Acute Bowel Obstruction: A Rare Circumstance of Prostate Cancer Discover
by Gnabro Gnakouri Alain-P1-4, Vodi Clément Cyrille1-4*, Kramo Nykan F1-4, Odo Biti Adé2-4, Ehui Yannick3-4, Fofana Abroulaye1-4, Drabo Ali1-4, Coulibaly Issoufou1-4, Konan Kevin1-4, Kouame Benjamin1-4, Konan Paul-Gerard1-4, Dekou Angoran H1-4
1Department of Urology, The University Hospital Center of Cocody, Abidjan, Côte d’Ivoire
2Department of Medical Oncology, The University Hospital Center of Treichville, Abidjan, Côte d’Ivoire
3Department of Anatomical Pathology, The University Hospital Center of Cocody, Abidjan, Côte d’Ivoire
4Félix-Houphouët Boigny, University of Abidjan, Côte d’Ivoire
*Corresponding author: VODI Clément Cyrille, Department of Urology, The University Hospital Center of Cocody, Abidjan, Côte d’Ivoire
Received Date: 25 July 2025
Accepted Date: 28 July 2025
Published Date: 30 July 2025
Citation: Alain-P GG, Cyrille VC, Nykan F K, Adé OB, Yannick E, et al. (2025) Acute Bowel Obstruction: A Rare Circumstance of Prostate Cancer Discover. J Urol Ren Dis 09: 1429. https://doi.org/10.29011/2575-7903.001429.
Abstract
Introduction: Prostate cancer is the leading cancer in incidence and mortality in Ivory Coast. The diagnosis is most often made at locally invasive or metastatic stages. However, extension to the rectum with acute digestive symptoms is rare, and can mimic primary rectal cancer.
Case presentation: We reported a case of a 69-year-old patient who presented with acute bowel obstruction due to a tumor filling the rectal lumen. The initial diagnosis of rectal cancer was revoked by histological analysis of the biopsy of this tumor which concluded that it was acinar adenocarcinoma of the prostate Gleason 9 (4+5) confirmed with immunohistochemical staining for prostate specific antigen. We performed colostomy followed by Androgen Deprivation Therapy (ADT) combined to chemotherapy. The evolution 11 months after surgery was marked by the occurrence of resistance to castration. The indication for second-line treatment with abiraterone acetate was not observe by the patient and the patient's death occurred in the 15th month following surgery.
Conclusion: Acute bowel obstruction due to rectal involvement by prostate cancer is rare and mimics rectal cancer. Histopathology and immunohistochemistry are essential for accurate diagnosis.
Keywords: Acute Large Bowel Obstruction; Histopathology; Immunohistochemistry; Prostate Cancer; Rectal Invasion
Introduction
Prostate cancer is a major public health problem worldwide. In Ivory Coast, it is the most common cancer in both genders, with 4041 cases in 2022, or 18.9% of all cancers, and the leading cause of cancer death with 2216 deaths in 2022, thus 15.7% of all cancer deaths [1]. Unlike developed countries, the majority of patients are still diagnosed at locally invasive or metastatic stages [2]. The circumstances of discovery are dominated by Lower Urinary Tract Symptoms (LUTS), poor general condition and bone pain respectively [3]. However, there are atypical clinical presentations that can sometimes mimic other conditions, thus delaying diagnosis and treatment. Indeed, a digestive symptomatology in the forefront following rectal involvement of prostate cancer remains rare [4]; thus, posing the problem of differential diagnosis with primary rectal cancer [5]. In addition, this clinical form requires multidisciplinary management and a treatment that is most often multimodal, combining bypass or surgical resection with hormonal treatment. We report a case of metastatic prostate cancer revealed by acute large bowel obstruction following invasion of the rectum.
Case Presentation
This was a 69-year-old patient who had been admitted at the surgical emergency department for painful abdominal distension associated with constipation and absence of flatus evolving for 3 days before his admission. The medical observation revealed symptoms evolving for more than a year consisting of alternating episode of diarrhea and constipation, 2 episodes of proctorrhagia 3 and 2 months ago. which were associated with significant weight loss (> 10% of body weight), asthenia and anorexia. However, the patient did not report any lower urinary tract symptoms. The physical examination noted a poor general condition (ECOG Performance Status Scale Grade 3), a distension of the abdomen, tender and increase percussion node, a large stony mass with an irregular surface, painless, filling the entire rectal lumen, with the absence of stool on the examination finger. The rest of the physical examination revealed no other abnormalities. The abdomino-pelvic CT performed (Figure 1).
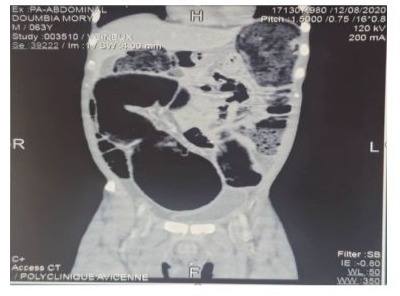
Figure 1: Abdominal-pelvic CT sagittal section showing a low colonic occlusion of mechanical origin
concluded that there was a complete mechanical digestive obstruction by a tumor occupying the entire lumen of the middle rectum with extension to the prostate. The diagnostic hypotheses mentioned were: locally advanced obstructive rectal cancer or prostate cancer with invasion of the rectum. The initial diagnosis was that of an obstructive rectal tumor on preliminary clinical-radiological data. An emergency bowel bypass by a bi-tubular colostomy with biopsy of the rectal mass was performed to diagnostic confirmation. The histopathological examination of the biopsy fragment concluded that adenocarcinoma of the prostate was Gleason 9 (4+5): ISUP 5. (Figure 2).

Figure 2: (HE x10) poorly differentiated acinar adenocarcinoma of the prostate with Gleason score 9 (4+5) i.e. a grade ISUP 5. The tumor architecture is made up of fused glands creating cribriform masses and layers (black star) within a fibromuscular stroma (blue star).
The total PSA performed at 3 weeks postoperatively was 129 ng/ml. A transrectal ultrasound-guided biopsy of the mass was performed after surgery to avoid misunderstanding an associated primary rectal tumor which also concluded that it was a prostatic acinar adenocarcinoma Gleason 9 (4+5): ISUP 5 confirmed with immunohistochemical staining for prostate specific antigen. The extension assessment that was carried out after the histological diagnosis included:
- MRI of the pelvis (Figure 3). showed: hypertrophic tumor of the prostatic gland with intrusion of the capsule, invasion of the seminal vesicles and floor crossing of the Denonvilliers' fascia and circumferential infiltration of the middle rectum associated with external and internal iliac pelvic lymphadenopathy.
- A Bone scintigraphy showed spinal bone metastasis in L1, L2, L3 and L4 and metastasis in the left iliac crest.
- Abdominal CT scan performed before surgery reenforce by a chest CT scan that did not observe secondary visceral lesions.
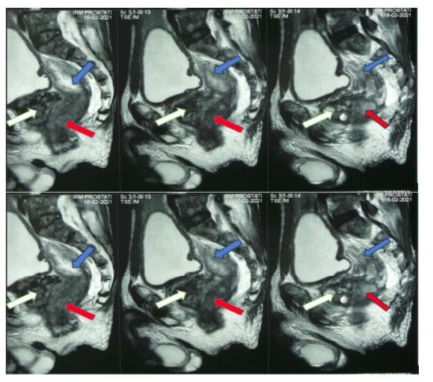
Figure 3: Pelvic MRI sagittal and cross-sectional showing a prostate tumor with invasion of the rectum. White arrow: prostate, blue arrow: rectal lumen, red arrow: tumor invading the rectum.
The working diagnosis was prostate acinar adenocarcinoma ISUP 5 T4N1M1b. The background treatment was concomitant hormonal chemotherapy combining: Bilateral testicular pulpectomy docetaxel 75 mg/m2 every 3 weeks for 8 weeks Prednisone 10 mg/day Monitoring methods included a physical examination, a total PSA, and a pelvic ultrasound. The monitoring rhythm was monthly for the first three months, then each trimester from the third month onwards. At the digestive level, it was planned to restore digestive continuity in there is a reduction in the tumor volume or, on the opposite, a pelvic exenteration if the patient's physical condition had allowed it. Evolution under treatment:
- in the third month: We noted an improvement in clinical condition marked by a general condition from ECOG Performance Status Grade 3 to grade 1, weight gain and a regression of asthenia and anorexia with a total PSA of 51 ng/ml however; The digital rectal examination and pelvic ultrasound showed a lack of regression in the volume of the tumor still obstructing the rectal lumen.
- In the sixth month: clinical improvement, patient with a ECOG Performance Status Grade 3 to grade 1, PSA nadir at 31 ng/ml, digital rectal examination and pelvic ultrasound still showed no regression in the volume of the tumor still obstructing the rectal lumen.
- In the eleventh month: the onset of vertebral bone pain led the patient to consult and he was found with an alteration of the general condition ECOG Performance Status Grade 3 associated with a reascent of the total PSA on 3 successive analyses at 2 weeks apart at 102ng/ml, 112ng/ml and 134 ng/ml with a total serum testosterone of 0.37ng/dl.
We concluded that Castrate-Resistant Metastatic Prostate Cancer (mCRPC) with advancement on chemotherapy. The patient was offered a second line of therapy with the addition of abiraterone acetate to the previous treatment. The patient had not been able to compile to the treatment due to lack of financial means and the patient's death occurred in the fifteenth month.
Discussion
Rectal involvement of prostate cancer is around 4% with extremes ranging from 1 to 12% as evidenced by several autopsy series [4]. This could be explained by the presence of Denonvilliers’ fascia, which represents an anatomical barrier to the invasion of the rectum [6]. Involvement of the rectum can potentially occur by 3 routes, in particular by contiguity by directly invading the fascia of Denonvilliers and then the rectal wall, by lymphatic route, and by propagation of prostate cancer cells from biopsy sample [7]. In the literature, acute intestinal occlusion represents a rarely reported circumstance of prostate cancer discovery [4]. In Ivory Coast, it seems to be first reported case revealed by an acute bowel occlusion. Clinical expressions of rectal involvement in prostate cancer are nonspecific; the most reported in the literature being proctorrhagia, alternating constipation and diarrhea, pelvic perineal pain [8]. Acute bowel obstruction combining abdominal pain, distension and absence of bowel movement and flatus is rarely described [9]. This clinical presentation in our patient can be explained by a long consultation delay; On the other hand, the majority of series have shorter consultation times. In addition, the digestive signs are rarely isolated, most often associated with LUTS; however, our patient did not describe any LUTS showing that, although absent, the possibility of advanced prostate cancer should always be considered by the clinician as a plausible etiology in the face of digestive symptoms associated with an alteration in general condition. This clinical presentation is most often observed in the context of a negative course of prostate cancer, which has already been diagnosed and treated or not [8]. The digital rectal examination, although it makes it possible to suspect a prostatic cause of the obstruction, cannot make it possible to distinguish it from a primary rectal involvement [10]. An elevation of total PSA can be observed both in primary prostate involvement and secondary prostate involvement by a pelvic tumor; conversely, a normal total PSA, although weighting in favour of primary rectal involvement, does not allow prostate cancer to be formally excluded [11].
Imaging, particularly MRI, can be of great help in the diagnosis of primary prostate cancer, but above all it can help pre-evaluated in case of surgery to removal the tumor [12]. Rectal endoscopy with biopsy and histopathological examination is also a diagnostic modality [7]. Anatomical pathology remains the cornerstone of the diagnosis by affirming the prostatic origin of the tumor, the histological type and then giving prognostic elements such as the ISUP score; However, acinar adenocarcinoma of the prostate and rectum with many common histopathological features may require immunohistochemistry to confirm the prostatic or rectal origin of the tumor [13]. In this clinical situation, emergency digestive surgery (colostomy/uni or bitubular ileostomy) remains the main approach; There is no evidence in the literature of the lifting of bowel obstruction by mechanical obstruction of the rectum after specific or non-specific medical treatment of prostate cancer [4]. The treatment is multidisciplinary at least involving digestive surgeons, urologists, oncologists and sometimes radiotherapists. This surgical treatment to remove the obstacle is associated with a specific treatment of prostate cancer depending on the stage of progression; In our case, we performed a bitubular colostomy to which we combined hormonal chemotherapy from the outset combining bilateral testicular pulpectomy with docetaxel. However, although the literature shows a beneficial effect of local treatment by radiotherapy [14] or total prostatectomy [15] in the case of locally advanced or oligometastatic cancer, allowing tumor reduction and clinical improvement; on the contrary, it is deleterious in metastatic patients, even those with a good general condition [8]. Rectal involvement of prostate cancer is evidence of a disease that is most often advanced. Although overall survival is less than 30 months in many series; Studies on prognosis vary. In the series by Ogasawara et al. Overall survival at 1, 3 and 5 years was approximately 68.3% ±5.3%, 54.4% ±7.2% and 38.8% ±11.1% [15] while Bowrey's median survival was 15 months [4]. Our result seems to be similar to Bowrey's because of the similar characteristics of most of the patients in this series to ours: patient in the metastatic stage at the time of diagnosis, hormonenaïve. Although our patient had a clinical and biological improvement at M3 and then at M6, we nevertheless noted the persistence of the tumor with obstruction of the rectum which did not allow us to consider the restoration of digestive continuity. The death of our patient, although occurring within the time frame mentioned in the literature, could theoretically be delayed by abiraterone acetate [16].
Conclusion
Rectal involvement of prostate cancer remains uncommon, and acute large bowel obstruction is an exceptional circumstance of discovery. The diagnosis, although helped by MRI, has as its cornerstone histology, which makes it possible to eliminate any diagnostic doubt and to adapt the background treatment. The performance of a digestive bypass combined with androgen deprivation treatment remains the basis of treatment. However, performing a local treatment such as total pelvic exenteration would appear to improve quality of life but not overall survival.
Author’s contributions: Gnabro Alain drafted the manuscript and assisted with the clinical data collection and interpretation
Vodi Clement and Kramo Nykan performed surgery and participate in collectind data
Odo Bitti and Ehui Yannick contributed to pathological examination and diagnosis
Availability of data and materials: All data generated or analyzed during this case are included within the article.
Declarations
Consent for publication: All authors consent to the publication of the manuscript in Journal of Case Report and Images in Urology
References
- Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, et al. (2024) Global cancer statistics 2022 : GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 74: 229‑263.
- Ludovic NBP, Addé OB, Christian NT, Yvon KK, Gaetan KZA, et al. (2021) Cancer de la prostate chez le sujet de race noire en Côte d’Ivoire 23: 49-54.
- Konan P, Gowe E, Dekou A, Fofana A, Vodi C (2015) CANCER METASTATIQUE DE LA PROSTATE DANS LE SERVICE D’UROLOGIE DU CHU DE COCODY. Uro’Andro 1: 172‑176.
- Bowrey DJ, Otter MI, Billings PJ (2003) Rectal infiltration by prostatic adenocarcinoma : report on six patients and review of the literature. Ann R Coll Surg Engl 85: 382‑385.
- Fry DE, Amin M, Harbrecht PJ (1979) Rectal obstruction secondary to carcinoma of the prostate. Ann Surg. Avr 189: 488‑492.
- Tzelves L, Protogerou V, Varkarakis I (2022) Denonvilliers’ Fascia : The Prostate Border to the Outside World. Cancers 14: 688.
- Yoon G, Han MH, Seo AN (2019) Rectal Invasion by Prostatic Adenocarcinoma That Was Initially Diagnosed in a Rectal Polyp on Colonoscopy. J Pathol Transl Med. Juill 53: 266‑269.
- Wang H, Yao Y, Li B (2014) Factors associated with the survival of prostate cancer patients with rectal involvement. Diagn Pathol 9: 35.
- Lebret T, Méjean A (2008) [Rare locations of metastases from prostate cancer]. Progres En Urol J Assoc Francaise Urol Soc Francaise Urol 7: S357-364.
- Khadem TH, Rosenberg J, Achiam MP (2013) [Digital rectal examination is a useful clinical procedure in the work-up of patients with colorectal or urogenital symptoms]. Ugeskr Laeger 175: 2636‑2639.
- Gallee MP, Visser-de Jong E, van der Korput JA, van der Kwast TH, ten Kate FJ, et al. (1990) Variation of prostate-specific antigen expression in different tumour growth patterns present in prostatectomy specimens. Urol Res 18: 181‑187.
- Lagabrielle S, Descat E, Piechaud T, Lebras Y, Dupin C, et al. (2016) L’IRM multiparamétrique dans l’évaluation des cancers de prostate localement avancés, corrélation avec les pièces d’anatomopathologie. Prog En Urol 26: 814‑815.
- Gan Q, Joseph CT, Guo M, Zhang M, Sun X, et al. (2019) Utility of NKX3.1 Immunostaining in the Detection of Metastatic Prostatic Carcinoma on Fine-Needle Aspiration Smears. Am J Clin Pathol 152: 495‑501.
- Lee MJ (2024) Prostate cancer invading rectal serosa and anal sphincter treated with definitive radiation therapy : Case report and review of the literature. J Cancer Res Ther 20: 1081-1084.
- Ogasawara RA, Okubo N, Nakanishi Y, Imasato N, Hirose K, et al. (2023) Laparoscopic total pelvic exenteration combined with transanal total mesorectal excision for locally advanced prostate cancer with rectal infiltration. IJU Case Rep 7: 83‑86.
- Fizazi K, Foulon S, Carles J, Roubaud G, McDermott R, et al. (2022) Abiraterone plus prednisone added to androgen deprivation therapy and docetaxel in de novo metastatic castration-sensitive prostate cancer (PEACE-1) : a multicentre, open-label, randomised, phase 3 study with a 2 × 2 factorial design. The Lancet 399: 1695‑707.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.