A Systemic Approach to Aging and Anti-Aging Interventions:A Mini-Review
by Chuan-Yuan Lin1,2, Jui-Yu Lin1,2*, Konstantin Frank3, Sachithevi Sivananthan4,5,Carmelo Crisafulli6, Waranaree Winayanuwattikun7, Antonina A. Gorskaya8, Lim-Kai Toh9
1Li-An Medical Clinic, Taipei 104452, Taiwan
2RX-Aesthetic Ltd., Hong Kong
3Center of Plastic, Aesthetic, Hand and Reconstructive Surgery, University Hospital Regensburg, Regensburg, Germany
4FMC Clinic, Dubai, UAE
5Sandalwood Medical, UK
6Gulglam Clinics, Dubai, UAE
7Division of Dermatology, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
8Clinics of Aesthetic Medicine “O’Live”, Nizhny Novgorod, Russia
9Doctors for Life Medical, Singapore
*Corresponding Author: Jui-Yu Lin, Li-An Medical Clinic, 4F., No. 267, Lequn 2nd Rd., Zhongshan Dist., Taipei City 104452, Taiwan
Received Date: 30 April 2025
Accepted Date: 04 June 2025
Published Date: 06 June 2025
Citation: Lin CY, Lin JY, Frank K, Sivananthan S, Crisafulli C, et al. (2025) A Systemic Approach to Aging and Anti-Aging Interventions:A Mini-Review. J Surg 10: 11344 https://doi.org/10.29011/2575-9760.011344
Abstract
Aging is a multifaceted biological process characterized by gradual molecular and cellular deterioration across various systems of the body, including the musculoskeletal, neurological, integumentary, and connective tissue systems. This mini-review explores the pathophysiology of aging in these seven key systems-bone, fat, muscle, neurological, vascular, connective tissue, and skin-highlighting the underlying mechanisms such as chronic inflammation, stem cell exhaustion, and genomic instability. Recent advancements in anti-aging therapies emphasize a multi-system, holistic approach that recognizes the interconnectedness of aging processes. Emerging treatments, including regenerative medicine, biostimulators, and personalized therapies, offer promising strategies for rejuvenating multiple systems simultaneously, thus enhancing overall health and mitigating the impact of age-related decline. The review also discusses the potential of stem cell therapies, gene editing, and longevity science in addressing the molecular basis of aging, alongside the role of lifestyle modifications and emerging technologies. As research progresses, the integration of regenerative approaches, genetic interventions, and personalized medicine holds the potential to transform aging from a passive process into an actively managed and rejuvenated state, improving both quality of life and longevity.
Keywords: Aging; Anti-aging interventions; Longevity science; Multi-system rejuvenation; Personalized medicine; Regenerative medicine; Senescence
Introduction
Aging is a complex biological process marked by progressive molecular and cellular damage, leading to the gradual deterioration of structure and function across multiple body systems. At the cellular level, this process is characterized by genomic instability, telomere attrition, epigenetic alterations, and loss of proteostasis-mechanisms now collectively defined as the “Hallmarks of Aging” [1]. Although aging impacts all organs and tissues, the most prominent changes are observed in systems responsible for mobility (musculoskeletal), cognition (neurological), and appearance (integumentary and connective tissue). These changes often arise from shared pathological mechanisms, such as chronic inflammation and stem cell exhaustion, which are increasingly recognized as fundamental drivers of multi-system decline [1-3] In recent years, anti-aging research has shifted from a primarily cosmetic focus toward a broader paradigm of systemic rejuvenation, acknowledging that interventions targeting a single system often confer pleiotropic benefits across others [4]. For instance, senolytic therapies not only eliminate senescent cells in the skin but also enhance vascular function and promote muscle regeneration [5]. Likewise, exercise-traditionally valued for maintaining muscle mass-has been shown to stimulate neurogenesis and improve bone density, primarily through myokine-mediated signaling pathways [6’7] . This interconnectedness highlights the importance of adopting a multi-system approach in modern anti-aging strategies. Understanding mechanisms of crosstalk-such as how osteocalcin from bone influences brain function or how adipose tissue senescence accelerates vascular stiffening-is essential for developing comprehensive interventions. Emerging frameworks, such as 'geroscience,' now focus on targeting fundamental aging processes to delay the onset of multiple age-related conditions simultaneously [1,3]. This mini-review explores the pathophysiology of aging across seven key systems-bone, fat, muscle, neurological, vascular, connective tissue, and skin-examining both established and emerging rejuvenation strategies. (Figure 1; Table 1) It highlights how combinatorial approaches may act synergistically to counteract cross-system decline, while also addressing current translational challenges such as the optimization of personalized treatment protocols.
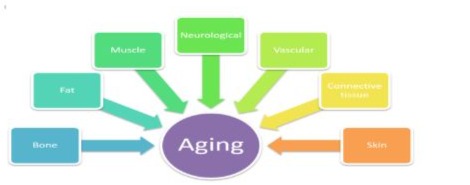
Figure 1: Multi-system aging.
|
System |
Age-related Pathology |
Current/Rejuvenation Strategies |
|
Bone |
Osteoporosis |
Bisphosphonates, vitamin D, stem cell therapy |
|
Fat |
Fat atrophy |
Fat grafting, SCAFs, adipose-derived stem cells |
|
Muscle |
Sarcopenia |
Resistance training, protein supplementation, myostatin inhibitors |
|
Neurological |
Neurodegeneration |
NAD+ boosters, neurotrophic factors, CRISPR, senolytics |
|
Vascular |
Vascular stiffening |
Anti-hypertensives, caloric restriction, senotherapeutics |
|
Connective Tissue |
Connective tissue degradation |
Collagen stimulators, retinoids, bio-regenerative scaffolds |
|
Skin |
Dermal atrophy |
Topical retinoids, lasers, PRP, biostimulators (e.g., PLA) |
Table 1: Aging pathologies and treatment by system.
Aging Pathology and Anti-aging Treatment Strategies for Different Systems
Bone System
Aging Pathology: Bone aging is characterized by the accelerated loss of mineral density and trabecular thinning, along with cortical porosity, leading to osteoporosis and fragility fractures [8-10]. A deficiency in dietary calcium triggers a significant increase in RANKL production, particularly in osteocytes, which become the primary drivers of subsequent bone loss [11]. As individuals age, the balance between bone resorption and formation shifts, resulting in increased bone loss, often exacerbated by hormonal changes, particularly in postmenopausal women. Postmenopausal women experience trabecular bone loss due to estrogen withdrawal, which enhances osteoclastogenesis through NF-κB signaling [12]. Regarding facial bone aging, bone resorption, especially in the maxillary and mandibular regions, plays a critical role. This leads to midface retrusion, deepening of the nasolabial folds, and overall facial sagging [13].
Treatment Strategies
- Bone Regeneration Therapies: [14] Techniques such as bone grafting, mesenchymal stem cell therapy, and the application of Bone Morphogenetic Proteins (BMPs) are being investigated for their potential to promote bone growth and repair.
- Pharmacological Interventions: [15] Medications like bisphosphonates and Selective Estrogen Receptor Modulators (SERMs) help reduce bone loss by inhibiting resorption.
- Calcium Hydroxylapatite (CaHA) Injections: [16] These injections are used for periosteal filling, aiding in the restoration of skeletal support.
- Low-Intensity Pulsed Ultrasound (LIPUS): [17] This therapy stimulates bone metabolism and helps delay bone resorption.
- Bioactive Glass Therapy: [18] This therapy releases calcium and phosphate ions, promoting bone regeneration.
Fat System
Aging Pathology: With age, body fat undergoes redistribution, characterized by a decrease in subcutaneous fat and an increase in visceral fat. This shift in fat distribution can lead to changes in body shape, such as the loss of facial volume and the accumulation of fat around internal organs, which increases the risk of metabolic disorders [19]. In terms of facial fat aging, age-related fat compartmentalization results in the loss of deep fat (e.g., SOOF) and the descent of superficial fat, causing an imbalanced facial appearance [20]. Consequently, deep fat atrophy contributes to midface hollowing, while the herniation of superficial fat worsens nasolabial fold prominence [20].
Treatment Strategies
- Adipose-Derived Stem Cells: [21] These cells show promise for regeneration and fat tissue restoration, providing a potential approach for restoring facial volume and reducing visceral fat.
- Fat Repositioning Techniques: [22] Cosmetic procedures such as fat grafting have gained popularity for facial rejuvenation and restoring lost volume in aging individuals.
- Poly-L-Lactic Acid (PLLA) Micro-Spheres: [23] These stimulate collagen production while enhancing the retention of fat grafts.
- Radiofrequency Microneedling (RF-MN): [24] This technique improves skin texture by promoting vascularization and remodeling of adipocytes.
Muscle System
Aging Pathology: Muscle mass and strength decline with age, a condition known as sarcopenia, which leads to functional impairments, frailty, and an increased risk of falls. Sarcopenia is influenced by factors such as reduced protein synthesis, hormonal changes, and physical inactivity [25]. In terms of facial muscle aging, it involves both muscle atrophy and compensatory hyperactivity, resulting in the development of both static and dynamic wrinkles [26]. Additionally, the decline of fast-twitch muscle fibers (e.g., zygomaticus major) with age weakens smile dynamics [27]. Electromyography (EMG) reveals increased involuntary contractions in hypertrophied facial muscles [28].
Treatment Strategies
- Exercise and Nutrition: [29] Resistance training combined with adequate protein intake has been shown to counteract muscle loss and improve strength in aging individuals.
- Regenerative Medicine: [30] The use of satellite cells, myostatin inhibitors, and stem cell therapies is being explored as potential treatments to restore muscle mass and function.
- Targeted Botulinum Toxin (BoNT) Injection: [31] EMG-guided micro-dosing allows for selective muscle relaxation without the risk of over-paralysis.
- Myomodulation with Fillers: [32] Restoring volume can enhance muscle tonicity.
- Microcurrent Stimulation (NuFACE): [33] A randomized trial demonstrated an 18% improvement in muscle tone with this treatment.
Neurological System
Aging Pathology: Aging affects the neurological system through the gradual decline in cognitive functions, including memory, attention, and processing speed. Neurodegenerative diseases such as Alzheimer’s and Parkinson’s are common among older adults, influenced by a combination of genetic, environmental, and lifestyle factors [34]. Age-related neurodegeneration also impacts facial nerve function, impairing skin barrier efficiency and collagen synthesis. The emerging "Neuro-Skin Axis" theory emphasizes the connection between neural pathways and skin health. [35]. Imaging studies show a direct correlation between nerve compression and facial muscle spasticity [36]. With age, axonal density and nerve regeneration capabilities decline, impacting facial expressions and symmetry [37].
Treatment Strategies:
- Cognitive Training and Neuroplasticity: [38] Mental exercises, coupled with cognitive training, aim to enhance brain function and neuroplasticity, thereby promoting cognitive health.
- Pharmacological Interventions: [39] Neuroprotective drugs, such as cholinesterase inhibitors and antioxidants, are being used to slow the progression of neurological decline.
- Exosome Therapy: [40] Exosomes enriched with miR-21 support nerve axon regeneration.
- Fullerenes as Antioxidants: [41] These compounds reduce oxidative stress in nerve endings, enhancing neurotransmission.
- Magnetic Stimulation (TMS): [42] This technique improves neuromuscular coordination and facial expressiveness.
Vascular and Lymphatic Systems
Aging Pathology: Aging results in endothelial dysfunction, arterial stiffening, and an increased risk of cardiovascular diseases such as atherosclerosis and hypertension. These vascular changes contribute to reduced oxygen delivery to tissues, heightening the risk of stroke and heart attack [43]. In terms of facial vascular and lymphatic aging, a decrease in microvascular density leads to a dull skin tone, slower tissue repair, and the accumulation of metabolic waste. The age-related decline in capillary function is further compounded by reduced lymphatic flow, which exacerbates puffiness and inflammation [44].
Treatment Strategies
- Lifestyle Modifications: [45] Regular physical activity, a healthy diet, and smoking cessation are crucial for maintaining vascular health.
- Targeted Therapies: [46] Interventions such as endothelial progenitor cell therapy and the use of vasodilators are being explored to improve vascular health in aging individuals.
- Platelet-Rich Plasma (PRP) Injections: [47] The high VEGF content in PRP promotes angiogenesis and epidermal thickening.
- Low-Level Light Therapy (LLLT): [48] 633nm red light enhances blood flow and endothelial function.
- Nicotinamide Mononucleotide (NMN) Supplementation: [49] This supplementation boosts NAD+ levels, improving endothelial cell function.
- Pulsed Vacuum Drainage: [50] This technique enhances lymphatic circulation, helping to reduce edema.
Connective Tissue System
Aging Pathology: Connective tissues, including ligaments, tendons, and cartilage, undergo degeneration with age, resulting in joint pain, stiffness, and reduced mobility. Collagen production declines, and existing collagen fibers lose their elasticity, which contributes to the physical appearance of aging skin and joints [51]. In the face, the Superficial Musculoaponeurotic System (SMAS) and ligamentous structures are vital for maintaining facial contours. Aging leads to reduced elasticity and progressive sagging, with the SMAS layer losing elastin at a faster rate than the dermis. Ligamentous aging contributes to midface sagging [52].
Treatment Strategies
- Biostimulators: [53,54] Injectable biostimulators, such as AestheFill, stimulate collagen synthesis, enhancing skin texture and elasticity.
- Regenerative Therapies: [47] Stem cell injections and platelet-rich plasma (PRP) treatments show promise in promoting the healing and regeneration of connective tissues.
- Polydioxanone (PDO) Thread Lifting: [55] This technique provides structural support while stimulating collagen synthesis.
- High-Intensity Focused Ultrasound (HIFU): [56] MRI studies have shown improvements in skin tightness following HIFU treatment.
Skin System
Aging Pathology: The skin is one of the most visible indicators of aging, showing changes such as wrinkles, loss of elasticity, and pigmentation irregularities. As the skin loses collagen and elastin over time, it becomes more prone to sagging, thinning, and the formation of fine lines. Aging also impairs keratinocyte turnover and the integrity of the lipid barrier, leading to dryness, rough texture, and heightened sensitivity. As epidermal turnover slows with age, skin regeneration decreases. Additionally, transepidermal water loss increases, contributing to dehydration and irritation [57,58].
Treatment Strategies
- Topical Treatments: [59] Retinoids, antioxidants, and peptides are commonly included in skincare products to promote skin rejuvenation.
- Injectable Fillers and Biostimulators: [60] Hyaluronic acid fillers and biostimulators help restore volume, smooth wrinkles, and stimulate collagen production.
- Regenerative Medicine: [47] Stem cell-based treatments and PRP have shown promise in rejuvenating aging skin by promoting cell regeneration and collagen synthesis.
- Retinoid Microinfusion: [61] Microneedle-assisted delivery enhances the penetration of vitamin A.
- Biomimetic Lipids: [62] Ceramide-based formulations improve moisture retention in the skin.
- Microbiome Regulation: [63] Phage-based skincare selectively targets pathogenic bacteria while preserving beneficial skin flora.
Future Perspectives in Anti-Aging Research
As research into aging and anti-aging interventions advances, the field is shifting toward a more integrated, multi-system approach. Instead of focusing solely on one aspect of aging, emerging therapies are exploring the potential to rejuvenate multiple systems simultaneously. The future of anti-aging research is set to combine regenerative medicine, genetic interventions, and personalized therapies to address the complexities of aging in a more holistic manner. Several key areas for future research include:
- Regenerative Medicine: [14,21,47] Stem cell-based therapies, gene editing, and tissue engineering are among the most promising fields in anti-aging research. By targeting the cellular and molecular mechanisms underlying aging, these therapies could provide a more effective approach to rejuvenation.
- Longevity Science: [1,5] Researchers are increasingly investigating pathways associated with longevity, such as the roles of telomeres, cellular senescence, and autophagy in aging. Understanding and manipulating these processes could offer new opportunities for slowing or even reversing the aging process.
- Personalized Anti-Aging Therapies: [1,34] As we gain a deeper understanding of the genetic, epigenetic, and environmental factors influencing aging, personalized medicine will play a crucial role. Tailored therapies based on individual genetic profiles and lifestyle factors will optimize anti-aging treatments and improve outcomes.
Conclusion
The aging process affects multiple systems within the human body, each requiring distinct yet often interconnected strategies for rejuvenation. From bone density and muscle health to skin rejuvenation and neurological preservation, aging touches all aspects of our physiology. Advancements in anti-aging therapies, such as regenerative medicine, biostimulators, and personalized treatments, are offering promising solutions for healthier aging across these systems. Emerging research into longevity science and the role of cellular mechanisms, such as telomeres, senescence, and autophagy, holds the potential to slow or even reverse certain aspects of aging. By adopting a multi-system, holistic approach, the future of anti-aging medicine is poised to provide more comprehensive and effective interventions, optimizing not only the quality of life but also the longevity of individuals. As science continues to evolve, the integration of genetic, epigenetic, and environmental factors will further refine personalized therapies, enabling us to address the complexities of aging more effectively. Ultimately, these innovations pave the way for a future where aging is not simply endured but actively managed and improved.
Financial Disclosure Statement: No funding was received for this article.
Conflicts of interest: The authors declare no conflicts of interest.
Short Running Head (no more than 40 characters in length): Aging and anti-aging interventions
References
- López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G (2013) The hallmarks of aging. Cell 153: 1194-1217.
- Franceschi C, Garagnani P, Parini P, Giuliani C, Santoro A (2018)Inflammaging: a new immune–metabolic viewpoint for age-related diseases. Nat Rev Endocrinol 14: 576-590.
- Kennedy BK, Berger SL, Brunet A (2014) Geroscience: linking aging to chronic disease. Cell 159: 709-713.
- Campisi J, Kapahi P, Lithgow GJ, Melov S, Newman JC et al. (2019) From discoveries in ageing research to therapeutics for healthy ageing. Nature 571: 183-192.
- Xu M, Pirtskhalava T, Farr JN (2018) Senolytics improve physical function and increase lifespan in old age. Nat Med 24: 1246-1256.
- Pedersen BK, Saltin B (2015) Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports 25: 1-72.
- Pedersen BK (2019) Physical activity and muscle-brain crosstalk. Nat Rev Endocrinol 15: 383-392.
- Riggs BL, Melton LJ (1995) The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone 17: S505-S511.
- Seeman E (2013) Age- and menopause-related bone loss compromise cortical and trabecular microstructure. J Gerontol A Biol Sci Med Sci 68: 1218-1225.
- Johnell O, Kanis JA (2004) Mortality after osteoporotic fractures. Osteoporos Int 15: 38-42.
- Xiong J, Piemontese M, Thostenson JD, Weinstein RS, Manolagas SC et al. (2014) Osteocyte-derived RANKL is a critical mediator of the increased bone resorption caused by dietary calcium deficiency. Bone 66: 146-154.
- Ji M-X, Yu Q (2015) Primary osteoporosis in postmenopausal women. Chronic Dis Transl Med 1: 9-13.
- Mendelson B, Wong C-H (2012) Changes in the facial skeleton with aging: implications and clinical applications in facial rejuvenation. Aesthetic Plast Surg 36: 753-760.
- Scarfì S (2016) Use of bone morphogenetic proteins in mesenchymal stem cell stimulation of cartilage and bone repair. World J Stem Cells 8:1-12.
- Mirkin S, Pickar JH (2015) Selective estrogen receptor modulators (SERMs): a review of clinical data. Maturitas 80: 52-57.
- dos Santos CPC, Cruel PTE, Buchaim DV (2025) Calcium hydroxyapatite combined with photobiomodulation for bone tissue repair: a systematic review. Materials 18:1120.
- Palanisamy P, Alam M, Li S, Chow SKH, Zheng Y-P et al. (2022) Low-intensity pulsed ultrasound stimulation for bone fractures healing: a review. J Ultrasound Med 41: 547-563.
- El-Rashidy AA, Roether JA, Harhaus L, Kneser U, Boccaccini AR et al. (2017) Regenerating bone with bioactive glass scaffolds: a review of in vivo studies in bone defect models. Acta Biomater 62: 1-28.
- Kuk JL, Saunders TJ, Davidson LE, Ross R (2009) Age-related changes in total and regional fat distribution. Ageing Res Rev 8: 339-348.
- Hung WK, Chen CB, Cheng CY (2023) The aging process of deep fat compartments in the midface and midfacial rejuvenation: an ultrasound-based analysis. Dermatol Sin 41: 251-256.
- Qin Y, Ge G, Yang P (2023) An update on adipose-derived stem cells for regenerative medicine: where challenge meets opportunity. Adv Sci 10: e2207334.
- Crowley JS, Kream E, Fabi S, Cohen SR (2021) Facial rejuvenation with fat grafting and fillers. Aesthet Surg J 41: S31-S38.
- Vleggaar D, Fitzgerald R, Lorenc ZP (2014) Consensus recommendations on the use of injectable poly-L-lactic acid for facial and nonfacial volumization. J Drugs Dermatol 13: s44-s51.
- Tan MG, Jo CE, Chapas A, Khetarpal S, Dover JS (2021) Radiofrequency microneedling: a comprehensive and critical review. Dermatol Surg 47: 755-761.
- Kakehi S, Wakabayashi H, Inuma H (2021) Rehabilitation nutrition and exercise therapy for sarcopenia. World J Mens Health 40: 1-10.
- Swift A, Liew S, Weinkle S, Garcia JK, Silberberg MB (2020) The facial aging process from the "inside out." Aesthet Surg J 41: 1107-1119.
- Nilwik R, Snijders T, Leenders M (2013) The decline in skeletal muscle mass with aging is mainly attributed to a reduction in type II muscle fiber size. Exp Gerontol 48: 492-498.
- Valls-Solé J, Montero J (2004) Role of EMG evaluation in muscle hyperactivity syndromes. J Neurol 251: 251-260.
- Gielen E, Beckwée D, Delaere A (2021) Nutritional interventions to improve muscle mass, muscle strength, and physical performance in older people: an umbrella review of systematic reviews and meta-analyses. Nutr Rev 79: 121-147.
- Lee S-J, Huynh TV, Lee Y-S, Fan C-M (2012) Role of satellite cells versus myofibers in muscle hypertrophy induced by inhibition of the myostatin/activin signaling pathway. Proc Natl Acad Sci U S A 109: E2353-E2360.
- Small R (2014) Botulinum toxin injection for facial wrinkles. Am Fam Physician 90: 168-175.
- de Maio M (2020) Myomodulation with injectable fillers: an innovative approach to addressing facial muscle movement. Aesthetic Plast Surg 44: 1300-1316.
- Kolimechkov S, Seijo M, Swaine I (2023) Physiological effects of microcurrent and its application for maximising acute responses and chronic adaptations to exercise. Eur J Appl Physiol 123: 451-465.
- Eggers AE (2009) Why do Alzheimer's disease and Parkinson's disease target the same neurons? Med Hypotheses 72: 698-700.
- Joghataie A, Shafiei Dizaji M (2018) Neuro-Skins: dynamics, plasticity and effect of neuron type and cell size on their response. Neural Process Lett 49: 19-41.
- Lu AY, Yeung JT, Gerrard JL (2014) Hemifacial spasm and neurovascular compression. ScientificWorldJournal 2014: 349319.
- Geoffroy CG, Hilton BJ, Tetzlaff W, Zheng B (2016) Evidence for an age-dependent decline in axon regeneration in the adult mammalian central nervous system. Cell Rep 15: 238-246.
- Kumar J, Patel T, Sugandh F (2023) Innovative approaches and therapies to enhance neuroplasticity and promote recovery in patients with neurological disorders: a narrative review. Cureus 15: e41914.
- Moreira NCDS, Lima JEBF, Marchiori MF, Carvalho I, Sakamoto-Hojo ET (2022) Neuroprotective effects of cholinesterase inhibitors: current scenario in therapies for Alzheimer's disease and future perspectives. J Alzheimers Dis Rep 6: 177-193.
- Liu YP, Yang YD, Mou FF (2022) Exosome-mediated miR-21 was involved in the promotion of structural and functional recovery effect produced by electroacupuncture in sciatic nerve injury. Oxid Med Cell Longev 2022: 7530102.
- Galvan PY, Alperovich I, Zolotukhin P (2017) Fullerenes as anti-aging antioxidants. Curr Aging Sci 10: 56-67.
- Schutter DJ, Enter D, Hoppenbrouwers SS (2009) High-frequency repetitive transcranial magnetic stimulation to the cerebellum and implicit processing of happy facial expressions. J Psychiatry Neurosci 34: 60-65.
- Bentov I, Donato AJ, Machin DR, Lesniewski LA (2018) Mechanisms of dysfunction in the aging vasculature and role in age-related disease. Circ Res 123: 825-848.
- Reed MJ (2015) The effect of aging on the cutaneous microvasculature. Microvasc Res 100: 25-31.
- Ghodeshwar GK, Dube A, Khobragade D (2023) Impact of lifestyle modifications on cardiovascular health: a narrative review. Cureus 15: e42616.
- Ross MD (2018) Endothelial regenerative capacity and aging: influence of diet, exercise and obesity. Curr Cardiol Rev 14: 233-244.
- Patel H, Pundkar A, Shrivastava S, Chandanwale R, Jaiswal AM (2023) A comprehensive review on platelet-rich plasma activation: a key player in accelerating skin wound healing. Cureus 15: e48943.
- Avci P, Gupta A, Sadasivam M (2013) Low-level laser (light) therapy (LLLT) in skin: stimulating, healing, restoring. Semin Cutan Med Surg 32: 41-52.
- Tarantini S, Valcarcel-Ares MN, Toth P (2019) Nicotinamide mononucleotide (NMN) supplementation rescues cerebromicrovascular endothelial function and neurovascular coupling responses and improves cognitive function in aged mice. Redox Biol 24: 101192.
- Liu J, Chen D, Yin X (2023) Effect of manual lymphatic drainage combined with vacuum sealing drainage on axillary web syndrome caused by breast cancer surgery. Int Wound J 20: 183-190.
- Loeser RF (2010) Age-related changes in the musculoskeletal system and the development of osteoarthritis. Clin Geriatr Med 26: 371-386.
- Hînganu MV, Cucu RP, Costan VV (2024) Aging of superficial musculoaponeurotic system of the face-novel biomarkers and micro-CT relevance of facial anti-gravity support. Diagnostics (Basel) 14: 1126.
- Lin JY, Lin CY (2022) Thickness-adjustable injectable poly-D,L-lactic acid: a versatile filler. Plast Reconstr Surg Glob Open 10: e4365.
- Lin JY, Lin CY (2024) The AestheCode system: a safe and efficient guide for AestheFill injection. Aesthetic Plast Surg 49: 2658-2660
- Kim JH, Han MW, Lee MH (2024) Comparative in vivo study of solid-type pure hyaluronic acid in thread form: safety and efficacy compared to hyaluronic acid filler and polydioxanone threads. Aesthetic Plast Surg 48: 221-227.
- Choi SY, No YA, Kim SY, Kim BJ, Kim MN (2016) Tightening effects of high-intensity focused ultrasound on body skin and subdermal tissue: a pilot study. J Eur Acad Dermatol Venereol 30: 1599-1602.
- Bay EY (2023) Topal IO. Aging skin and anti-aging strategies. Explor Res Hypothesis Med 8: 269-279.
- Csekes E, Račková L (2021) Skin aging, cellular senescence and natural polyphenols. Int J Mol Sci 22: 12641.
- Griffiths TW, Watson REB, Langton AK (2023) Skin ageing and topical rejuvenation strategies. Br J Dermatol 189: i17-i23.
- Fisher SM, Borab Z, Weir D, Rohrich RJ (2024) The emerging role of biostimulators as an adjunct in facial rejuvenation: a systematic review. J Plast Reconstr Aesthet Surg 92: 118-129.
- Jaiswal S, Jawade S (2024) Microneedling in dermatology: a comprehensive review of applications, techniques, and outcomes. Cureus 16: e70033.
- Yong TL, Tan KW, Ng CH (2025) Ceramides and skin health: new insights. Exp Dermatol 34: e70042.
- Natarelli N, Gahoonia N, Sivamani RK (2023) Bacteriophages and the microbiome in dermatology: the role of the phageome and a potential therapeutic strategy. Int J Mol Sci 24: 2695.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.