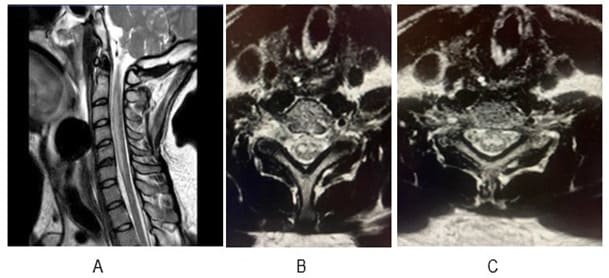
Figure 1A: MRI Cervical spine - Sagittal T2 sequence showing hyperintensity from C2 to C6 in the anterior portion of the spinal cord (ACA territory). Figure-1B and 1C are axial sections showing lesion in the grey matter region (Owl’s eye appearance).
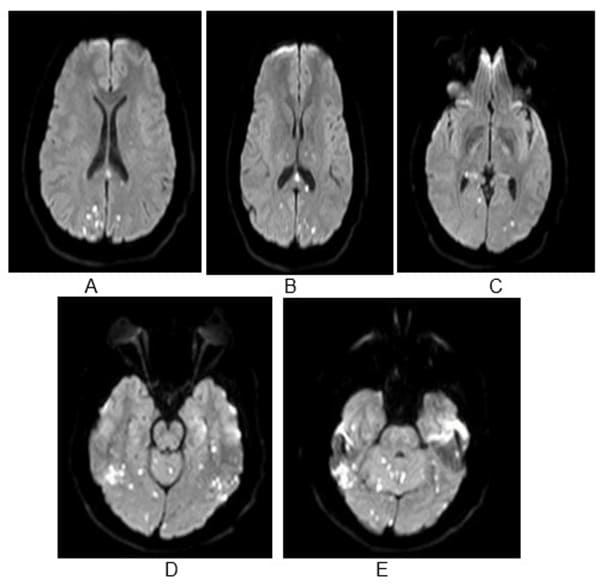
Figure 2A-E: MRI Brain – Diffusion sequence showing bilateral punctate restricted diffusion; A and B - parietal and occipital infarcts, B-E - Occipital infarcts, D and E – bilateral cerebellar infarcts.
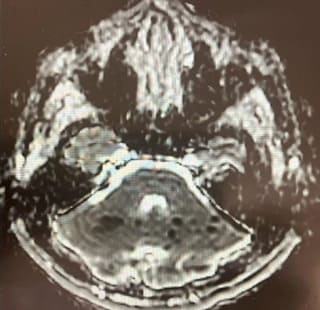
Figure 3: Shows corresponding ADC sequences showing hypointense/ darker regions suggesting acute ischemic infarcts.
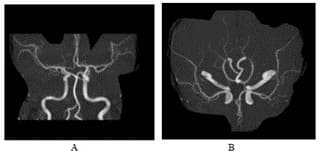
Figure 4: MRA head shows intact vasculature, no evidence of stenoses or obvious dissection.
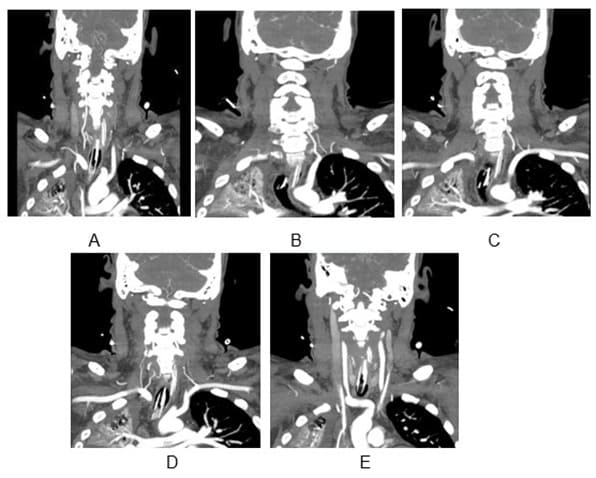
Figure 5A: 5E-CTA neck done few days later showing intact vasculature.
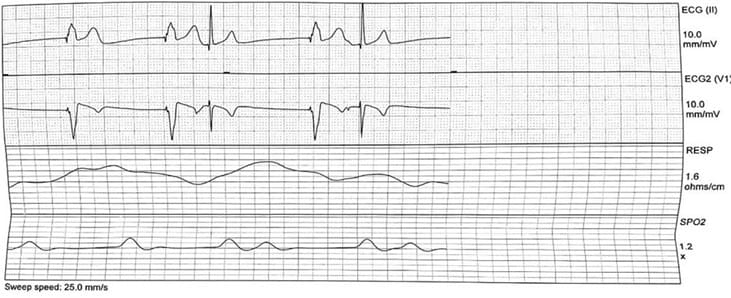
Figure 6: EKG rhythm strip-showing bradycardia during patient neck movement.
Discussion
Anterior spinal artery syndrome of the cervical spinal cord can be devastating due to respiratory failure and quadriplegia. In younger otherwise healthy patients, it is usually the result of vertebral artery dissection from trauma. It can occur in patients with systemic hypotension from various causes such as cardiac arrest. Cardio embolic infarction of the spinal cord is reported in literature however mostly in the thoracic region of the cord. Here we report a patient with anterior spinal artery infarct in the cervical region with intact extra cranial vasculature. Early symptoms of neck pain and paraesthesia’s in the extremities indicate the neurological localization to the cervical spinal cord. Dysconjugate gaze that resolved soon after is likely explained by bilateral posterior circulation acute infarcts. Cervical spinal cord and bilateral posterior cerebral infarcts in the context of atrial fibrillation indicates most likely cardiac source of thrombus despite negative echocardiographic findings. There was no evidence of vertebral or aortic dissection, spinal cord trauma, and antecedent hypoperfusion secondary to cardiac dysrhythmia before symptom onset (where patients are found down), vascular malformations, vasculitis, autoimmune diseases, or complications from surgical procedures. Apart from the atypical source of embolization for the cervical spinal cord infarct, our case is typical in terms of initial presentation of spinal cord infarcts hyper acute to acute presentation (< 6 hours), acute phase of spinal cord injury -first four weeks of hospital course with severe autonomic dysfunction plateauing thereafter and notable recovery in respiratory function and lower extremity strength. Prolonged recovery states are reported for spinal infarcts beyond the typical 6-12 months for cerebral infarcts. Persistent severe weakness and ventilator dependent state also is typical in high cervical lesions, and hence our patient will likely require extensive rehabilitation and dedicated potentially lifelong nursing care. To summarize the different types of spinal cord infarction based on vascular supply are anterior cord syndrome, posterior cord syndrome, central cord syndrome, and Brown-Séquard syndrome. Due to its long length the spinal cord it is supplied by various arteries at different segments. The cervical spinal cord receives blood from the vertebral arteries, ASA and PSAs. The thoracic spinal cord is supplied by segmental arteries from the aorta. The lumbar spinal cord is nourished by the arteria radicular is magna anterior (also known as the artery of Adamkiewicz) and additional lower lumbar arteries. The sacral spinal cord is supplied by segmental arteries as well. Collateral circulation through anastomoses between these arteries ensures continuous blood flow. The cardiovascular response to Spinal Cord Injury or infarction in this case is divided into two phases: the acute phase occurs immediately and lasts up to four weeks, and the chronic phase starts 2-6 weeks from the event and can last for prolonged periods. In the acute phase of SCI, sinus bradycardia, characterized by a slow heart rate due to parasympathetic predominance, is the primary abnormality. This condition is more prevalent in cases of higher-level injuries like in our patient. Sinus arrests often occurred sometimes multiple times in a day leading to asystole. Cardiac arrest and the need for cardiopulmonary resuscitation (CPR) are most likely to happen within the first 2-4 weeks of SCI, and fatal outcomes can occur due to asystolic arrest. Common triggers for severe bradycardia during the acute recovery period of SCI include tracheal suctioning, hypoxia, repositioning of the patient, or can happen even without any apparent cause. Managing survivors of SCI primarily involves preventing and treating Bradyarrhythmias. Intravenous administration of atropine and methylxanthines are the main drugs used for treatment and prophylaxis. When medical therapy fails, pacemaker implantation becomes necessary, especially in cases of higher-level cervical cord injuries (above C5/C6). Additionally, in the acute phase of severe SCI, sympathetic withdrawal can lead to neurogenic shock, characterized by low blood pressure (systolic blood pressure less than 90 mmHg) and bradycardia (heart rate less than 60 bpm). This condition has a poor prognosis, and treatment involves intravenous administration of colloid fluids and/or vasopressors to maintain a target mean arterial pressure of 80-90 mm Hg within the first week of injury, aiming to prevent further ischemic damage to the spinal cord. The diagnosis of spinal cord infarction involves a combination of methods including medical history, physical examination, imaging studies, and diagnostic tests. Magnetic Resonance Imaging (MRI), though not necessary for diagnosis provides detailed images of the spinal cord and surrounding structures, allowing visualization of ischemic changes, infarcted areas, and potential causes of spinal cord infarction and more importantly rules out other structural etiologies causing cord compression [6,7].
Conclusion
Stroke is a common neurological problem and in the acute state patients present to the emergency room; overtime most emergency room physicians and stroke neurologists would encounter unusual presentations of stroke. Hence it is important to consider stroke as an etiological diagnosis in patients presenting with acute onset of neurological symptoms however atypical. Appropriate clinical context and a normal cervical MRI should remind us of the limitations of the study techniques rather than disregard the possibility of stroke. Knowledge of neuroanatomy is important to localize the lesion and particularly knowledge of neurovascular anatomy is critical in determining the event as a vascular event. Committing patients to long-term anticoagulation without an obvious source of cardiac embolization at the same time no alternative explanation for the mechanism of stroke can be challenging management dilemma. In patients with high risk for falls, one could justify holding off anticoagulation. Finally due to the rarity of spinal cord infarctions of the cervical region clinical trials are unlikely. Knowledge of how to investigate and manage these patients must come from detailed case studies as we have attempted here. We hope future detailed case reports should help us formulate protocols to facilitate thrombolytic therapy for this under recognized category of spinal cord infarcts.
Acknowledgements: Anish Iyyavoo (Sophomore -BioEngineering, UC Berkeley College of Engineering, Berkeley, CA) for manuscript writing provided edits of multiple drafts of data acquired by authors by 1, 2, 3 and 4. Author roles
- Author 1 - Initiated the idea and gathered initial data and provided initial draft/s
- Author 2 - gathered initial clinical data and provided initial draft, participated in manuscript writing with author 1.
- Authors 3 & 4 – edited manuscript for intellectual content.
Ethical Considerations: Written patient consent was obtained for this case report publication, available with corresponding author. (Patient unable to write due to hand weakness, placed an “x” in place of signature)
Conflict of Interest: All authors report no conflict of interest.
References
- Rubin M N, Rabinstein AA (2013) Vascular diseases of the spinal cord. Neurol Clin. 31: 153-81.
- Pikija S, Mutzenbach JS, Kunz AB, Nardone R, Leis S, et al (2017) Delayed Hospital Presentation and Neuroimaging in Non-surgical Spinal Cord Infarction. Frontiers in Neurology, 8.
- Masson C, Pruvo JP, Meder JF, Cordonnier C, Touzé E, et al (2004) Spinal cord infarction: clinical and magnetic resonance imaging findings and short term outcome. J Neurol Neurosurg Psychiatry. 75:1431-5.
- Hsu JL, Cheng M, Liao M, Hsu H, Weng Y, et al (2019). The etiologies and prognosis associated with spinal cord infarction. Annals of Clinical and Translational Neurology, 6: 1456–1464.
- Salvador de la Barrera S., Barca-Buyo A., Montoto-Marqués A., Ferreiro-Velasco M., Cidoncha-Dans M, et al (2001). Spinal cord infarction: prognosis and recovery in a series of 36 patients. Spinal Cord, 39: 520–525.
- Zalewski NL, Rabinstein A. A, Krecke K. N, Brown R. D, Wijdicks E. F. M, et al (2019). Characteristics of Spontaneous Spinal Cord Infarction and Proposed Diagnostic Criteria. JAMA Neurology, 76: 56.
- Nichtweiß M, S Weidauer S (2015) Differential Diagnosis of Acute Myelopathies: An Update. Clin Neuroradiol. 25: 183-7.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.