A Rare Case of Superior Mediastinal Cyst in Pregnancy with Spontaneous Postpartum Disappearance.
by Muhammad Mohsin Zahoor*, Hira Gul, Abdul Mannan, Brain Casserly, Abdul Rehman, Abdul Raziq
Respiratory Department, University Hospital Limerick, Limerick, Ireland
*Corresponding author: Muhammad Mohsin Zahoor, Respiratory Department, University Hospital Limerick, Ireland
Received Date: 03 August 2025
Accepted Date: 07 August 2025
Published Date: 11 August 2025
Citation: Zahoor MM, Gul H, Mannan A, Casserly B, Rehman A, et al. (2025). A Rare Case of Superior Mediastinal Cyst in Pregnancy with Spontaneous Postpartum Disappearance. Ann Case Report. 10: 2367. https://doi.org/10.29011/2574-7754.102367
Abstract
Bronchogenic cysts are congenital anomalies arising from abnormal budding of the tracheobronchial tree, typically requiring surgical intervention when symptomatic. We present an unusual case of a 29-year-old pregnant woman who presented with acute chest pain and shortness of breath, initially raising concern for pulmonary embolism. Computed tomography pulmonary angiography (CTPA) revealed a 5 cm bronchogenic cyst located posterior to the trachea, with no evidence of pulmonary embolism. The patient was managed conservatively with antibiotics and discharged with close monitoring. Remarkably, follow-up imaging after delivery demonstrated near-complete resolution of the cyst, which had decreased to 1 cm without any medical or surgical intervention. This case highlights the potential for spontaneous regression of bronchogenic cysts, possibly influenced by the physiological changes of pregnancy, and challenges the conventional approach of mandatory surgical excision for such lesions.
Keywords: Bronchogenic cyst in pregnancy, mediastinal mass, spontaneous regression, cystic lesion
Introduction
Mediastinal masses represent a diverse group of lesions that may arise from congenital anomalies, neoplastic processes, or inflammatory conditions. Their discovery during pregnancy poses unique diagnostic and therapeutic challenges, particularly when they are asymptomatic and incidentally identified. The mediastinum is anatomically divided into anterior, middle, and posterior compartments, each with distinct differential diagnoses. Cystic lesions in the superior mediastinum are relatively rare and may include bronchogenic cysts, oesophageal duplication cysts, thymic cysts, lymphangia’s, and foregut duplication cysts [1]. The physiological changes of pregnancy, including alterations in immune function, hormonal milieu, and lymphatic flow, may influence the behaviour of certain mediastinal lesions. However, data on the natural history of mediastinal cystic masses during pregnancy are sparse. Most literature focuses on symptomatic masses requiring intervention, while asymptomatic lesions are often underreported. This case report adds to the limited body of evidence by documenting a large cystic mass that regressed spontaneously postpartum, emphasizing the value of conservative management and close follow-up.
Case Presentation
A 29-year-old at 32 weeks of gestation presented to the emergency department with acute-onset chest pain and dyspnoea. She denied fever, cough, haemoptysis, or palpitations. Laboratory investigations revealed mildly elevated inflammatory markers, and cardiac troponins were negative. Given her pregnancy and clinical presentation, pulmonary embolism was initially suspected. A CTPA was performed, the scan was negative for embolic disease but revealed an incidental cystic lesion in the superior mediastinum, measuring approximately 5 cm. The lesion was located posterior to the trachea and displaced the oesophagus anteriorly. No signs of compression or invasion of adjacent structures were noted Figure 1.

Figure 1: Coronal section of CT thorax showing smooth lines bronchogenic cyst in the mediastinum.
Given the absence of symptoms attributable to the mass and the patient’s stable condition, a multidisciplinary team including obstetrics, radiology, and thoracic surgery opted for conservative management. The patient was discharged with instructions for postpartum imaging follow-up. A repeat CT scan performed six weeks after delivery demonstrated a dramatic reduction in the size of the lesion, now measuring only 1 cm (Figure 2).
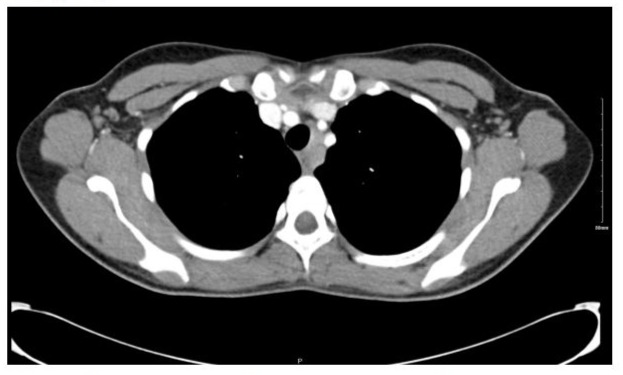
Figure 2: Coronal section of CT thorax showing interval regression of mediastinal bronchogenic cyst.
The patient remained asymptomatic throughout the course of observation.
Discussion
Bronchogenic cysts are congenital abnormalities and maybe missed initially on the chest radiography but are visible as smooth lined cysts with low density contents on the computed tomography, which differentiates them from the mediastinal lymph nodes. This case illustrates the natural history for bronchogenic cysts and a rare phenomenon of spontaneous regression of a superior mediastinal cystic mass discovered during pregnancy. The differential diagnosis for such lesions includes bronchogenic cysts, oesophageal duplication cysts, thymic cysts, and lymphatic malformations such as cystic hygromas. Imaging characteristics such as location, fluid content, and displacement of adjacent structures can guide diagnosis, but definitive classification often requires histopathological confirmation [1].
Bronchogenic cysts and foregut duplication cysts may remain asymptomatic and undetected until adulthood [2]. Lymphatic malformations, including cystic hygromas, are more commonly diagnosed in paediatric populations but can occasionally present in adults [3]. These lesions may fluctuate in size due to hormonal or immunologic factors, particularly during pregnancy [4]. The acute chest pain and shortness of breath in this case may have resulted due to expansion of the cyst, and the spontaneous regression post-partum raises intriguing questions about the influence of pregnancy-related physiological changes. It is plausible that hormonal shifts postpartum contributed to the involution of the cystic lesion [5]. Similar regression has been documented in foetal mediastinal masses, including rhabdomyomas and teratomas, although such reports are exceedingly rare in adults [6]. From a clinical management perspective, this case supports a conservative approach for asymptomatic mediastinal cystic lesions discovered during pregnancy. The risks associated with surgical intervention, anaesthesia, and foetal compromise must be weighed against the potential for spontaneous resolution [7]. The American College of Radiology (ACR) guidelines on incidental mediastinal findings recommend observation for benign-appearing cystic lesions without concerning features [8]. Additionally, Up-to-date provides a structured approach to evaluating mediastinal masses in adults, emphasizing the importance of location and imaging features in guiding management [9]. Cardiac MRI and echocardiography have also been shown to be useful adjuncts in evaluating mediastinal masses during pregnancy, especially when CT is contraindicated or inconclusive [10].
Conclusion
This case highlights an unusual but clinically important instance of spontaneous regression of a bronchogenic cyst following pregnancy. While surgical resection remains the mainstay of treatment for symptomatic cases, our findings suggest that conservative management may be appropriate in select patients, particularly when pregnancy-related physiological changes could influence cyst behaviour. Moreover, it raises important questions about the influence of pregnancy-related hormonal and immunologic shifts on the behaviour of cystic lesions an area that remains underexplored in adult thoracic pathology. By documenting this outcome, we contribute to the limited literature on mediastinal mass dynamics in pregnancy and highlight the value of postnatal follow-up in guiding management. This case serves as a reminder that incidental findings, when approached thoughtfully, can be navigated safely without compromising maternal or fetal outcomes. Further research is needed to explain the mechanisms underlying this phenomenon and to identify predictors of spontaneous regression. Clinicians should be aware of this possibility when managing bronchogenic cysts in pregnant patients or those with high surgical risk. Its publication is warranted to enhance awareness, support evidence-based practice, and encourage further research into the natural history of mediastinal cystic lesions in reproductive-age women.
References
- Jeung MY, Gasser B, Gangi A, Bogorin A, Charneau D, et al. (2002). Imaging of cystic masses of the mediastinum. Radiographics. 22: S79-S93.
- Amini B, Weerakkody Y, Bell D. (2025). Cystic mediastinal masses. Radiopaedia. Retrived in Online.
- Alawaysheh F, Aqrabawi HE, Alali A, Almhairat A, Alsawalgeh G. (2024). Neonatal mediastinal cystic hygroma: Case report. International Journal of Science and Research (IJSR), 13: 1188-1191.
- Gupta R, Munoz JC, Garg P. (2007). Mediastinal pancreatic pseudocyst - a case report and review of the literature. MedGenMed, 9: 8.
- Fesslova VME, Poziello C, Evangelista M, Cavoretto PI, Mellone R, et al. (2025). Atypical mediastinal mass in the fetus: A review of the literature. Archives of Gynecology and Obstetrics, 311: 203-212.
- The Fetal Medicine Foundation. (2025). Mediastinal tumor. The Fetal Medicine Foundation. Retrived in Online.
- Novoa G, Rotolo A, Montalto S. (2011). Large mediastinal mass in pregnancy: Utility of echocardiography and cardiac MRI. Journal of Medical Cases, 2: 13-14.
- Munden RF, Carter BW, Chiles C. (2018). Managing incidental findings on thoracic CT: Mediastinal and cardiovascular findings. Journal of the American College of Radiology, 15: 1087-1096.
- Berry MF, Bograd AJ, Muller NL. (2024). Approach to the adult patient with a mediastinal mass. UpToDate.
- Bhalla S, Hazewinkel M, Smithuis R. (2025). Mediastinal masses - differential diagnosis. Radiology Assistant. Retrived in Online.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.