A Giant Epidermoid Cyst
by Anmol Singh Randhawa*, Shiteez Agrawal, Swarjith Nimmakayala, Anurag Srivastava, Bhawani Shanker Sharma, Pankaj Gupta
Department of Neurosurgery, Mahatma Gandhi University of Sciences and Technology, Jaipur, India
*Corresponding author: Anmol Singh Randhawa, Department of Neurosurgery, Mahatma Gandhi University of Sciences and Technology, Jaipur, India
Received Date: 01 May 2025
Accepted Date: 31 May 2025
Published Date: 04 June 2025
Citation: Randhawa AS, Agrawal S, Nimmakayala S, Srivastava A, Sharma BS, Gupta P (2025) A Giant Epidermoid Cyst. Arch Surg 5: 128 https://doi.org/10.29011/3066-2559.000128
Introduction
Epidermoid cysts are usually painless and slowly grow as domeshaped skin lesions that may have varying textures - from firm to fluctuant. These cysts are commonly found on the neck, trunk, face, scalp, and scrotum. They typically arise when pilosebaceous follicles rupture due to an obstruction of the sebaceous gland opening, leading to a surface comedo or punctum.[1] These conventional epidermoid cysts have an epithelial wall and can range in size from a few millimeters to five centimeters in diameter. Although rare, giant epidermoid cysts with a diameter of 5 cm or more have been reported.[2] In this case, we report a giant epidermoid cyst over the scalp in an elderly woman, which was successfully removed.
Case Report
An elderly woman, aged 72,was admitted to the neurosurgical ward with a complaint of a large swelling on her scalp that had been present for 50 years. She first noticed the swelling when she was 22 years old, and it was initially about 5 x 5 cm in size. However, it kept growing slowly, and over the last five years,it started increasing more rapidly towards the left side. The swelling also became ulcerated at the apex. The patient had also been experiencing neck pain for the last year, which radiated to her left shoulder, especially when standing. She also complained of a deformity in her neck that caused an abnormal forward bend. The swelling was so large that the patient was unable to sleep or lie down in a supine position. However, she had no associated complaints of fever, weight loss, or any other lumps in her body (Figure 1).

Figure 1: Clinical preoperative photograph showing a giant epidermoid cyst of the scalp.
During the inspection, a swelling in the bilateral parieto-occipital region of the scalp was observed. The swelling measured 26x24x12 cm and had a globular shape with a lobulated surface. It had clearly defined edges,was soft, painless, non-tender, cystic, and showed no signs of infection. There was no evidence of expansile or pulsatile pulsations, and no impulse was observed on coughing. The overlying skin had normal color with venous engorgement, but there were no signs of redness or edema. Additionally, there was ulceration on the apex of the swelling. The transillumination test was negative.thin walled, cystic fluid collection of size 26 x 24 x 12 cm seen arising from deep scalp layers of left parieto-occipital region, extending from midline posterior high parietal region up to posterior aspect of occipital bone abutting their outer cortices and with normal underlying bone with no intra-cranial extension of the lesion (Figure 2).
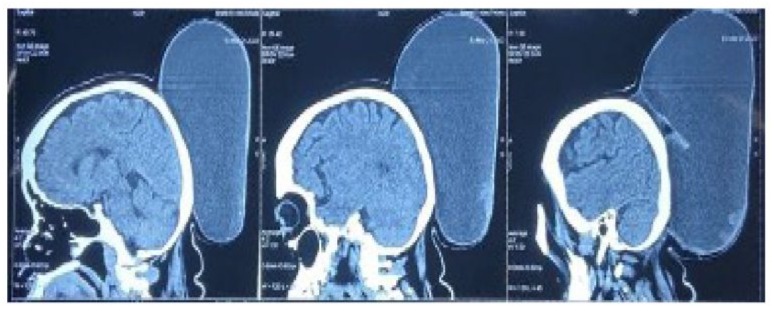
Figure 2 : Preoperative NCCT Head-Saggital cuts.
The patient was diagnosed with a large epidermoid cyst based on the findings. Lipoma and dermoid cyst were also considered as potential differential diagnoses. A preoperative Non-Contrast-CT scan of the skull was done to check for any bony or intracranial involvement. The scan revealed a large multiloculated, thin-walled, cystic fluid collection measuring 26 x 24 x 12 cm. The cyst was found in the deep scalp layers of the left parieto-occipital region and extended from the midline posterior high parietal region up to the posterior aspect of the occipital bone, abutting their outer cortices, with normal underlying bone with no intracranial extension of the lesion.On preoperative Magnetic Resonance Imaging (MRI), a large cystic lesion was detected in the scalp region between the parietal and occipital lobes. The lesion was well-defined, had multiple compartments, and measured around 26 cm × 24 cm × 12 cm. The cystic lesion did not affect the skull or brain. On T2-weighted images, the lesion appeared homogeneous with a high-intensity signal (Figure 3).
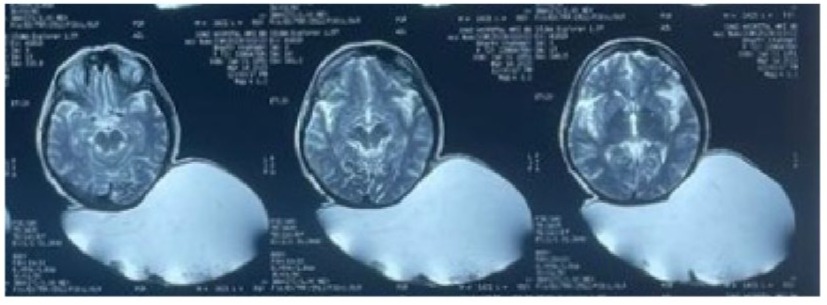
Figure 3 : T2 WI-Magnetic resonance image-Axial cuts.
Complete en mass excision of the lesion was carried out by an elliptical incision under general anesthesia and the wound was closed in layers, after adjustment of the flaps. An elliptical incision with a vertical extension lines was designed with consideration of redundant skin, and the dissection was extended from the subcutaneous layer to the subgaleal plane to expose the mass. Neovascularization was detected in the vicinity of the growth. Upon confirming that the mass was encapsulated, it was entirely removed. The mass had a weight of 3000 grams. Additionally, we excised the excess skin that had stretched to accommodate the mass and conducted primary closure. The wound healed without any problems or complications.The gross appearance of the mass showed that it had an outer membranous capsule with inner yellow and brown debris, and cut surface showing greyish white areas (Figure 4).
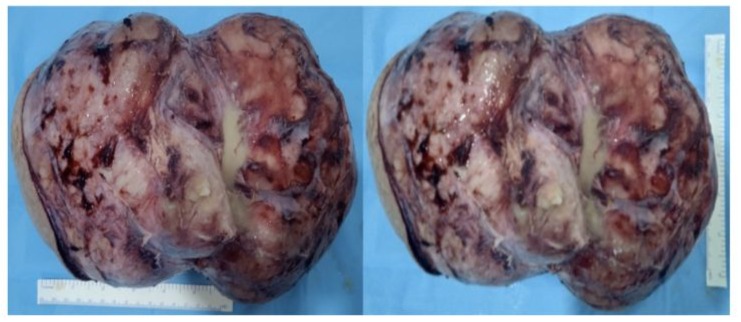
Figure 4 : Gross total excision of mass
The cystic lumen was filled with pultaceous fluid and showed degenerated and necrotic keratinaceous debris on histologic findings (Figure 5).
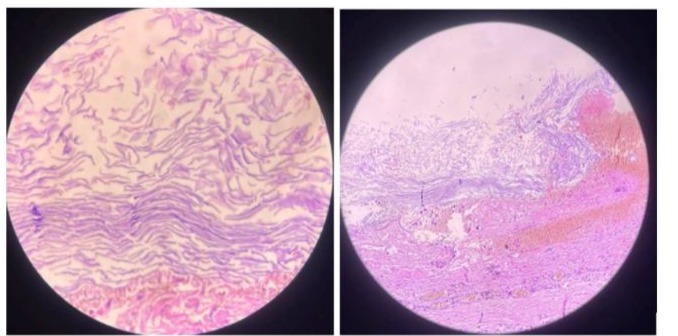
.Figure 5 : Histologic findings. There is an outer membranous capsule with inner degenerated and necrotic keratinaceous debris.
The postoperative period was uneventful and an excellent scar was noticed on follow-up (Figure. 6).
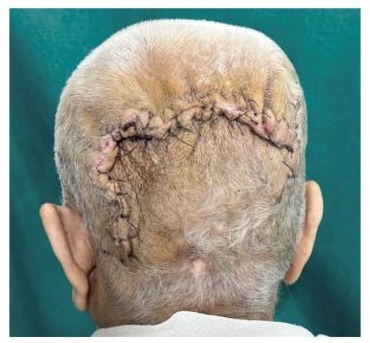
Figure 6 : Clinical photograph showing an excellent scar at two week follow- up
The patient was satisfied with the aesthetic results of the operation. Pathological examination of the specimen revealed that it was an epidermoid cyst.The patient had an uneventful postoperative period with excellent aesthetic results and an epidermoid cyst was discovered during pathological examination of the specimen.
Discussion
The term “sebaceous cyst” is now less commonly used. More contemporary alternatives include “epidermoid cyst,” “epithelial cyst,” or “keratin cyst.”[3] Epidermoid cysts are rare, benign cysts that grow slowly.[2] They are lined with an epithelium that looks like the infundibulum of the hair follicle and has the same cytokeratin profile.[4]These cysts occur when a pilosebaceous follicle ruptures, often in association with acne, and are most commonly found on the face and scalp. Epidermoid cysts have a thin capsule of stratified squamous epithelium filled with keratin, cellular debris, and lipids, but they do not contain hairs or other dermal elements [5] that differentiate them from dermoid cysts. These cysts grow slowly, similar to normal skin. Usually, these cysts show up as uncomplicated skin lesions, but in some cases, they can become more complex. Multiple cysts in combination with multiple fibromas and osteomas could indicate Gardner’s syndrome.[3] There are different types of epidermoid cysts, and one of them is the intracranial epidermoid cyst. This type is rare, and it is believed to arise from the sequestration of ectodermal remnants within the cranial bones [6]. When this type of cysts appears, it usually presents as a swelling over the scalp or as a well-circumscribed intracranial lesion. There are several surgical approaches to treat epidermoid cysts. Complete surgical excision is the most effective method, as it ensures complete removal and prevents recurrence. However, this technique can be timeconsuming and requires suturing the wound. An alternative technique is the minimal excision technique, which is less invasive and has been proven successful [7]. This technique involves making a small two-millimeter incision. A firm digital pressure is necessary to expel the cyst contents and separate the cyst wall from the neighboring tissues, making it easier for extraction. The small incision can then be closed with a single suture or left to heal naturally. Another variation of this technique is using a punch biopsy instrument to create the opening into the cyst [8]. An elderly female patient had a large cystic swelling on her scalp for the last 50 years, measuring 26 x 24 x 12 cm. This is the largest reported case of an epidermoid cyst, with the previous largest size being 20 cm × 15 cm × 10 cm.[9] The histopathology report of the specimen confirmed it as an epidermoid cyst. In conclusion, epidermoid cysts are typically benign skin growths, but there have been rare cases involving unusually large size, atypical locations, unusual complications, or rapid growth. These cases emphasize the potential complexities and variations that can occur with epidermoid cysts. Accurate diagnosis, evaluation, and treatment by professionals are important in managing such rare cases to ensure the best possible outcome for the patients
References
- Lookingbill DP, Marks JG (2000) Principles of Dermatology. 3rd ed. Philadelphia, PA: WB SaundersCompany 120-125.
- Baek SO, Kim SW, Jung SN (2011) Giant epidermal inclusion facial cyst. J Craniofac Surg 22:1149-1151.
- Zuber TJ(2002) Minimal excision technique for epidermoid (sebaceous) cysts. Am Fam Physician 65: 1409-1412.
- Kalgutkar A, Kini S, Jambhekar N, Das S (2006) Intradiploic primary epithelial inclusion cyst of the skull. Ann Diagn Pathol 10: 20-23.
- Boffano P, Roccia F, Campisi P, Zavattero E, Gallesio C, Bosco GF (2011) Epidermoid cyst of the temporal region. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 112 (6):e113-116.
- Diven DG, Dozier SE, Meyer DJ, Smith EB (1998)Bacteriology of inflamed and uninflamed epidermal inclusion cysts. Arch Dermatol 134: 49-51.
- Im JT, Park BY(2013) Giant epidermal cyst on posterior scalp. Archives of Plastic Surgery 40(03):280-282.
- Mehrabi D, Leonhardt JM, Brodell RT(2002) Removal of keratinous and pilar cysts with the punch incision technique: analysis of surgical outcomes. Dermatol Surg 28:673-677.
- Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, Mc- Michael AJ, et al (2019)Fitzpatrick’s dermatology. New York: Mc- Graw-Hill Education.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.