Acute Richter’s Incisional Hernia Trough Trocar Site after Laparoscopic Gastric Surgery: A Futile Complication or with a Fatal Risk?
by Italo Braghetto*, Owen Korn, Bárbara Carreño, Enrique Cruz, Valentina Núñez
Department of Surgery, Hospital Clínico “Dr. José J. Aguirre” Faculty of Medicine, University of Chile, Santiago,Region Metropolitana, Chile
*Corresponding Author: Italo Braghetto, Department of Surgery, Hospital Clínico “Dr. José J. Aguirre” Faculty of Medicine, University of Chile, Santiago, Region Metropolitana, Chile
Received Date: 09 January 2026
Accepted Date: 14 January 2026
Published Date: 16 January 2026
Citation: Braghetto I, Korn O, Carreño B, Cruz E, Núñez V (2026) Acute Richter’s Incisional Hernia Trough Trocar Site After Laparoscopic Gastric Surgery: a Futile Complication or With a Fatal Risk? J Surg 11: 11540 https://doi.org/10.29011/2575-9760.011540
Abstract
Trocar Site Hernia (TSH) is an important yet under-recognized complication, reported in 0.3% to 6% of laparoscopic surgery, depending on patients characteristics (age, BMI), trocar type and diameter.The objective of this paper is to report the incidence and clinical presentation of acute Richter´s TSH after laparoscopic gastric resection analyzing the diagnosis, surgical procedures, postoperative complications and outcome. This study is based on the experience on 1612 patients submitted to laparoscopic gastric surgery performed by a single surgeon (IB) for different causes. For these procedures 5 trocars were used. Four out of 1612 patients were re-operated due to acute small bowel obstruction (0.24%) confirmed with CTscan and submitted to laparoscopic exploration,soon after diagnosis confirmation that are the subject of analysis. TSH occurred at 12-mm ports, all patients were submitted to re-operation for treatment of complications secondary to small bowell obstruction, two had severe septic complications due aspirative pneumonia anddisruption of previous gastrojejunl anastamosis. All patients were submitted to re-operation for early recognition and surgical management. Despite the severe complications patient outcomes was favorable without postoperative mortality. The hospital stay ranged from 10 to 82 days. TSH is an uncommon event but carries substantial morbidity and potentially fatal consequences, should be recognized as a serious postoperative threat rather than a benign technical inconvenience. Early diagnosis, routine fascial closure of large ports, and heightened vigilance in postoperative gastric surgery patients could improve outcomes.
Keywords: Complications; Hernia; Laparoscopy; Site; Trocar
Introduction
Laparoscopic surgery is widely practiced and offers realistic benefits over conventional surgery. Port site hernia is an important yet under-recognized complication of laparoscopic surgery, which carries a high risk of strangulation due to the small size of the defect involved. There is considerable variation in results between surgeons, concerning port-site complications. Trocar Site Hernias (TSH) are reported in 0.3% to 6% of laparoscopic cases, depending on patients characteristics (age, BMI), trocar diameter and type. Most occur with trocars over 10 mm in diameter [1-5].
The Objective Of This Paper Is:
- To calculate the incidence and clinical presentation of acute Richter´s incisional hernia after laparoscopic gastric resection
- To analyze the performed surgical procedure after diagnosis confirmation, postoperative complications and outcome.
Material and Methods
This study is based on the experience with laparoscopic procedures with resectional gastric surgery performed by a single surgeon for different indications including a total universe of 1612 patients, divided as: Sleeve gastrectomy (683 patients), Resectional Gastric bypass, (551 patients), Fundoplication + distal gastrectomy for Barrett´s esophagus, (151 patients), Conversion to Toupet´s fundoplication+distal gastrectomy due to failed Nissen fundoplication, (81 patients), Conversion to resectional GBP after failed Sleeve gastrectomy due to reflux esophagitis, (66 patients) and Total gastrectomy for gastric cancer, (80 patients). The procedures were performed according to the indications and protocols established in our Departmentand published previously [6-11]. The trocars used (Single Use sterile laparocopic System Class IIa, Surgaid Medical, Xiamen, Co China) were inserted as follow: trocar 1, supra-umbilical (11mm); trocar 2, sub-xiphoid (5mm); Trocar 3(12mm), left subcostal axillary line(11mm); Trocar 4, mid-clavicular left upper abdominal quadrant (12mm between trocars 1 and 3);and trocar 5, mid-clavicular right upper quadrant of the abdomen (11mm) (Figures 1-3).
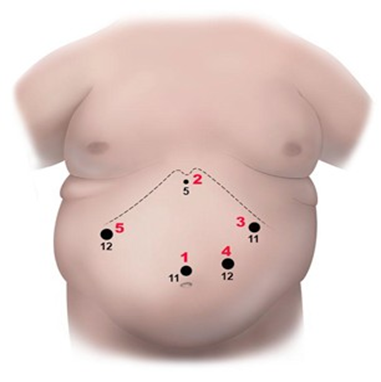
Figure 1: Trocar site location and diameter of each one (mm) for laparoscopic gastric resection.
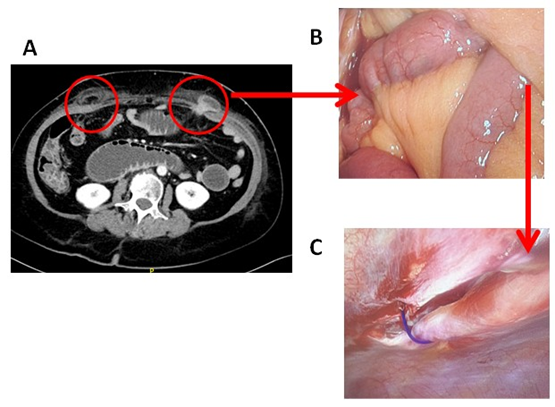
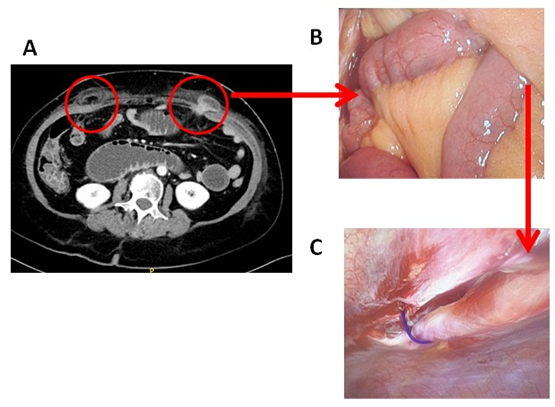
Figure 2: CT scan demonstrating two trocar site hernias demonstrating: A) right upper abdominal quadrant, and left upper abdominal quadrant with Richter´s small bowel hernia B) Intraoperative finding demonstrating small bowel obstruction and C) Closure of the trocar site hernia.
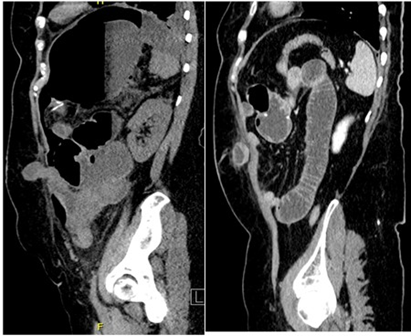
Figure 3: CT scan lateral vision demonstrating trocar site hernia at left upper abdominal quadrantdemonstrating small bowel obstruction.
Results
Four out of 1612 patients have been re-operated due to acute small bowel obstruction (0.24%, one of the lowest rate published) confirmed with CT scan and submitted to laparoscopic exploration soon after diagnosis confirmation that are the subjects of analysis. Table 1 presents the demographic characteristics of four female patients who developed acute Richter’s trocar-site hernia. In this cohort, all cases were female and half presented obesity, aligning with reports showing higher incidence in women and individuals with BMI >30. Patient profile correlates with known epidemiologic risk factors, suggesting that preoperative identification of high-risk individuals may guide preventive closure strategies.
Table 1. Patient Demographics characteristic of patients included
|
Case |
Age |
Sex |
BMI |
Diagnosis |
Operation |
|
Case 1 (CA) |
47 |
Female |
27.9 |
LSBE Esophagitis D |
Nissen Fundoplication + Antrectomy |
|
Case 2 (XC) |
61 |
Female |
25.3 |
Esophagitis grade D + Type III Hiatal Hernia |
Hiatoplasty + Nissen fundoplication |
|
Case 3 (JG) |
45 |
Female |
38.8 |
Morbid obesity + Esophagitis |
Sleeve Gastrectomy |
|
Sleeve gastrectomy |
|||||
|
Case 4 (MLG) |
60 |
Female |
30 |
HH + Esophagitis post SG |
LSBE : Long segment Barrett’s esophagus. SG: Sleeve gastrectomy. HH: Hiatal hernia.
All hernias occurred at 12-mm ports, consistent with evidence indicating port sizes ≥12 mm significantly increase hernia risk. Two patients presented trocar hernia after conversion or reoperation procedure that agree with supporting literature that secondary procedures and repeated manipulation may weaken fascial integrity. All patients were submitted to re-operation for treatment of the described complications as is shown in Table 2.
Table 2. Surgical Details and Trocar Characteristics: Relationship between surgical technique, trocar placement, and hernia development.
|
Case |
Initial Operation |
Second Operation |
Trocar Site Hernia |
Trocar Diameter |
Complication |
Re-operation |
|
Case 1 |
Nissen Fundoplication + Antrectomy |
No |
Right upper quadrant |
12mm |
Bowel obstruction |
Bowel reduction |
|
Case 2 |
Hiatoplasty + Nissen fundoplication |
Redo hiatoplasty +Toupet fundoplication+Distal Gastrectomy Roux –en- Y gastrojejunostomy |
Left upper quadrant |
12mm |
Bowel obstruction + Anterior partial dehiscence gastrojejunal anastomosis + Subhepatic perigastric abscess. |
Bowel reduction + Resuturing dehiscence+ Peritoneal lavage + Drainage + antibiotics. |
|
Case 3 |
Sleeve Gastrectomy |
Conversion to Roux-Y distal gastrectomy |
Left upper quadrant (Figure 2) |
12mm |
Bowel obstruction |
Bowel reduction |
|
Case 4 |
Sleeve Gastrectomy |
Conversion to Roux-Y distal gastrectomy |
Left paraumbilicalRight upper quadrant (Figure 3) |
12mm |
Bowel obstruction Omental hernia |
Bowel reduction Omental reduction |
Complications ranged from minor to life-threatening situations. Despite low overall incidence, severe complications such as septic shock and multi-organ failure were observed All patients were submitted to re-operation for treatment of the described complications. Patients recovered successfully after timely early recognition and surgical management had outcomes ultimately favorable, however others with severe complication should be considered a potentially lethal event requiring urgent evaluation and treatment. No mortality was observed despite presenting severe complications. (Table 3)
Table 3. Postoperative Complications and Outcomes
|
Case |
Surgical procedure |
Complication |
Management |
Hospital Stay (days) |
Clavien Dindo |
Outcome |
|
Case 1 |
Bowel reduction |
Localized bowel pneumatosis |
Conservative medical treatment |
10 |
IV |
Good |
|
Case 2 |
Bowel reduction. Resuturing dehiscence. Peritoneal lavage. Drainage + antibiotics. |
Wound infection |
Repeated wound lavage + antibiotics |
25 |
IV |
Good |
|
Case 3 |
Bowel reduction |
No major complication |
Uneventful recovery |
7 |
IV |
Good |
|
Case 4 |
Bowel reduction Omental reduction |
Severe septic shock, pneumonia, multiorgan distress |
ICU care, ventilation, antibiotics+ Antifungals+ amputations |
82 |
IV |
Good |
Discussion
Incidence and Timing Across Laparoscopic Procedures
TSH remains an infrequent but clinically significant complication of laparoscopic surgery can occur promoting serious risk of bowel obstruction eventually involving during the early postoperative period the anastomotics integrity. Reported incidences range widelyfrom 0.14% to 6%-depending on patient-related factors. Female sex and elevated BMI, age, co-morbidities, trocar diameter, surgical technique are risk factors for trocar-site hernias, especially in bariatric and foregut surgery. While many port-site hernias become apparent only months after surgery, acute Richter-type herniation represents a unique presentation characterized by early onset, minimal external findings, and a disproportionately high risk of strangulation due to entrapment of the anti-mesenteric bowel wall. This sharp contrast between low incidence and potentially catastrophic outcomes underscores the importance of early recognition [4,5,12-15]. Large series confirm that TSH may occur both early and late. Zareen et al [12]. reported an incidence of 0.14% during 43 months of follow-up with no associated mortality, whereas Pilone et al [13]. found a higher prevalence of 1.6% but also without acute complications. In contrast, studies focused on bariatric and complex upper gastrointestinal surgery report variable incidence ranging from 0.2 to 39.3% depending on the time of symptoms presentation, diagnosis methodology, risk factors and follow-up. By ultrasound or CT scan the incidence is so high as 39%. Clinically early hernias with relevant symptoms or its consequences receiving surgical treatment is 0.5 to 3% early hernias, likely reflecting larger trocar diameters (≥12 mm), prolonged manipulation, and elevated intra-abdominal pressure [5,14,16]. Our incidence of 0.0024% (4/1612) acute Richter’s hernias fits within the lower range of reported rates, yet the severity of presentations positions this as a complication underestimated in its clinical significance [13-17].
Risk Factors
As we mention before, risk factor analysis in the literature consistently highlights trocar diameter, obesity, female sex, and advanced age as major contributors to TSH development [1,2,13,17-19]. Most symptomatic TSHs occur at ≥10- 12 mm ports, a finding corroborated by our serie.
Additional procedural factors noted in bariatric and gastric surgery include:
- High intra-abdominal pressure due to pneumoperitoneum
- Repetitive torquing at working ports
- Prolongued manipulation
- Thick abdominal walls making fascial closure difficult [19-21]
Our cohort, composed exclusively of female patients with BMI ranging from normal to obese (25-38 kg/m²), aligns with established epidemiologic trends.
Acute vs Chronic Clinical Presentation
Chronic TSH tends to present with a palpable mass or discomfort, often diagnosed months to years after surgery. In contrast, acute TSH Richter’s hernia lacks classical obstructive symptoms because only part of the bowel circumference is incarcerated. Prior case reportsemphasize how subtle symptoms may progress abruptly to ischemia or perforation. All patients in our series presented with acute small-bowel obstruction, confirmed by CT scan, highlighting the typical but nonspecific early manifestations [21-24]. One unique case in our series showed two simultaneous Richter’s hernias in different trocar sites, reinforcing the need for meticulous evaluation in symptomatic postoperative patients.
Diagnostic Approach
CT scan remains the diagnostic modality of choice, with a high index of suspicion required in the early postoperative period. Ultrasound has been validated for late-detection screening in bariatric patients [25,26] but has limited sensitivity in acute settings. Rapid diagnosis is essential because Richter’s hernias may progress to necrosis without complete obstruction.
Complication Severity: Minor Event or Fatal Risk?
While many studies describe TSH as a minor complication, the literature clearly documents cases of strangulation, necrosis, perforation, peritonitis, and even mortality when diagnosis is delayed [22,23]. Our experience strongly reinforces this. Although all patients ultimately survived, one case evolved into bilateral pneumonia due to bile aspiration secondary to bowell obstruction, septic shock, multi-organ dysfunction, and distal limb necrosis, requiring prolonged ICU care and amputations due to . This case demonstrates that TSH, particularly of the Richter type, can trigger lifethreatening systemic complications. Thus, despite low incidence, the potential severity elevates trocar-site Richter’s hernia from a trivial technical complication to a genuinely fatal risk.
Prevention and Role of Fascial Closure
Routine fascial closure of 12-mm ports, particularly in upper abdominal locations, may reduce postoperative Richter-type hernia incidence but no consensus exists. The debate about routine closure of ≥10-12 mm trocar sites remains active. Survey data [1] confirm inconsistent practice patterns across specialties. Recent multicenter evidence [20] supports the use of 12-mm trocars with integrated fascial closure, demonstrating improved prevention rates in overweight patients. However, some bariatric surgery groups argue that non-closure may be acceptable due to postoperative weight loss decreasing wall tension [13].
Nonetheless, literature consensus indicates
- Closure of fascial defects ≥10 mm is recommended, particularly in the upper abdomen.
- Closure is crucial in obese patients due to thick adipose layers that mask early signs of herniation.
- Sharp or bladed trocars carry higher risk than conical dilating trocars [25-28].
In our series, all hernias occurred in 12-mm trocars, reinforcing the necessity for consistent and meticulous closure in high-risk cases.
Lessons Learned from our Experience
Several insights emerged from this analysis
- Early postoperative bowel obstruction after gastric surgery should raise immediate suspicion for Richter-type TSH, even in the absence of classic symptoms.
- CT confirmation is mandatory, as clinical evaluation alone may underestimate severity.
- Prompt laparoscopic reduction is safe, feasible, and avoids bowel loss in most cases.
- Severe systemic complications may occur, even in the absence of bowel necrosis, due to aspiration, delayed diagnosis, or physiologic stress from obstruction.
- Prevention through systematic closure of all ≥12 mm trocar sites should be strongly considered.
The strength of this study is because analyses the experience in a large number of patients, only one surgeon participating and only one single center. The limitation is because it includes only acute complication missing a follow-up for detection of undiagnosed presence of TSH
Conclusions
Richter’s trocar-site hernia is an uncommon event but carries substantial morbidity and potentially fatal consequences. Our series confirms that even in experienced hands and high-volume practice, acute TSH can develop and lead to severe complications. Given the low but real risk of strangulation, TSH should be recognized as a serious postoperative threat rather than a benign technical inconvenience. Early diagnosis, routine fascial closure of large ports, and heightened vigilance in postoperative gastric surgery patients are essential to improve outcomes.
References
- Owens M, Barry M, Janjua AZ, Winter DC (2011) A systematic review of laparoscopic port site hernias in gastrointestinal surgery. Surgeon. 4: 218-224.
- Comajuncosas J, Vallverdú H, Orbeal R, Parés D (2011) Trocar site incisional hernia in laparoscopic surgery. Cir Esp. 2: 72-76.
- Rossi A, McLaughlin D, Witte S, LynSue J, Haluck RS, et al (2017) An Expanded Retrospective Review ofTrocar site hernias in laparoscopic gastric bypass patients. J Laparoendosc Adv Surg Tech A. 6: 633-635.
- Karampinis I, Lion E, Grilli M, Hetjens S, Weiss C, et al (2019) Trocar site hernias in bariatric surgery—an underestimated issue. a Qualitative Systematic Review and Meta-Analysis Obes Surg. 29: 1049-1057.
- Coblijn UK, de Raaff CA, van Wagensveld BA, van Tets WF, de Castro SM (2016) Trocar port hernias after bariatric surgery. Obes Surg. 3: 546-551.
- Braghetto I et al. (All published works on sleeve gastrectomy, subtotal gastrectomy, fundoplication failures, and gastric cancer surgery included as methodological references in the manuscript).
- Braghetto I, Korn O, Valladares H, Gutiérrez L, Csendes A, et al (2007) Laparoscopic sleeve gastrectomy: surgical technique, indications and clinical results. Obes Surg. 17: 1442-1450.
- Braghetto I, Csendes A, Korn O, Gutierrez L, Brunet L, et al (2011) Laparoscopic resectional gastric bypass in patients with morbid obesity: experience on 112 consecutive patients. J Gastrointest Surg. 15: 71-80.
- Braghetto I, Korn O, Csendes A, Gutiérrez L, Valladares H, et al (2012) Laparoscopic treatment of obese patients with gastroesophageal reflux disease and Barrett’s esophagus: a prospective study..Obes Surg. 5: 764-772.
- Braghetto I, Martinez G, Korn O, Zamorano M, Lanzarini E, et al (2018) Laparoscopic subtotal gastrectomy in morbid obese patients: a valid option to laparoscopic gastric bypass in particular circumstances (prospective study). Surg Today. 48: 558-565.
- Braghetto I, Burgos A, Lasnibat, J.P (2024) Comparison of the Intragastric Volume and Pressure required to Cause a Leak Along the Suture Line in a Resected Stomach Post Sleeve Gastrectomy. Indian J Surg. 86: 571-575.
- Zareen M, Sarwar S, Ullah Z, Khattak A, Saeed R (2025) Surgeons’ preference regarding port site closure and incidence of port site hernias in bariatric surgery: a retrospective multicentre study. Cureus. 3: e80982.
- Pilone V, Di Micco R, Hasani A, Celentano G, Monda A, et al (2014) Trocar site hernia after bariatric surgery without fascial closure. Int J Surg. S1: S83-86.
- Karampinis I, Lion E, Hetjens S, Vassilev G, Galata C, et al (2020) Trocar Site HERnias After Bariatric Laparoscopic Surgery (HERBALS): a Prospective Cohort Study. Obes Surg. 5: 1820-1826.
- Scozzari G, Zanini M, Cravero F, Passera R, Rebecchi F, et al (2014) High incidence of trocar site hernia after laparoscopic or robotic Rouxen-Y gastric bypass. Surg Endosc. 10: 2890-2898.
- Abou Hussein B, Al Marzouqi O, Hajijama S, Al Ani A, Toba N, et al (2025) Effect of Fascial Closure versus Non-fascial Closure on Developing Trocar Site Hernias (TsH) in the Bariatric Population: A Systematic Review. Obes Surg. 5: 1925-1933.
- Ahlqvist S, Edling A, Alm M, Dackhammar JB, Nordin P, et al (2022) Trocar Site Hernia After Gastric Sleeve. Surg Endosc. 6: 4386-4391.
- Wells A, Germanos GJ, Salemi JL, Mikhail E (2019) Laparoscopic surgeon´s perspectives on risk factors and prophylaxis of trocar site hernias. JSLS. 2: e2019.00013.
- Gutierrez M, Stuparich M, Behbehani S, Nahas S (2020) Does closure of fascia, type, and location of trocar influence port-site hernia occurrence? Surg Endosc. 12: 5250-5258.
- Ishii M, Okuya K, Miyo M, Miura R, Toyota M, et al (2025) Safety and efficacy of a 12-mm trocar with integrated fascial closure for preventing port-site hernia in minimally invasive abdominal surgery: a multicenter prospective observational study among over weight patients with thick abdominal walls. Surg Endosc.
- Matthews BD, Heniford BT, Sing RF (2001) Preperitoneal Richter hernia after laparoscopic gastric bypass. Surg Laparosc Endosc Percutan Tech. 1: 47-49.
- Ebrahimi R, Kermansaravi M, Eghbali F, Pazouki A (2019) Gastric remnant perforation due to trocar site herniation after laparoscopic Roux-en-Y gastric bypass. Ann R Coll Surg Engl. 3: e88-e90.
- López-Negrete Cueto E, Suárez Sánchez A, Rodicio Miravalles JL, Amoza Pais S, Moreno Gijón M, et al (2025) Ultrasound study of trocar site hernia after bariatric surgery: medium and long-term follow-up. J Abdom Wall Surg. 4: 15002.
- Loret N, De Visschere M, Berwouts L (2017) Unusual presentation of trocar site hernia after gastric bypass. Acta Chir Belg. 1: 61-63.
- Richards Y (2023) Port-site hernias in patients undergoing laparoscopic or robotic surgery: can they be prevented? J Perioper Pract. 9: 269-275.
- Damani T, James L, Fisher JC, Shah PC (2021) Incidence of acute postoperative robotic port-site hernias. J Robot Surg. 15:457-463.
- Rebibo L, Demouron M, Dembinski J, Dhahri A, Yzet T, et al (2019) Impact of Routine 12 Mm Epigastric Trocar Site Closure on Incisional Hernia After Sleeve Gastrectomy: A Prospective Before/After Study. OBES SURG.11: 3500-3507.
- Ece I, Yilmaz H, Alptekin H, Yormaz S, Colak B, et al (2018) Port site hernia after laparoscopic sleeve gastrectomy: a retrospective cohort study of 352 patients. Updates Surg. 1: 91-95.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.