Acute Thalamic Stroke caused by Primary Angiitis of Central Nervous System: A Case Report and Literature Review
by Husam Jamil*, Zeinab Abdallah Ellias Diab, Gihan Musa, Mohammad Mohiuddin
Calderdale and Huddersfield Foundation Trust, UK
*Corresponding author: Husam Jamil, ST7 Acute Internal Medicine and Stroke Fellow at Yorkshire and Humber deanery Calderdale and Huddersfield Foundation Trust, Uk.
Received Date: 24 July, 2025
Accepted Date: 06 August 2025
Published Date: 08 August 2025
Citation: Jamil H, Diab ZAE, Musa G, Mohiuddin M (2025) Acute Thalamic stroke caused by primary angiitis of central nervous system. J Neurol Exp Neural Sci 7: 159. https://doi.org/10.29011/2577-1442.100059.
Abstract
Primary angiitis of central nervous system (PACNS) is a rare and poorly understood disorder. Stroke as its complication is a recognised entity. We present a case of a 67-year-old female who had presented with sudden onset confusion and slurring of speech on the background of PACNS. CT head and MRI scans confirmed a left sided thalamic stroke. She was managed by a multi-disciplinary team of stroke physicians, rheumatologists, radiologists, physiotherapists, occupational therapists and speech and language therapists. She was discharged after 3 days of admission in stroke unit and remained well upon three-month followup review. Our case adds insights to this rare presentation and to the body of knowledge of this clinical area.
Introduction
PACNS is rare [1]. and is generally associated with poor clinical outcomes. It has a wide clinical spectrum, and it poses a clinical challenge for diagnosis and management. Prior studies categorised different subtypes of primary angiitis of the central nervous system (PACNS) based on distinct clinical, radiological, and histopathological features , and have been linked to the disease severity, morbidity and mortality.
In this case we discuss a patient who developed stroke on the background of PACNS and had favourable clinical outcomes following prompt management.
Case Presentation
A 67-year-old female patient presented to the emergency department of a district general hospital in UK with clinical symptoms of confusion and slurring of speech from a day ago. She had a past medical history of interstitial lung disease for which she was on 2mg prednisolone once a day, mild cognitive impairment, hypertension and probable primary angiitis of the CNS (PACNS) based on abnormal MRI, atypical perinuclear antineutrophil cytoplasmic antibodies (pANCA) and positive being lupus anti-coagulant. The diagnosis of probable PACNS was made 7 years ago by Rheumatology team and she had received pulsed Cyclophosphamide Methylprednisolone with good clinical improvement, following which these medications were discontinued. Upon this admission, she was only on Mycophenolate Mofetil 500mg once daily for PACNS.
The history was obtained from a family member who accompanied her and described her as ‘not her usual self as she kept on forgetting things’. This was an acute and sudden onset deterioration on the background of her cognitive impairment. The slurring of speech was also of sudden onset. There were no features of facial droop, limb weakness, vision symptoms and collapse with head injury.
An urgent CT head (Figure 1) was arranged which confirmed acute/ subacute infarct in left thalamus following which an urgent referral to the stroke team was made. Upon assessment by the stroke team, patient had a BP of 132/91, National Institute of Health Stroke Scale (NIHSS) score of 6/42 and modified Rankin Scale (mRS) of 1/6. Clinical examination revealed confusion and word finding difficulty which led to the NIHSS score of 6. A decision was made to admit the patient to hyper-acute stroke unit (HASU) locally
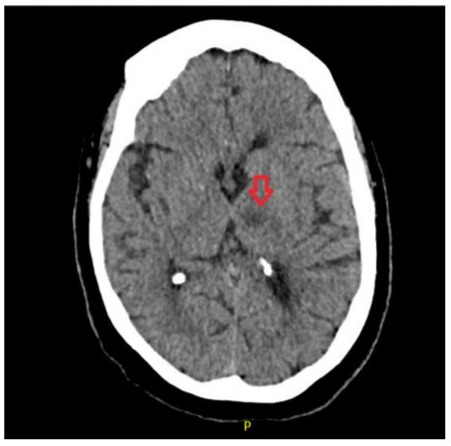
Figure 1: CT head demonstrating focal hypodensity in the left thalamus (red arrow) with appearances concerning for acute/ subacute infarct possibly on a background of small chronic infarct.
Patient was treated with standard stroke care which included anti-platelet therapy, statins and multi-disciplinary (MDT) approach. The MDT included stroke physicians, rheumatologists, radiologists, speech and language therapists, physiotherapists and occupational therapists. An MRI scan with DWI FLAIR imaging of the brain was arranged (figure 2) to determine the age of the infarct, the MRI confirmed an acute stroke in the left thalamus. A 24-hour tape was arranged to observe electrical activity of the heart which did not reveal any arrythmias. Carotid ultrasound was normal. A referral was also made to Rheumatology team to advise further on PACNS management. They did not advise any further change in medication. The view of MDT was that this stroke was a likely complication of PACNS.
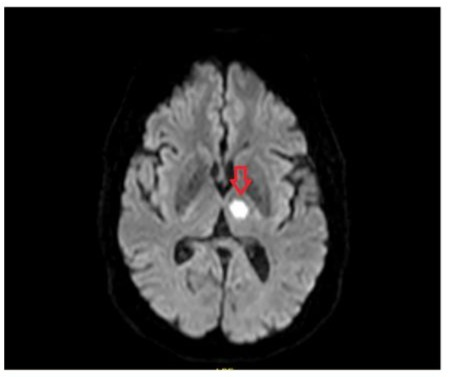
Figure 2: Well-defined focal area (red arrow) of FLAIR hyperintensity involving the left thalamic region signifying an acute infarct on the MRI DWI FLAIR scan.
After 3 days of inpatient stay, patient improved remarkably well and was discharged on life-long clopidogrel. An outpatient MR angiogram scan 2 months after discharge showed improvement in the infarct area with no new abnormalities. Her 90-day mRS on follow up by stroke team was 1/6 following which she was discharged from stroke care. Consent was obtained from patient for documentation of this case report.
Discussion
Search Strategy
For the literature review, an advanced search was performed on PubMed from 1998 to 2025. Key words were formed for the two important concepts relevant for the case report: ischemic thalamic stroke and PACNS. The keywords within each concept were combined with an OR and between the two concepts were joined by an AND. Figure 3 describes our search strategy in more detail. Google scholar was used as well for the literature review. Relevant studies are mentioned in sections below.
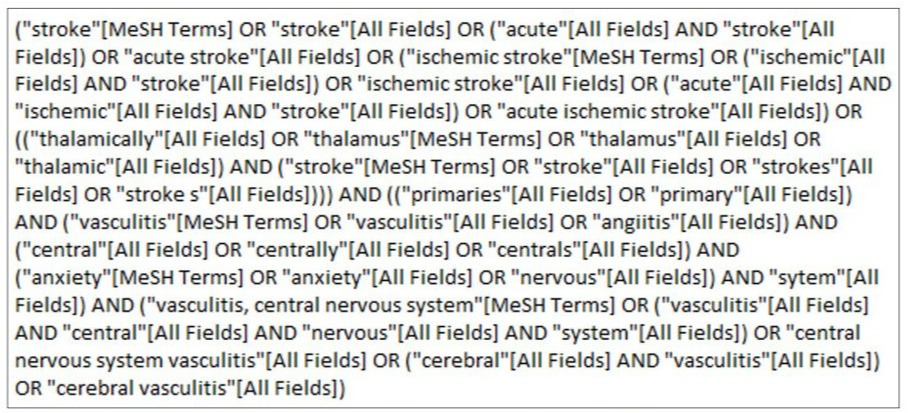
Figure 3: Search strategy on PubMed for literature review for our case report. Keywords included acute stroke, acute ischemic stroke, thalamic stroke, primary angiitis of central nervous system and cerebral vasculitis.
PACNS Epidemiology
Epidemiology
PACNS is extremely rare and can present with a wide spectrum of neurological symptoms, often mimicking other unusual or unexplained neurological conditions. With a documented incidence [1] of 2.4 per 1,000,000 person-years, PACNS is perceived as not a single disease entity but rather an umbrella term encompassing several subtypes, which may involve different regions of the CNS, affect vessels of varying sizes, and display distinct histological and pathological patterns. Although brain biopsy is regarded as the gold standard diagnostic test, its sensitivity and specificity are limited. Therefore, careful assessment to rule out PACNS mimics is crucial [2]. Our patient did not undergo brain biopsy, and diagnosis was made based on MRI findings, atypical pANCA and positive being lupus anti-coagulant-hence the term ‘probable PACNS’.
Clinical Presentation and Incidence of stroke as a complication
The most common presenting symptoms [3] included focal neurological deficits (63%), headaches (51%), and cognitive decline (41%).Patients with biopsy-proven disease had higher rates of cognitive impairment (55% vs 39%) and seizures (36% vs 16%) compared to those with angiography-confirmed disease, whereas focal neurological signs were less common (56% vs 95%). Cerebrospinal fluid abnormalities were observed in 97% vs 65%, and MRI abnormalities in 97% vs 98% of cases, respectively [3] in a systematic review. Its broad clinical presentation can also include ischaemic or, infrequently, haemorrhagic strokes as found in the retrospective analysis of Patel [4] et al, which studied 1136 patients admitted to US hospitals from 2016-2018. The analysis revealed that out of those admitted, ischemic stroke was found in 38.2%, haemorrhagic stroke in 13% and transient ischemic attack in 20.2% of patients. This supports the view of our MDT that the thalamic stroke in our patient was a complication of probable PACNS.
Thalamic Stroke
The thalamus has important functions which include sleep cycle, emotions, memory, executive functions, processing of sensory infection and sensorimotor control. A stroke [5] in this region can impair memory and learning, impairments of orientation, personality and executive function and language deficits. Our patient presented with acute memory loss and word finding difficulty and this can be explained based on location of stroke.
Treatment in PACNS and acute ischemic stroke
The Recommendations for management of PACNS have been made mainly based on observational studies and there is need for higher evidence based Randomized controlled trials [6]. The approach to management of Primary angiitis of CNS is based on two phases. Initially phase is the induction of Remission, which is subsequently followed by the phase of maintenance [7]. The remission of disease activity was defined as improvement in disease symptoms without developing any new symptoms after a period of 3 months following the initiation of induction phase, in a French observational study [8].
Induction of Remission
A combination of corticosteroids alongside cyclophosphamide is mainly used for induction of Remission[6]. A relapse was defined development of either a new symptom or clinical worsening from baseline or development of new changes on subsequent imaging [8]. Prednisone orally at starting oral dose of 1mg/kg, and most people achieved Remission after they received the treatment for a span of 12-18 months [9].
Maintenance Therapy
This achieved primarily by using immunosuppressive medications such as Methotrexate, Azathioprine, Mycophenolate. In most Reports, Immunosuppressants are combined with oral steroids which are slowly tapered own are used in the maintenance phase [3]. Our patient had initially received induction therapy which yielded good results and later she was on maintenance therapy with Mycophenolate Mofetil.
The UK stroke guidelines in 2023 [10] have clearly described the management of acute ischemic stroke in view of updated guidance on extended-windows for thrombolysis, thrombectomy, wake-up strokes and secondary prevention. As the patient has presented a little above 24 hours of symptom onset, they did not qualify for thrombolysis or thrombectomy hence were treated with standard acute ischemic stroke care. This did not influence their medication management of PACNS and other co-morbidities.
Prognosis of PACNS
Overall, long-term survival is reduced in primary CNS vasculitis [1]. A retrospective study revealed that increased mortality was linked to large vessel involvement in cerebral infarction, older age at diagnosis, and diagnosis by angiography [11]. Our patient did well following the MDT management and 3 month followup revealed similar mRS as was pre-admission. As per the most recent input of rheumatology, there are plans to further reduce the dose of Mycophenolate Mofetil in upcoming reviews.
Strengths of our study
Our literature search did not reveal a specific case of thalamic stroke caused by PACNS. Our study shows that with MDT approach, prompt treatment and diagnosis can lead to favourable outcomes in this group of patients.
Limitations of our Study
This is a case-study. The literature has scant information on the topic of PACNS and stroke as its complication. Randomised trials are needed for stronger evidence on this niche clinical area.
Conclusion
Our study adds to the body of knowledge of management of PACNS patients who present with acute stroke. MDT approach is optimal way of management for better prognosis. More studies are needed in future to enhance the knowledge base of stroke due to PACNS.
References
- Salvarani C, Brown RD, Calamia KT, Christianson TJ, Weigand SD, et al. (2007) Primary central nervous system vasculitis: analysis of 101 patients. Annals of Neurology 62(5): 442-451.
- Mandal J, Chung SA (2017) Primary angiitis of the central nervous system. Rheumatic Disease Clinics 43(4): 503-518. 3. Beuker C, Strunk D, Rawal R, Schmidt-Pogoda A, Werring N, et al. (2021) Primary Angiitis of the CNS: A Systematic Review and Metaanalysis. Neurol Neuroimmunol Neuroinflamm 8(6): e1093. 4. Patel SD, Oliver FO, Elmashad A, Patel N, Mehta T, et al. (2022) Outcomes among patients with primary angiitis of the CNS: A Nationwide United States analysis. Journal of Stroke and Cerebrovascular Diseases 31(11).
- Schmahmann JD (2003) Vascular syndromes of the thalamus. Stroke 34(9): 2264-2278.
- Beuker C, Schmidt A, Strunk D, Sporns PB, Wiendl H, et al. (2018) Primary angiitis of the central nervous system: diagnosis and treatment. Therapeutic advances in neurological disorders 11. 7. Sherri A, Mortada MM, Makowska J, Polak A (2024) Primary angiitis of the CNS and ANCA-associated vasculitis: from pathology to treatment. Rheumatology International 44(2): 211-222.
- Kesav P, Raj DM, Ali RA, Hussain SI, John S (2024) Primary CNS Vasculitis-a Focussed review on treatment. Vascular Health and Risk Management 20: 453-465.
- Godasi R, Pang G, Chauhan S, Bollu PC (2018) Primary central nervous system vasculitis. Treasure Island, StatPearls Publishing, USA.
- Crow J, Smith A (2023) National Clinical Guideline for stroke for the United Kingdom and Ireland: part I–an overview of the updated recommendations. British Journal of Occupational Therapy 86(10): 661-664
- Salvarani C, Brown RD, Christianson TJH, Huston J, Giannini C, et al. (2015) Adult Primary Central Nervous System Vasculitis Treatment and Course: Analysis of One Hundred Sixty-Three Patients. Arthritis & Rheumatology 67(6): 1637-1645.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.