An Unusual Case of Intensive Acute Abdominal Pain Caused by Non-Perforated Jejunal Diverticulitis
by Robert Kliček1,4, Ana Andrilović1, Karolina Krstanac2, Arijana Pačić2, Adrijana Perkunić3, Josipa Petrović3
1Department of Abdominal Surgery, Clinical Hospital “Dubrava”, Zagreb, Croatia
2Department of Pathology and Cytology, Clinical Hospital “Dubrava”, Zagreb, Croatia
3Department of Radiology and Invasive Radiology, Clinical Hospital “Dubrava”, Zagreb, Croatia
4School of Medicine, University of Zagreb, Zagreb, Croatia
*Corresponding author: Robert Kliček, Department of Abdominal Surgery, Clinical Hospital, “Dubrava”, Zagreb, Croatia, School of Medicine, University of Zagreb, Zagreb, Croatia
Received Date: 18 December 2024
Accepted Date: 23 December 2024
Published Date: 26 December 2024
Citation: Klicek R, Andrilovic A, Krstanac K, Pacic A, Perkunic A, et al (2024) An Unusual Case of Intensive Acute Abdominal Pain Caused by Non-Perforated Jejunal Diverticulitis. Ann Case Report. 9: 2136. https://doi.org/10.29011/2574-7754.102136
Abstract
We report a case of a 65-year-old female patient admitted to the hospital due to sudden acute abdominal pain. Laboratory results revealed leukocytosis and multislice computed tomography revealed free intraabdominal liquid in the left upper quadrant among jejunal loops. An urgent laparotomy was performed, and jejunal diverticulitis was found without signs of perforation. The part of the affected jejunum was resected with jejunal primary anastomosis. The patient recovered well and was discharged home on the 5th postoperative day. The gastrointestinal assessment revealed no inflammatory bowel disease during follow-up, and the symptoms did not reoccur. Two years later, the patient underwent a postoperative ventral hernia repair. Jejunal diverticulitis is less common than diverticular colon disease. However, it may cause acute abdominal pain due to bleeding and perforation. To this date jejunal diverticulitis was not presented as the cause of acute abdominal pain without perforation.
Keywords: Jejunal Diverticulitis; Acute Abdominal Pain; Perforation; Diverticular Disease.
Introduction
Jejunal diverticulitis is less common than diverticular colon disease and usually presents with nonspecific symptoms. Complications include acute intestinal obstruction, bleeding, and mainly perforation with localized or generalized peritonitis [1,2].
There have been no reported cases of jejunal diverticulitis without perforation as the cause of acute abdominal pain.
We report a case of a 65-year-old female patient who presented with an acute abdomen with intermittent obstruction and without any signs of perforation or bleeding. The indication for surgical exploration was set due to the finding of some free fluid surrounding the jejunum and suspected acute appendicitis on MSCT, along with the clinical asset of the acute abdomen (Figures 1&2).
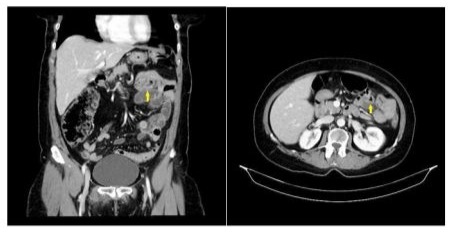
Figure 1: Inflammatory changes surrounding jejunum.
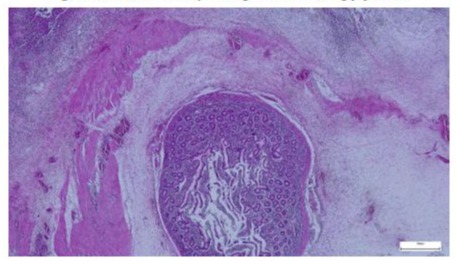
Figure 2: H&E 25× Small bowel diverticulum is seen here as an outpouching of the small bowel mucosa in the subserosal adipose tissue. Active inflammation is seen in the diverticular wall and in the surrounding tissue.
Case Report
A 65-year-old female presented to the emergency department with severe pain in the periumbilical region, with pain radiating to both lateral sides and in the upper abdomen. The patient didn’t have nausea, and she passed a normal stool two hours before the onset of pain. Past medical history included problems with the spine, hysterectomy with bilateral salpingectomy, and cholecystectomy. On physical examination, her abdomen was painful and diffusely tender, with signs of peritonitis. The auscultation bowel sounds were positive. Her vital signs were a temperature of 37.9 C (rect) and 37.1 C (ax), blood pressure of 120/80 mmHg, heart rate of 75 beats per minute, and oxygen saturation of 98%.An urgent MSCT of the abdomen showed free fluid surrounding a segment of the jejunum and suspected initial phase of appendicitis. The patient underwent a laparotomy, which showed the presence of two diverticula with active inflammation seventy centimeters distal to the Treitz ligament. Twenty-five centimeters of jejunum were resected, and a termino-terminal anastomosis was created. After that, an appendectomy was performed. Histopathology later confirmed the diagnosis of diverticulitis with inflammatory infiltrate, and the appendix was free of inflammation. The postoperative period went without any complications, and the patient went home with instructions for taking antibiotics for the next five days.
Discussion
Small bowel diverticula occur in the duodenum in 79%, in the jejunum or ileum in 18%, and in all three segments in 3%, and 60% of patients with small bowel diverticula have concurrent colonic diverticula [3,4]. Compared to the diverticulosis of the colon, jejunal diverticulitis is a rare disease with a prevalence of 0.06% -1.3% [5]. It mainly affects the population between 60- and 70-years years of age [6]. Furthermore, the occurrence of the disease is more frequent in men than in women. Various studies have shown that the disease itself has many complications that may be fatal to the patient, such as malabsorption, obstruction, gastrointestinal bleeding, and at the end of peritonitis development, perforation. Up to 30% of the cases of jejunal diverticulitis develop complications requiring surgical interventions. The mechanism of diverticulitis is associated with increased intraluminal pressure, peristaltic dysfunction, and other factors that lead to weak areas. Diverticulitis localization within the small intestine is largest in the proximal jejunum, with 75%, then in the distal jejunum (20%) and at the end of the ileum, at 5%. The symptoms themselves are mostly unspecific and vary from abdominal pain, constipation, and diarrhea to sometimes severe acute episodes with intra-abdominal abscesses and perforations [5]. In the diagnostic procedure, radiographic methods are mainly used to exclude perforation. Also, ultrasound is a method of detecting diverticulitis of the jejunum, but it has some limitations, such as adiposity or meteorism. Today, the main preoperative examination is abdominal MSCT [7], which can display the wall thickness typical in patients with diverticulitis. Due to the inflammation of the surrounding mesentery, small collections of free fluid can be accumulated [8,9], as is evident in the report. If the patient is hemodynamically stable with localized peritonitis, non-surgical treatment with antibiotics is desirable, although it does not prevent recurrences [10]. However, if peritonitis has spread to the other structures, the indication for laparotomy and primary anastomosis is given as it was performed in our patient. The other complications may include acute intestinal obstruction, diverticular bleeding and bowel perforation [11]. We performed the resection of the small bowel with the inflamed diverticula, although there were no signs of perforation, in order to achieve higher rate of survival and better outcomes as it is suggested in literature [12] Diagnosing complicated jejunal diverticulosis is complex and sometimes not accurately established, even by enhanced CT scan which indicates surgical diagnostic laparotomy before severe complications develop [13]. Symptomatic diverticula are associated with a higher rate of complication than those found accidentally [14].
Conclusion
Jejunal diverticulitis is a condition that should be considered in patients with acute abdominal clinical assets without specific proof of the cause. Since the establishment of diagnosis might be challenging, we need to consider the surgical exploration in order to avoid the development of complications.
References
- Chendrasekhar A, Timberlake GA. (1995) Perforated jejunal diverticula: an analysis of reported cases. Am Surg.61:984.
- Novak JS, Tobias J, Barkin JS. (1997) Nonsurgical management of acute jejunal diverticulitis: a review. Am J Gastroenterol. 92:1929.
- Akhrass R, Yaffe MB, Fischer C, Ponsky J, Shuck JM (1997) Smallbowel diverticulosis: perceptions and reality. J Am Coll Surg.184:383.
- Transue DL, Hanna TN, Shekhani H, Rohatgi S, Khosa F, et al (2017) Small bowel diverticulitis: an imaging review of an uncommon entity. Emerg Radiol. 24:195.
- Shahjehan A, Atif R, Rayyan P (2014) Jejunal diverticulitis: imaging to management Ann Saudi Med 34: 87-90
- Fang M, Agha S, Lee R, Culpepper-Morgan J, D’Souza A. (2000) Perforation of jejunal diverticulum: case report and review of literature. Conn Med. 64:7–10.
- Ceuppens AS, Dhont S, Sneyers B, Schepers C, Ramboer K, et al (2018) Jejuno-ileal diverticulosis: a review of literature. Acta Gastroenterol Belg. 281:517-519.
- Lebert P, Ernst O, Zins M. (2019) Acquired diverticular disease of the jejunum and ileum: imaging features and pitfalls. Abdom Radiol (NY). 44:1734.
- Chapman J, Al-Katib S, Palamara E. (2021) Small bowel diverticulitis - Spectrum of CT findings and review of the literature. Clin Imaging. 78:240.
- Kassir R, Bouiel-Bourilier A, Baccot S, Abboud K, Dubois J, et al. (2015) Jejuno-ileal diverticulitis: Etiopathogenicity, diagnosis and management. Int. J. Surg. Case Rep., 10: 151-153.
- Sinclair A. (2017) Diverticular disease of the gastrointestinal tract. Prim. Care Clin. Office Pract., 44: 643-654
- Mansour M, Abboud Y, Bilal R, Seilin N, Alsuliman T, et al (2022) Small bowel diverticula in elderly patients: a case report and review article. BMC Surg. 22:101.
- Chiorescu S, Mocan M, Santa ME, Mihăileanu F, Chiorescu RM. (2024) Acute complicated jejunum diverticulitis: a case report with a short literature review. Front Med (Lausanne). 11:1413254.
- Yoon YS, Park IJ, Lee KH, Kim HC, Yu CS, et al (2004) Should small bowel diverticula be removed?]. Korean J Gastroenterol. 44:275.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.