Adult Patient with Complete Androgen Insensitivity Syndrome (CAIS)-Late Diagnosis and Serious Psychological Sequelae - Case Report
by Szymacha Weronika1*, Maraszewska Ewa1, Karolina Kowalczyk2, Aleksandra Buczek-Kutermak3, Dagmara Pluta2
1Student Scientific Society at the Department of Gynecological Endocrinology, School of Medicine, Medical University of Silesia, Medyków 14, 40-752 Katowice, Poland.
2Department of Gynecological Endocrinology, Faculty of Medical Sciences in Katowice, Medical University of Silesia, Medyków 14, 40-752 Katowice, Poland.
3Omnia Medica, Al. Piłsudskiego 67b, 43-100 Tychy, Poland
*Corresponding Author:- Weronika Szymacha, Student Scientific Society at the Department of Gynecological:- Endocrinology, School of Medicine, Medical University of Silesia, Medyków 14, 40-752 Katowice, Poland. 885396619.
Received Date: 18 September 2024
Accepted Date: 1 October 2024
Published Date: 4 October 2024
Citation: Weronika S, Ewa M, Kowalczyk K, Buczek-Kutermak A, Pluta D (2024) Adult Patient with Complete Androgen Insensitivity Syndrome (CAIS)-Late Diagnosis and Serious Psychological Sequelae - Case Report Gynecol Obstet Open Acc 8: 214. https://doi.org/10.29011/2577-2236.100214
Abstract
The following case report aims to highlight the psychological aspect in patients with complete androgen insensitivity. Androgen insensitivity syndrome (AIS) is a rare cause of primary amenorrhoea. Treatment depends on the patient's phenotype and gender, involving removal of the testes after or before puberty. Contemporaries often leave the testes until late puberty to allow testosterone to promote the development of secondary sexual characteristics. However, leaving the gonads carries a risk of malignancy, so annual follow-up is necessary. Additional procedures include dilatation of the vaginal diverticulum or surgical vaginal creation, which may not be required in some patients. The decision to have surgical correction of the external genitalia should be an informed one and preferably made after reaching adulthood. Psychological care is crucial as women with complete androgen insensitivity syndrome (CAIS) have an increased risk of psychological, mood, and anxiety disorders. It is important that patients receive support from the time of diagnosis to help them cope with the challenges of gender identity and social roles. The clinical case highlights the need for education about gender development and early diagnosis of CAIS, which is important for cancer risk reduction and psychological support. A multidisciplinary approach, involving gynecologists, endocrinologists, geneticists and specialists in psychiatry and psychology, is crucial in the treatment of AIS. Further research and awareness-raising among doctors and parents is needed.
Keywords:androgen insensitivity, CAIS, gender development disorders, psychological aspect of diagnosis
Introduction
Androgen Insensitivity Syndrome (AIS-Androgen Insensitivity Syndrome) is one of the causes of disorders of sexual development. The onset of AIS is associated with the occurrence of mutations in the gene encoding the androgen receptor, leading to a loss of function of this receptor. The syndrome is most often inherited in a recessive manner, coupled to the X chromosome, but 30% of detected mutations are de novo [1]. Despite the male karyotype (46, XY), the external genital organs of patients with AIS show varying degrees of abnormalities, from the presence of an almost normal male phenotype to a completely female phenotype, which depends on the degree of androgen resistance. Depending on the clinical manifestation, there are 3 forms of AIS: partial (PAIS), mild (MAIS), and complete (CAIS) form. The complete androgen insensitivity syndrome presences of both female external genitalia and testes, usually located in the pelvis or inguinal canals, with an XY karyotype and predominantly female gender identification. During the fetal period, the lack of androgen receptor activity prevents the action of testosterone and dihydrotestosterone [2]. As a result, the development of structures derived from Wolffian ducts does not occur, resulting in the lack of formation of internal male sex organs, such as the epididymis, ductus deferens, seminal vesicles and prostate gland. At the same time, the Anti-Müllerian hormone (AMH) produced in the Sertoli cells of the testes causes regression of the Müllerian ducts, which prevents the development of female internal sex organs. During sexual maturation, testosterone secreted by the testes is converted to estradiol in the peripheral tissues, leading to the development of some secondary female sexual characteristics, such as the development of breasts and a female body figure, with no or scanty sexual hair and a blind vagina. Sexual hairiness is sparse or absent as it depends on the action of androgens and in CAIS there is complete insensitivity to androgens. In contrast, a blind vagina is due to the inhibitory effect of AMH on the proximal part of the vagina; the posterior part of the vagina is independent of the action of the hormone [3][14]. Complete androgen insensitivity syndrome occurs with a frequency of 2-5:100000 people with a male karyotype. The diagnosis of AIS usually occurs as a result of the discovery of an inguinal hernia in children (resulting from the presence of undescended testicles) or primary amenorrhea [3, 10]. The case described in this work involves a patient diagnosed with CAIS only at the age of 40.
Case presentation
A 40-year-old female patient was admitted to the Department of Gynecological Endocrinology at the Silesian Medical University in Katowice with a pre-determined karyotype of 46XY and an ultrasound result that showed an absent uterus and no visible gonads, in order to expand the diagnosis. During hospitalization, a gynecological examination was performed, which showed a properly developed vulva, clitoris, urethral meatus and the vaginal entrance was determined to be moderately wide. A blindly terminated vagina was visualized, and the uterine adnexa were determined to be non-explosive. The patient's axillary hair was never present, and pubic hair was sparse, of the female type. Symmetrical, normal breasts of glandular structure without focal changes on palpation were found. Sexual development was graded M5 on the Tanner scale. Normal folitropin (FSH) and progesterone results were obtained. Elevated values of lutropin (LH) and androstenedione were found in the hormonal tests. Attention was drawn to significantly elevated levels of total and free testosterone and AMH. (Table 1) An ultrasound was ordered, which confirmed the absence of a uterus. A structure possibly corresponding to a gonad was visualized in the right ovarian cast, and no gonad was visualized in the left ovarian cast. Accordingly, the diagnosis was expanded to include a pelvic magnetic resonance imaging (MRI), which described the absence of the uterus and adnexa, as well as a nodule of the left adrenal gland. In view of the exhaustion of further non-invasive diagnostic methods, surgical exploration of the gonads was ordered. During the observation of the patient in the ward, a significantly lowered mood was noticeable. The patient agreed to a psychological consultation, which revealed that the patient was further characterized by a tendency to withdraw, lack of assertiveness, lack of a sense of identity, anhedonia and derealization. Psychoeducation was carried out, and it was recommended that she continue after her hospitalization. The patient underwent a diagnostic laparoscopy procedure without complications. The histopathological examination obtained after the procedure described the right gonad (4.5x2x2cm) as a macroscopically unchanged testis. The histopathological diagnosis described an immature testis, seminal tubular epithelium composed of immature Sertoli cells and proliferation of Leydig cells in the lining. In the left gonad (3.5x2x2cm), the image of an immature testicular utricle and crushed ducts of epididymal epithelium were also described. (Figure 1). After the procedure, the patient received hormone replacement therapy administered by the transdermal route and ongoing psychological support, as well as a recommendation for further follow-up at the Gynecological Endocrinology Clinic.
|
Hormone |
Patient score |
Standard |
|
FSH |
8,85 |
1,7-21,5 IU/l |
|
LH |
22,1 |
1-95 IU/l |
|
Progesterone |
1,47 |
0,27-2,54 ng/ml |
|
Androstendione |
2,14 |
0,49-1,31 ng/ml |
|
Total testosterone |
>15 |
0,084-0,481 ng/ml |
|
Free testosterone |
14,79 |
0,2-4,1 pg/ml |
|
AMH |
159 |
0,06-4,4 ng/ml |
Table 1: Hormone test results
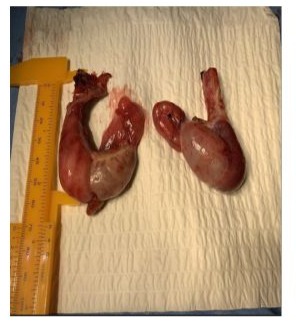
Figure 1: Right and left gonad. The photograph was taken immediately after removal, still in the operating theatre, before securing the material for histopathological examination.
Discussion
Androgen insensitivity syndrome is one of the rare causes of primary amenorrhea. Treatment depends on the phenotype and gender of the individual. Encountered methods of treating complete androgen insensitivity are: removal of the testicles after puberty, as in the presented case, or total gonadectomy before the onset of sexual maturation [2]. Currently, many clinical centers opt to leave the testicles in place at least until late puberty, when high testosterone levels allow for spontaneous puberty. However, the timing of the procedure is currently a topic of debate, as the testes are a source of testosterone, which undergoes peripheral conversion to estrogen, which allows the development of secondary sexual characteristics; on the other hand, it is reported that leaving the gonads is associated with a risk of carcinogenesis [4],[8]. Bilateral gonadectomy used to be the standard and was performed as soon as the diagnosis was confirmed, but since 1995, when the disease was first described, numerous studies have found a risk of carcinogenesis that varies from 22% to as low as 0.8%, according to various sources [7]. Removal of the gonads is associated with the use of hormone replacement therapy until the age of 50 [9]. Young women may be concerned about taking medications for most of their lives. They are uncertain about the side effects of therapy [7] and have concerns about the gonadectomy procedure itself and its risks, so sometimes they decide to postpone the surgery, or forgo it altogether. If gonadectomy is abandoned, annual monitoring of the gonads left behind, including determination of tumor markers and abdominal ultrasound, is necessary [11] . Another consideration remains dilatation of the vaginal diverticulum or complete surgical creation of the vagina [12]. Neovagina creation is carried out in the manner of minimally invasive dilatation or surgery using the Abbe-McIndoe method and the Vecchietti and Davydov-Moore procedure, which involves the creation of a vagina from the peritoneal bulb. The aforementioned methods have their advantages and disadvantages - even non-invasive dilatation is associated with discomfort and time-consuming[6]. However, it should be noted that not all patients will require this type of surgery, [5][13] as was the case with the presented patient. The existing vaginal recess may be sufficiently stretchy or even the size of a normal vagina. In order for the patient to make an informed decision regarding surgical correction of the external genitalia, it is recommended that this stage of treatment be carried out even after the patient has reached the age of majority. It is impossible to ignore such an important but sensitive issue as psychological or psychiatric care for a patient with androgen insensitivity syndrome. The presented patient received help in this area already during her hospitalization and continued for many weeks after the procedure. According to research, women with CAIS have a 5-fold higher risk of psychiatric disorders, a 3-fold higher risk of mood disorders, a 4-fold higher risk of anxiety disorders and a 20-fold higher risk of obsessive-compulsive disorders. Moreover, knowing that sexual well-being depends on both physical and psychological states, it is concluded that CAIS patients face far-reaching lack of self-confidence and lack of sexual satisfaction, or even before that, anxiety at the very thought of engaging in intercourse.[4]These data confirm the need for a psychiatrist or psychologist to care for the patient, especially when the diagnosis significantly affects a previously certain gender identity and social role. Moreover, doctors should be open to the patient's decision to change her gender identity to male, or other than female and male.
Conclusions
The presented clinical case highlights one of the reasons for the lack of early diagnosis of CAIS - the lack of education of the youngest children and parents about sexual development. If there had been awareness in the patient's community about the need to see a doctor if menarche did not occur, the patient would have been diagnosed while she was still in her teens. Prompt diagnosis of CAIS is crucial because of the reduction of the risk of tumors of embryonic origin in the undescended testicles and for psychological reasons, given the fact of the patients' predominantly female gender identity, which will confront the diagnosis of male chromosomal sex. The case underscores the importance of a multidisciplinary approach that involves gynecologists, endocrinologists, geneticists and specialists in psychiatry and psychology in the care of patients with CAIS. Further research and awareness-raising for doctors as well as parents is needed to improve understanding and treatment of this complex disease.
Declarations
Contributors:
All authors contributed to planning, literature review and conduct of the review article. All authors have reviewed and agreed on the final manuscript.
Competing interests: None
Patient consent for publication:
Informed consent was obtained from the patient, consent form available upon request / Not applicable
Ethics approval and consent to participate:
Ethical approval for this publication by IRB at Kern Medical / Not applicable
Availability of data and materials: Not applicable
Funding: None from any funding agency in the public, commercial or not-for-profit sectors. / Not applicable
References
- Tyutyusheva N, Mancini I, Baroncelli GI, D'Elios S, Peroni D. et al (2021) Complete Androgen Insensitivity Syndrome: From Bench to Bed. Int J Mol Sci 22 (3): 1264.
- Delli Paoli E, Di Chiano S, Paoli, D (2023) Androgen insensitivity syndrome: a review. J Endocrinol Invest 46, 2237–2245.
- Fulare S, Deshmukh S, Gupta J (2020) Androgen Insensitivity Syndrome: A rare genetic disorder. Int J Surg Case Rep 71: 371-373.
- Kosti K, Athanasiadis L, Goulis DG (2019) Long-term consequences of androgen insensitivity syndrome. Maturitas 127: 54–1.
- Guo M, Huang JC, Li CF, Liu YY (2023) Complete androgen insensitivity syndrome: a case report and literature review. J Int Med Res 51 (2): 3000605231154413.
- KOT, Justyna and JACH, Robert 2019. Metoda Davydova-Moore’a w leczeniu zespołu Mayera-Rokitansky’ego-Kustera-Hausera. Studium przypadku. Pielęgniarstwo Polskie.
- Deans R, Creighton SM, Liao LM, Conway GS (2012) Timing of gonadectomy in adult women with complete androgen insensitivity syndrome (CAIS): Patient preferences and clinical evidence. Clin Endocrinol (Oxf).
- Gamcová Viktória, Eim Josef, Meixnerová Ivana, Hudeček Robert (2022) Complete androgen insensitivity syndrome - rare case of malignancy of dysgenetic gonads. Ceska Gynekol. 87 (3) :184-187.
- Singh P, Gothwal M, Yadav G, Singh K (2019) Complete Androgen Insensitivity Syndrome: Dilemmas for Further Management after Gonadectomy. J Hum Reprod Sci 12 (4) :348-350.
- Deeb A, Hughes IA (2005) Inguinal hernia in female infants: a cue to check the sex chromosomes? BJU Int 96 (3) :401-3.
- Döhnert U, Wünsch L, Hiort O (2017) Gonadectomy in Complete Androgen Insensitivity Syndrome: Why and When? Sex Dev 11 (4) :171-174.
- Ismail-Pratt IS, Bikoo M, Liao LM, Conway GS, Creighton SM (2007). Normalization of the vagina by dilator treatment alone in Complete Androgen Insensitivity Syndrome and Mayer-Rokitansky-Kuster-Hauser Syndrome. Hum Reprod 22 (7): 2020-4.
- Gomez-Lobo V, Amies Oelschlager AM (2016) North American Society for Pediatric and Adolescent Gynecology. Disorders of Sexual Development in Adult Women. Obstet Gynecol. 128 (5) :1162-1173.
- Lanciotti L, Cofini M, Leonardi A, Bertozzi M, Penta L, et al. (2019) Esposito, S. Different Clinical Presentations and Management in Complete Androgen Insensitivity Syndrome (CAIS). Int. J. Environ. Res. Public Health 16: 1268.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.