An Innovative LASER-Suction-Y Connecting (LASY) System: Readily Available and Reproducible Technique, Perfect Tool for Single Handed Endoscopic Ear Surgery
by Wai Tsz Chang1,2* Ricky Chin1, Horace Cheng1,3, Kary Lui Choi Mui1,4, Xiaoxin Chen1, Michael Chi Fai Tong1,2
1Department of Otorhinolaryngology, Head and Neck Surgery, The Chinese University of Hong Kong, Hong Kong
2Institute of Human Communicative Research, The Chinese University of Hong Kong, Hong Kong
3Department of Ear Nose and Throat, Prince of Wales Hospital, Shatin, Hong Kong
4Department of Ear Nose and Throat, United Christian Hospital, Kwun Tong, Hong Kong
*Corresponding author: Wai Tsz CHANG, Department of Otorhinolaryngology, Head and Neck Surgery, Prince of Wales Hospital, 30-32 Ngan Shing Street, Shatin, NT, Hong Kong
Received Date: 09 June 2025
Accepted Date: 27 June 2025
Published Date: 01 July 2025
Citation: Chang WT, Chin R, Cheng H, Mui KLC, Chen X, et al. An Innovative LASER-Suction-Y Connecting (LASY) System: Readily Available and Reproducible Technique, Perfect Tool for Single Handed Endoscopic Ear Surgery. J Surg 10: 11371 https://doi.org/10.29011/2575-9760.011371
Abstract
Objective:To explore the feasibility and learning curve of assembling an innovative single-handed LASER- Y connecting (LASY) suction system in endoscopic ear surgery.
Study Design:A prospective, multicentered study, 43 nurses and doctors from Hong Kong attempted to assemble the innovative single-handed LASER suction system.
Setting:University-affiliated tertiary referral centres in Hong Kong, including Prince of Wales Hospital, Alice Ho Miu Ling Nathersole Hospital, Tseung Kwan O Hospital and United Christian Hospital.
Main Outcome Measures:Description of the techniques for imitating the system. The objective time required and the subjective assessment of the degree of difficulty in assembling the device were measured.
Results:Of the 43 participants, 34 are nurses and 9 are doctors. They have different lengths of professional experience, 12 with <5 years, 15 with 5-10 years, and 16 with >10 years. The mean time to set up the device for the first time was only 109.9 seconds (less than 2 minutes), and the time used is negatively correlated with the experience of assembling (r = -0.375). The learning curve was so steep that they were able to reach the plateau of only 60 seconds the third time they set up the system. 81% of participants considered setting up the system to be very easy or easy and 0% difficult or very difficult. There was no statistically significant difference in the time taken by nurses and doctors to set up the system (p > 0.05). There was no statistically significant difference in the time required for participants with different levels of professional experience (p > 0.05).
Conclusion:Our innovative single-handed LASER-suction-Y connecting (LASY) system is easy to setup, easily reproducible with a steep learning curve of 3 time of setting up the system and very short set up time of 60 seconds. For users who found the chopsticks technique too difficult to learn and use, it is a good applying LASER single handed in endoscopic ear surgery.
Background
The microscope has long played an essential equipment for ear surgery. Recently the adaptation of Endoscopic Ear Surgery (EES) has become more popular. Not only does the endoscope provide a wider field of view, but it also allows surgeons to look around corners during surgery, making it more suitable for a small, complex structure such as the ear. Clinical
studies have also shown that the surgical results of EES in various type of otological operations are comparable to those of using a microscope [1-3]. The history of EES can be traced back to three decades ago [4]. Cohen et al. proposed a classification system of three waves on the use of endoscopy in otology [5]. The first wave (Cohen class 1) was about an endoscope used for inspection without dissection. It mainly described the diagnostic and documentary aspects of the endoscope. Nomura demonstrated the use of an endoscope in the examination of the middle ear in 1982. [6] The second wave (Cohen class 2) was mixed dissection, in which an endoscope was used as part of the dissection. Here, the endoscope was used as an aid adjunct to the microscopic removal of the disease. An example of this was Badr-el-Dine, who demonstrated the value of an endoscope in cholesteatoma surgery [7]. The third wave (Cohen class 3) was about ourely endoscopic procedures. It demonstrated the use of an endoscope as the main workhorse for ear surgery.
As early as 1992, Dr. El-Guindy from Egypt had increased the likelyhood of using endoscope in performing myringoplasty [8]. Nowadays, the endoscope is increasingly used for various type of ear surgeries such as cholesteatoma surgery [7], endoscopic tympanoplasty [9], endoscopic stapedotomy, and ossiculoplasty etc. [10, 11].However, EES also has its problems. During EES, the operating surgeon must use one hand to hold the endoscope, which means that only one hand is available to hold the instruments [12]. This inevitably increases the operating time and the risk of possible complications by frequent switching of instruments. Functional endoscopic sinus surgery was introduced earlier than EES and encountered the same obstacles during its development. During FESS, when involves heavy bleeding that impairs vision of the surgeon, or when the tissue needs to be held under tension so that it can be dissected cleanly, it is always best to use both hands. The bimanual technique, involving two trained endoscopists was proposed early on to solve this problem [13].
More recent development is the use of an endoscope holding arm so that only one trained endoscopist is needed during the surgery [14]. However, it is still challenging to develop a holder with sufficient accuracy and effectiveness for use in middle ear surgery [13]. Several endoscopic instruments have been modified for use in ESS meanwhile [15].Surgeons have been using the LASER in microscopic ear surgery for long [16-19]. It has enabled hemostasis and non-contact ablation of tissue. Nowadays, there are also more and more established roles for LASERs in the EES era [20]. Although LASERs are undoubtedly excellent tools in EES, there are many challenges in applying this technique in EES given the fact that only one hand is available. In common practice, the use of smokegenerating devices such as LASER and diathermy requires suction to ensure a good view of the surgical field. Also, minor bleeding might still be encountered during LASER application that prevent the application of further LASERs. Suction is needed during the whole procedure.
But in the situation where one hand is occupied with an endoscope, it is difficult to use LASER and suction at the same time. In single-handed endoscope-guided surgery, an assistant would most often need to hold a sucker in the meatus. Either inefficient suctioning of the smoke or there is an increased risk of the suction device accidentally advancing into the stapes [15]. The single-handed LASER-suction system with suction was first described in 2006 [21] and was developed to avoid such a scenario. It is similar to the concept of suction diathermy, where one device contains both diathermy and suction functions. Yet, the device was very bulky that cannot be fit into the ear canal. This time, we can build this simple device ourselves instead of using a prefabricated production from the manufacturers. It is a device made from readily available materials and can be easily constructed even by inexperienced hands. Considering the short time required to train and build the device, there is no doubt that it can be easily out into practice.
Description of Technique
The innovative Single-Handed LASER-suction-Y connecting (LASY) System. To build the instrument for the single-handed LASY system, only simple instruments that are commonly seen in an operating theatre were needed. That include a plastic or Silicon suction catheter, an 18-gauge (for 300mm LASER fiber) or 16-gauge (for 400mm LASER fiber) intravenous (IV) cannula, a disposable Zoellner suction tube, a fine tip of 18-gauge and a LASER device with LASER fiber (the TruBlue LASER system is used here for demonstration).
The intravenous (IV) cannula (here we use the 18-gauge for demonstration) is inserted into the plastic suction tube towards the end attaching to the Zoellner suction tube and withdraw the introducer.
Leaving the plastic cannula inside the suction tube (Figure 1).
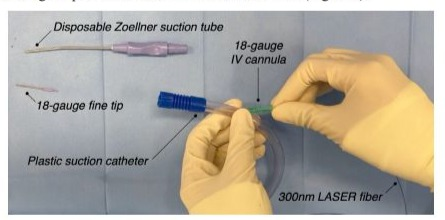
Figure 1:The intravenous (IV) cannula (here we use the 18-gauge for demonstration) is inserted into the plastic suction tube towards the end attaching to the Zoellner suction tube, and withdraw the introducer. Leaving the plastic cannula inside the suction tube.
The LASER fiber (here we use 300nm LASER fiber for demonstration purposes) is inserted into the lumen of the suction tube via the IV cannula. Continue to advance the fiber, until approximately 20 cm of the fiber emerges from the funnel port (Figure 2).
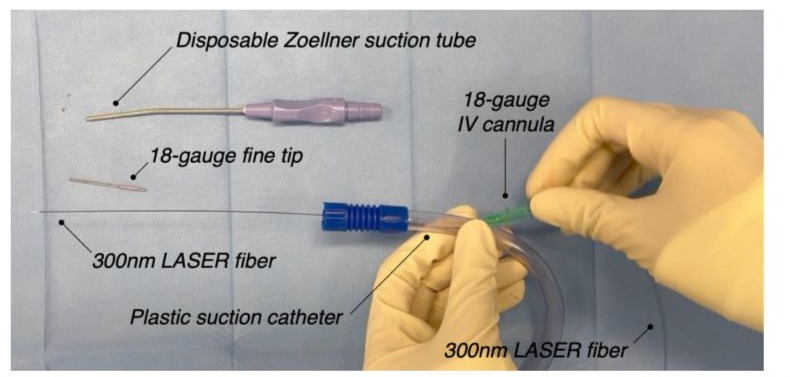
Figure 2: The LASER fiber (here we use 300nm LASER fiber for demonstration purposes) is inserted into the lumen of the suction tube via the IV cannula. Continue to advance the fiber, until approximately 20 cm of the fiber emerges from the funnel port.
Gradually insert the disposable Zoellner suction tube, thread the fiber and then the fine tip of 18-gauge along the LASER fiber like a guide wire and connect it to the funnel connector. Adjust the length of the exposed laser fiber to about 3 mm from the fine tip to facilitate suctioning of blood and fluid (Figures 3,4) showed the intraoperative view when applying this LASY system.
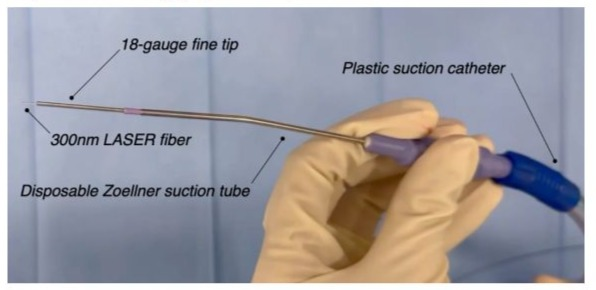
Figure 3: Gradually insert the disposable Zoellner suction tube, thread the fiber and then the fine tip of 18-gauge along the LASER fiber like a guide wire and connect it to the funnel connector. Adjust the length of the exposed laser fiber to about 3 mm from the fine tip to facilitate suctioning of blood and fluid.
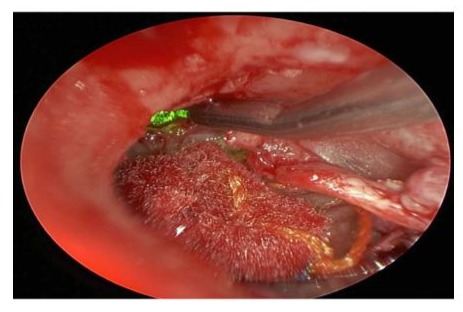
Figure 4: Intraoperative view of using the LASER-suction system.
Methods
In this a multicentered prospective study in 4 different university-affiliated tertiary hospitals in Hong Kong, including Prince of Wales Hospital, Alice Ho Miu Ling Nathersole Hospital, Tseung Kwan O Hospital and United Christian Hospital. From April 2023 to October 2023, doctors and nurses from the operating room were recruited for the study. The first author demonstrated the assembly techniques to the staff. They were given questionnaires to complete, in which they were asked to state their professional experience of between 1 and more than 10 years. They were either assembling the device for the first time or only had some experience of assembling instruments. The entire process was staggered over time and the level of difficulty of assembly was rated on a scale of very easy, easy, moderately difficult, difficult and very difficult.
Results
43 healthcare professionals, including 34 nurses and 9 doctors, were included in the study. 12 (27.9%) of them who have less than 5 years of experience, 15 (34.9%) have 5-10 years of experience and 16 (37.2%) had more than 10 years of experience (Table 1).
|
Health professions |
N (%) |
|
Nurses |
34 (79.1%) |
|
Doctors |
9 (20.9%) |
|
Working experience |
|
|
<5 years |
12 (27.9%) |
|
5-10 years |
15 (34.9%) |
|
>10 years |
16 (37.2%) |
Table 1. Characteristics of the Health Professionals
The mean time to set up this device for the first time was only 109.9 seconds (less then 2 minutes) and the time to set-up dropped significantly with experience (Table 2).
| Number of time(s) in assembling the device | Mean time (s) |
|---|---|
| 1st time | 109.9 ± 34.8 |
| 2nd time | 82.4 ± 21.6 |
| 3rd time | 60.7 ± 18.2 |
| 4th time | 66 ± 16.5 |
| 5th time | 51.2 ± 20.1 |
Table 2: Mean time used to assemble the single-handed LASER-suction system
The results show a steep learning curve for setting up the device (Figure 5)
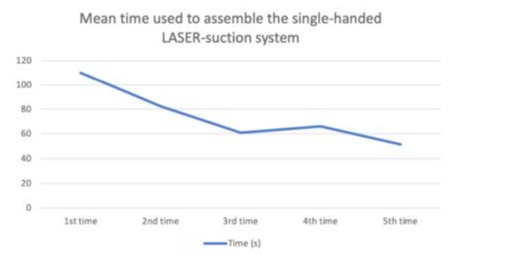
Figure 5: The mean time to set up the device decreases significantly with experience
As the mean time for the 3rd time assembling the device dropped to 60.7 seconds (1 minute). From the 3rd time onward, the curve begins to plateau and kept the average time to finish setting up at around 1 minute. 35 (81%) of the participants considered it easy or very easy, the remaining 8 (19%) considered it moderately difficult and none of them think it was difficult or very difficult (Figure 6).
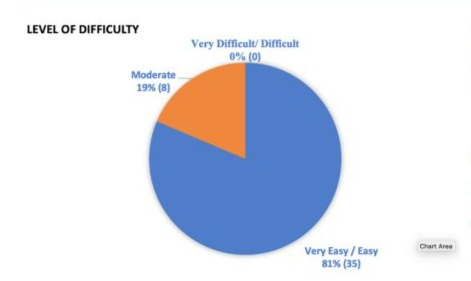
Figure 6: Most participants found it is very easy / easy to set up the device, and none of them deemed it as difficult.
The time used to set-up the device by nurses and doctors was compared. The mean time for nurses and doctors to assemble is 88.8 seconds and 77.3 seconds respectively. Independent t test was performed to compare the time used, but it did not show a statistically significant difference (p < 0.05) (Table 3).
| Professions | N | Mean | S.D. | P value |
|---|---|---|---|---|
| Nurse | 34 | 88.79 | 59.618 | 0.52 |
| Doctor | 9 | 77.33 | 54.975 |
Table 3: Mean and standard deviation of time used to assemble the singlehanded LASER-suction system by nurses and doctors respectively.
The time used by participants with different durations of working experience was also compared. The mean time for participants with <5 years, 5-10 years, and >10 years is 111.1 seconds, 85.7 seconds, and 68.5 seconds respectively. One-way analysis of variance was performed to compare the time used, but it did not show a statistically significant difference as well (p < 0.05) (Table 4).
|
Number of years of working experience |
N |
Mean |
S.D. |
P value |
|
<5 years |
12 |
111.08 |
59.479 |
0.161 |
|
5-10 years |
15 |
85.73 |
71.386 |
|
|
>10 years |
16 |
68.5 |
36.244 |
Table 4: Mean and standard deviation of time used to assemble the single-handed LASER-suction system by participants of different years of working experience.
Discussion
Given the limitations of the EES, many new techniques have emerged to solve the problem of single-handed operation.The four-handed technique requires two surgeons to operate together. If the chief surgeon wants to use the LASER, the assistant must be ready for the suction at the same time and place it precisely. This method requires a high degree of communication and cooperation between the chief surgeon and the assistant. In addition, with a limited working area in the ear canal, even a slightly unfavourable position of the suction catheter would block the surgeon’s field of vision. The frequent movement back and forth would greatly increase the risk of unnecessary bleeding, even if the suction catheter is placed outside when not in use. It is an inefficient technique. Therefore, a very experienced assistant is required for the procedure.The chopsticks technique is another emerging technique in EES [21]. This technique requires only one hand and does not require any modifications to the instrument. In this case, two instruments, a LASER and a suction catheter, are held in the hand as when using chopsticks. The chopstick technique also allows some fine movements. The instruments can be held together to pick bone and tissue, and they can also be spread open to dissect the tissue. Although it seems to be a perfect solution for EES, it also has its limitations. It requires good coordination between the fingers, precise positioning and the use of force to control the two instruments well. In addition, when used on a distal target, there would be a narrow angle between the two instruments, which limits the range of movement of the instruments distally. All in all, this would be a technique more suitable for daily chopstick use. For this innovative single-handed LASY system, only the most important equipment was required for the setup. All essential equipment was readily available in the operating room. In this prospective study, we showed that the time required to set up the device was minimal, with only 2 minutes needed even for the first use. It has been shown that the learning curve is very steep and only reaches a plateau at around 1 minute on the third application, regardless of the experience of the staff. It is indeed very easy to learn and none of the participants found the system difficult to set up.Compared to the four-handed technique, only one surgeon is required for this procedure. This shows that this single-handed device helps to save manpower and improve the efficiency of the surgery. Unlike the chopstick’s technique, surgeons do not need to learn new skills for this technique. They can simply use it as they have done before. However, with the chopstick’s technique, different combinations of instruments can easily be used, e.g. two dissectors, a burr and suction, whereas with the technique described here, only LASER and suction can be used. The use of this technique in various ear procedures needs to be investigated further.
Conclusion
Our innovative single-handed LASY system is easy to setup, easily reproducible with a steep learning curve of 3 time of setting up the system and very short set up time of 60 seconds. For users who found the chopsticks technique too difficult to learn and use, it is a good applying LASER single handed in endoscopic ear surgery.
Conflict of interest
The TruBLUE LASER fibers and the publication fee is sponsored by the Wetech Engineering & Technology Ltd. ARC Laser GmbH.
References
- Presutti L, Marchioni D, Mattioli F, Villari D, Alicandri-Ciufelli M (2008) Endoscopic management of acquired cholesteatoma: our experience. Journal of otolaryngology - head & neck surgery = Le Journal d’otorhino-laryngologie et de chirurgie cervico-faciale, 37, 481-487.
- Marchioni D, Alicandri-Ciufelli M, Molteni G, Genovese E, Presutti L (2010) Endoscopic tympanoplasty in patients with attic retraction pockets. The Laryngoscope, 120, 1847-1855.
- Presutti L, Gioacchini F M, Alicandri-Ciufelli M, Villari D, Marchioni D (2014) Results of endoscopic middle ear surgery for cholesteatoma treatment: a systematic review. Acta otorhinolaryngologica Italica : organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale, 34, 153-157.
- Tarabichi M, Arsiwala Z (2021) History of Endoscopic Ear Surgery. Otolaryngologic clinics of North America, 54, 1-9.
- Cohen M S, Basonbul R A, Barber S R, Kozin E D, Rivas A C et al (2018). Development and validation of an endoscopic ear surgery classification system.The Laryngoscope, 128,967-970.
- Nomura Y (1982) Effective photography in otolaryngology-head and neck surgery: endoscopic photography of the middle ear. Otolaryngology--head and neck surgery :official journal of American Academy of Otolaryngology-Head and Neck Surgery, 90, 395-398.
- Badr-el-Dine M. (2002) Value of ear endoscopy in cholesteatoma surgery. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology, 23, 631-635.
- El-Guindy A (1992) Endoscopic transcanal myringoplasty. The Journal of laryngology and otology, 106, 493-495.
- Anzola J F, & Nogueira J F (2016) Endoscopic Techniques in Tympanoplasty. Otolaryngologic clinics of North America, 49, 12531264.
- Moneir W, Abd El-Fattah AM, Mahmoud E, Elshaer M (2017) Endoscopic stapedotomy: Merits and demerits. J Otol. :97-100.
- Das A, Mitra S, Ghosh D, Sengupta A (2021) Endoscopic Stapedotomy: Overcoming Limitations of Operating Microscope. Ear, nose, & throat journal, 100, 103-109.
- Emre I E, Cingi C, Bayar Muluk N, Nogueira J F (2020) Endoscopic ear surgery. Journal of otology, 15, 27-32.
- Briner H R, Simmen D, Jones N (2005) Endoscopic sinus surgery: advantages of the bimanual technique. American journal of rhinology, 19, 269-273.
- Hintschich C A, Fischer R, Seebauer C, Schebesch K M, Bohr C, et al(2022). A third hand to the surgeon: the use of an endoscope holding arm in endonasal sinus surgery and well beyond. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery, 279, 1891-1898.
- Badr-El-Dine M, James A L, Panetti G, Marchioni D, Presutti L, et al (2013) Instrumentation and technologies in endoscopic ear surgery. Otolaryngologic clinics of North America, 46,211-225.
- Escudero L H, Castro A O, Drumond M, Porto S P, Bozinis D G, et al (1979) Argon laser in human tympanoplasty. Archives of otolaryngology ,105, 252-253.
- Perkins R C (1980) Laser stepedotomy for otosclerosis. The Laryngoscope, 90, 228-240.
- Vincent R, Gratacap B, Causse J B, Gherini S (1996) Argon laser and Gherini-Causse Endo-Otoprobe in otologic surgery. Ear, nose, & throat journal, 75, 770-780.
- Saeed S R, Jackler R K(1996) Lasers in surgery for chronic ear disease. Otolaryngologic clinics of North America, 29, 245-256.
- Fyrmpas G, Tsetsosm N, Katotomichelakis M, Rudic M (2021) Lasers in endoscopic middle ear surgery: where do we stand today? European Archives of Oto-Rhino-Laryngology : Official Journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : Affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery, 278, 4169-4177.
- Clark M P, Commins D (2006) One-handed KTP laser application with suction, for ear surgery. Annals of the Royal College of Surgeons of England, 88, 500.
- Chang WT, Tong MCF (2020) Adopting Chopsticks Technique in Endoscopic Ear Surgery - An Alternative to Single-handed Operations. J Otolaryng Head Neck Surg 6: 46.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.