Acute Irreducible Anterior Shoulder Dislocation from Engaged Hill-Sachs Lesion: in Resource Limited Setup
by Adonias A1, Fentahun M1*, Melese G1, Ageru Z2, Alazar M1, Habtamu M1
1Department of Orthopedics and Trauma Surgery, Black Lion Specialized Hospital, Addis Ababa University, Ethiopia
2Departments of Pediatrics and Child health, Black Lion Specialized Hospital, Addis Ababa University, Ethiopia
*Corresponding author: Fentahun Melese, Department of Orthopedics and Trauma, Black Lion Specialized Hospital, Addis Ababa University, Addis Ababa, Ethiopia
Received Date: 14 March, 2025
Accepted Date: 24 March, 2025
Published Date: 26 March, 2025
Citation: Adonias A, Fentahun M, Melese G, Ageru Z, Alazar M, Habtamu M (2025) Acute Irreducible Anterior Shoulder Dislocation from Engaged Hill-Sachs Lesion: in Resource Limited Setup. J Orthop Res Ther 10: 1380. https://doi.org/10.29011/2575-8241.001380
Introduction
The gleno-humeral joint, often regarded as one of the most dynamically mobile joints within the human body, exemplifies a remarkable range of motion that is unparalleled among the various joints. This extreme mobility, while essential for numerous activities and functions, but makes the gleno-humeral articulation particularly vulnerable to dislocation and subluxation events. In general, clinical datas indicate that shoulder dislocations comprise approximately 50% of all joint dislocations encountered in medical practice, underscoring the prevalence and significance of this injury within the realm of orthopaedics.
It is worthy that a substantial amount of these dislocations-estimated to be between 12% and 15%-is associated with avulsion fractures of the greater tuberosity [1]. This integration highlights the complexity of shoulder dislocations and points avulsion fractures as the predominant complication linked with anterior shoulder dislocations. The complex anatomy of the shoulder, together with the forces exerted during dislocation events, leads to the occurrence of such complications, necessitating a thorough understanding of the underlying mechanisms involved.
Several issues can impede the successful reduction of shoulder dislocations, which are often identified as blocking agents. These agents may arise from various soft tissue structures, including the subscapularis muscle [1,4,5,7], the tendon of the long head of the biceps [2], or the glenoid labrum [3]. Additionally, bony tissue factors, such as loose fragments from the glenoid or fractures involving the greater tuberosity [4,8], can further impede the reduction process. Though the challenges, it is important to emphasize that the overall occurrence of irreducible shoulder dislocations remains relatively rare, which may provide some reassurance to both clinicians and patients alike.
In this presentation, we shall delineate our comprehensive approach to the management of irreducible shoulder dislocations, with a particular focus on the technique of open reduction accompanied by infraspinatus remplissage. This strategic intervention is specifically designed to address significant Hill-Sachs lesions, which are often encountered in conjunction with anterior dislocations. By employing this technique, we aim to enhance the stability of the shoulder joint and mitigate the risk of future dislocation episodes, thereby improving patient outcomes and restoring functional capacity. Through a detailed exploration of the rationale, methodology, and anticipated benefits of this approach, we hope to contribute to the ongoing discourse surrounding the effective management of shoulder dislocations and their associated complications.
Case Presentation
A 24-year-old right-handed man, who is a college graduate, presented to the trauma emergency department after sustaining a fall that affected the right side of his body from an approximate height of four meters ladder. He experienced severe shoulder pain and was unable to use his hand. A clinical examination revealed a box-like appearance of the right shoulder, along with a loss of the right deltoid muscle contour. The limb was positioned in slight abduction and external rotation, and it was relatively locked in a 45-degree external rotation. The glenoid appeared to be empty.
Otherwise, there were no neurological deficits in the territories of the median, ulnar, radial, and axillary nerves. Brachial, ulnar, and radial pulses were palpable. The examination of the remaining musculoskeletal system was unremarkable. He has no known medical or surgical illness.
An initial imaging assessment was conducted with a single Anterio-posterior X-ray while the patient was in a supine position. The imaging revealed an anterior shoulder dislocation with no visible associated fractures.

Figure 1: Shoulder AP X-ray with anterior shoulder dislocation.
The orthopedic team made two attempts to achieve reduction under sedation in the emergency department; however, both efforts were unsuccessful. Due to the ongoing dislocation, further imaging studies were deemed necessary to evaluate the shoulder joint more thoroughly.
Subsequent imaging was conducted using an anteroposterior (AP) shoulder X-ray while the patient was positioned supine. This imaging confirmed the presence of a persistent dislocation, prompting the need for additional diagnostic evaluation. As a result, a computed tomography (CT) scan of the shoulder was performed to obtain a more detailed view of the involved bony and soft tissue structures.
The CT scan revealed an anterior shoulder dislocation accompanied by a significant Hill-Sachs defect, which was found to be engaged with the glenoid rim. This finding is particularly significant, as it suggests a potential complication that could hinder future reduction attempts and affect the overall stability of the shoulder joint. Additionally, the imaging indicated a shallow anterior glenoid rim, which may further contribute to the joint's instability. Notably, the soft tissue window of the CT scan appeared normal, indicating that there were no major soft tissue injuries associated with the dislocation.
These findings highlight the complexity of the case and emphasize the necessity for a carefully considered management approach, taking into account the anatomical and pathological factors identified through imaging. The persistence of the dislocation, along with the presence of a substantial Hill-Sachs defect and a shallow glenoid rim, calls for a thorough discussion regarding potential surgical interventions aimed at restoring stability and function to the shoulder joint.
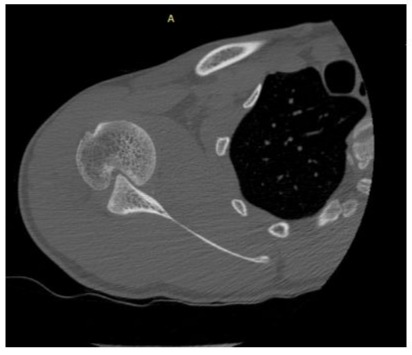
Figure 2: Axial view CT scan revealed big hill-sachs defect with an engaged glenoid.

Figure 3: Coronal view of right shoulder CT scan.

Figure 4: Sagittal view of right shoulder CT scan.
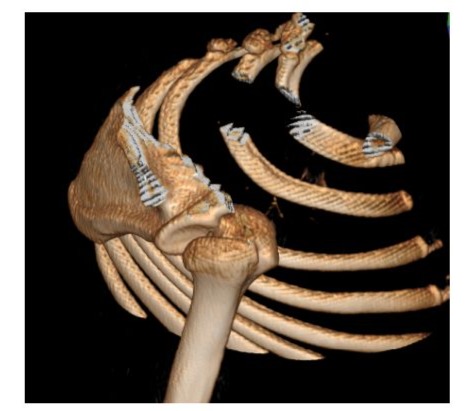
Figure 5: 3D view of right shoulder.
The patient was admitted to the operating room for an open reduction procedure under general anesthesia. To optimize visualization and facilitate access to the surgical site, the patient was held in a beach chair position.
An initial attempt at closed reduction was performed under general anesthesia; however, this attempt proved unsuccessful. Consequently, the surgical team determined that an open reduction procedure was imperative. The surgical approach utilized a deltoid-splitting technique, characterized by an incision made between the middle and posterior deltoid muscles. This method provided direct access to the joint while minimizing trauma to the surrounding muscular structures.
Upon gaining access, the fracture/dislocation was identified, and successful open reduction was conducted to reposition the dislocated humeral head, employing a Shanz pin as an aid. The infraspinatus muscle was meticulously tagged and secured to the Hill-Sachs defect using an anchor suture. After achieving hemostasis, the deltoid muscle was approximated, and the surgical site was meticulously closed in layers. The skin was sutured using 2-0 absorbable suture.
The surgical site was then appropriately dressed to mitigate the risk of infection. Postoperative pain management strategies were implemented, and a comprehensive rehabilitation protocol will be discussed with the physical therapist to ensure optimal recovery for the patient. Following the surgical procedure, the shoulder was immobilized with a universal shoulder immobilizer for a duration of two weeks. Subsequently, a regimen of progressive shoulder range of motion exercises was initiated. At the six-week follow-up, the patient exhibited a stable shoulder with abduction achieved up to 120 degrees, as well as a functional range of flexion, extension, and rotation, all without any reported shoulder pain.
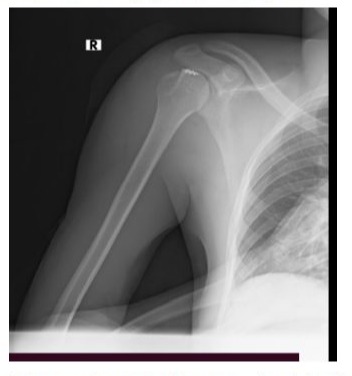
Figure 6: Postoperative AP shoulder x-ray-reduced shoulder joint anchor suture in situ.

Figure 7: 6 weeks post-operative photo.
Discussion
Irreducible Anterior shoulder dislocation is rare when there is no associated proximal humerus fracture. A review conducted by Guha and Jago in 2004 [6] found that merely ten cases of irreducible anterior shoulder dislocation have been documented over the last 35 years, with the majority occurring in males and only one patient being younger than 45. Plenty of mechanical factors can impair reduction, including a dislocated tendon of the long head of the biceps [2], a displaced glenoid labrum [3], bony fragments from the glenoid or greater tuberosity [4,8], and the subscapularis tendon [1,4,5,7]. Specifically, the subscapularis may hinder reduction when it is tightly stretched across the front of the joint, causing the anterior lip of the glenoid to be trapped in a large Hill-Sachs defect, which is located in the posterior-superior aspect of the humeral head. Specifically, the subscapularis may block reduction when it is tightly stretched across the front of the joint, causing the anterior lip of the glenoid to become trapped in a large Hill-Sachs defect located on the postero-superior aspect of the humeral head.
In our case, the anterio-medial glenoid rim was engaged in the large Hill-Sachs defect, marking our first encounter with this situation. Intraoperatively, the significant Hill-Sachs defect was visible and was filled and fixed using the infraspinatus tendon with an anchor suture. The remaining soft tissue was reinforced with strong sutures. Following this remplissage procedure, the shoulder demonstrated stability across all ranges of motion.
We suggest that in an unusual situation when closed reduction of anterior shoulder dislocation is difficult, particularly in the absence of a visible fracture, considering an engaged Hill-Sachs defect will be a valuable differential.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
Adonias Ager and Fenthahun Melese conceived the study project, followed the patients, collected the data, and drafted the article. Melese G., the main surgeon, followed the patients and revised and approved the final version of the article.
Funding
No funding was obtained or sought, as this is a case report that describes the patients we evaluated, treated, and followed.
Acknowledgments
We would like to thank our radiology department's CT interpretations and orthopedics head, who provide technical support.
Reference
- Ilahi OA (1998) Irreducible anterior shoulder dislocation with fracture of the greater tuberosity. American journal of orthopedics (Belle Mead NJ) 27(8): 576-578.
- Michael S, David M Epstein, Brett H Young, Laith M Jazrawi (2010) Irreducible Anterior and Posterior Dislocation of the Shoulder due to Incarceration of the Biceps Tendon. International Journal of Shoulder Surgery 4(3): 83.
- Mihata T, M Doi, M Abe (2000) Irreducible Acute Anterior Dislocation of the Shoulder Caused by Interposed Fragment of the Anterior Glenoid Rim. J Orthop Sci 5(4): 404-446.
- Kuhnen W, RJ Groves (1979) Irreducible Acute Anterior Dislocation of the Shoulder: Case Report.” Clinical Orthopaedics and Related Research 139: 167-168.
- Lam SJ (1966) Irreducible Anterior Dislocation of the Shoulder. The Journal of Bone and Joint Surgery. British Volume 48(1): 132-133.
- Guha AR, ER Jago (2004) Irreducible Acute Anterior Shoulder Dislocation. International Journal of Clinical Practice 58(12): 1184-1186.
- Ayoubi Rami, Talal Najm, Joseph Maalouly, Dany Aouad, Vladimir Kanj (2021) Irreducible Anterior Shoulder Dislocation with Interposition of the Lesser Tuberosity and Subscapularis. Trauma Case Reports 32: 100429.
- Davies MB, C Rajasekhar, M S Bhamra (2000) Irreducible Anterior Shoulder Dislocation: The Greater Tuberosity Hill–Sachs Lesion.” Injury 31(6): 470–471.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.