A Case of Internal Hernia and Pouch Volvulus in a Pregnant Woman (13th Week of Gestation) with a History of IPAA Treated Surgically
by Luisa Moretti*
Department of Medicine, University of Udine, Udine, Italy
*Corresponding author: Luisa Moretti, Department of Medicine, University of Udine, Udine, Italy
Received Date: 27 September 2025
Accepted Date: 07 October 2025
Published Date: 01 October 2025
Citation: Moretti L. (2025). A Case of Internal Hernia and Pouch Volvulus in a Pregnant Woman (13th Week of Gestation) with a History of IPAA Treated Surgically. 10: 2425. https://doi.org/10.29011/2574-7754.102425
Abstract
Introduction: Ileal pouch anal anastomosis (IPAA) following total proctocolectomy is a routine surgery for medically refractory ulcerative colitis (UC) or familial adenomatous polyposis (FAP). Volvulus of the ileal pouch as a complication of IPAA is extremely rare. We presented a case of internal hernia and volvulus of a J-type ileal pouch in a pregnant woman.
Presentation of case: A 36 years-old pregnant woman (13th week of gestation), with history of total proctocolectomy with IPAA for severe UC in 2022 and endoscopic decompressions for pouch volvulus, presented with signs of bowel obstruction. Pouchscopy showed twisting of the pouch with ischemic mucosal distress. During emergency surgery internal hernia of small-intestine loops under the superior mesenteric artery axis was found and reduced. This caused the rotation of the pouch. Closure of the passage between the mesentery and the retroperitoneum followed by a proximal diversion ileostomy were performed.
Discussion: Although IPAA significantly improves patients’ quality of life, it carries a wide spectrum of complications, including volvulus of the ileal pouch. This is an extremely rare condition, particularly in pregnant women. In general, the type of treatment depends on the viability of the pouch. In pregnancy, the lack of literature on this pathology makes it impossible to identify a gold standard for the treatment.
Conclusion: Early diagnosis and treatment of ileal pouch volvulus and internal hernia is necessary to prevent the development of local ischaemia. In pregnant women, if the pouch is viable, endoscopic derotation can be performed as a conservative treatment but it is associated with an increased risk of recurrence. If associated with internal hernia, closure of the passage between the mesentery and the retroperitoneum and pouchpexy are valid treatments to avoid recurrence allowing pouch preservation. If pouch gangrene is present, it is indicated to redo the pouch anastomosis with preferable proximal diversion ileostomy.
Introduction
Ileal pouch anal anastomosis (IPAA) after total proctocolectomy, first described by Parks AG et al., in the early 1980s, is now the surgical procedure of choice in ulcerative colitis and familial adenomatous polyposis (FAP). [1] The incidence of ulcerative colitis disease among women is 10.4 per 100,000. The peak of the disease is between 15- and 25-years old, and about a quarter of women will conceive after diagnosis. [2] In cases refractory to medical therapy, women of childbearing age with inflammatory bowel disease may require surgical treatment with proctocolectomy and IPAA. These procedures provides the benefit of enhance continence by maintaining anal sphincter function thus decreasing stool frequency. This significantly improves patients’ health-related quality of life. [3] Complications of IPAA are varied, including occlusion due to twisted pouch syndrome, pouch volvulus or by adhesions, which traditionally require surgical intervention. [4, 5] Pouch volvulus is distinct from twisted pouch syndrome. In the first case a properly constructed pouch develops an acute volvulus around the axis of the superior mesenteric axis (SMA) and is related to a lack of adhesions in the pelvis. [6] If left untreated, the volvulus can disrupt vascularization, leading to pouch ischemia and necrosis. Treatment usually involves emergency endoscopy to untwist the pouch or surgical approaches of pouchpexy or redo pouch-surgery to prevent future episodes [7].
Here we report a case of pregnant woman with history of proctocolectomy and IPAA for ulcerative proctitis, complicated by a surgically treated pouch volvulus and internal hernia, so that others may benefit from our experience. To our knowledge, no such case has ever been reported.
Case Report
A 36-years old pregnant woman with a BMI of 17 and no comorbidities presented at our Hospital Emergency Department with abdominal pain and costipation. She was diagnosed 10 years earlier with ulcerative proctitis (UP). She reported history of flares and ostomy complications in association with her three previous gestations periods. Two years after UP diagnosis, during her first pregnancy, she experienced a severe flare requiring intravenous steroids, followed by rescue therapy with infliximab with a subsequent clinical, biochemical, and endoscopic (Mayo 1 colitis in sigmoidoscopy) response. Despite maintenance with infliximab, the following year she underwent total colectomy and ileostomy because of toxic megacolon. Histological examination confirmed the presence of ulcerative proctocolitis in active phase without dysplasia. Two years later, while in her 16th week of the second pregnancy, she was admitted for acute obstructive symptoms. An abdominal ultrasound revealed a small bowel angulation just few centimeters from the skin margin, likely caused by post-surgical adhesions and potentially enhanced by the mass effect of the gravid uterus. A trans-stomal endoscopic decompression was performed and, after assessement of the normal course of the pregnancy, the patient was discharged with a scheduled follow-up. The patient required 7 additional endoscopic decompressions and temporary placement of a drainage tube at increasingly shorter intervals. At 37 week she underwent elective cesarean section (CS) and gave birth to a healthy baby. Three years later a proctectomy and ileal pouch-anal anastomosis (IPAA) were performed. She was then submitted to ileostomy’s closure 7 months later. Her postoperative course was regular, with a normal functionality of the pouch. Later that same year, she presented to the emergency department complaining of abdominal pain and closed bowel. The patient was four week pregnant. A pouchscopy showed a twisting of the pouch bowel around its mesenteric axis; an endoscopic derotation was then performed, which allowed liquid stools and gas drainage. A wire-guided rubber drainage tube was placed to overcome the twisted segment and was held in place for 6 hours. After having carefully monitored the foetus, the patient was discharged home. She was submitted to 7 further endoscopic decompressions in two months. At this point she presented to the Emergency Department for a new episode of pouch twisting. This time lower endoscopy showed a complete spiral of the J-pouch with ischemic mucosal distress (Figure 1). Laboratory examinations were normal. After a collegial discussion of the case, considering the risk of perforation if the conservative approach was continued in a patient 13 weeks pregnant, it was decided to take the patient to the operating room. An explorative laparoscopy showed diffuse distention of the small intestine. The pouch was twisted on mesenteric axis and displaced in the right inferior quadrant by the uterus and by some loops of small intestine that were dislocated under the mesenteric axis as an internal hernia (Figures 2, 3). Not surprisingly there were no adhesions, either in the pelvis or in the abdomen, which made the pouch completely mobile. After conversion to open surgery, the internal hernia was manually reduced. Then closure of the passage between the mesentery and the retroperitoneum with interrupted non-absorbable suture and fibrin glue followed by a proximal diversion ileostomy were performed. An intraoperative pouchscopy was performed and it showed the persistence of an ischemic distress area, although the mucosa was intact. The postoperative course was uneventful and eight days later the patient was discharged. The pregnancy continued normally. At one month - endoscopic control of the pouch a cuffitis was described and was locally treated with mesalazine. The follow-up ultrasound at 7 months was regular for the observation period and fetal growth was normal.

Figure 1: Endoscopic ischemic mucosal distress.

Figure 2: Small intestinal loops herniated under the mesenteric axis.
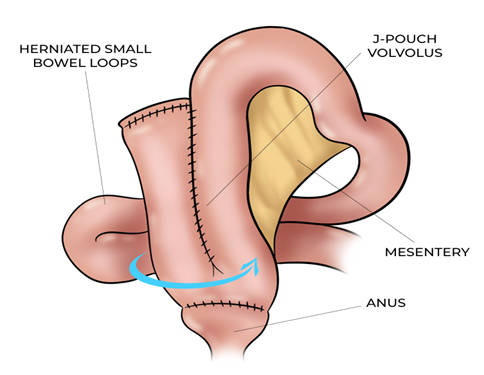
Figure 3: Representation of pouch volvulus and internal hernia.
Discussion
Total proctocolectomy with IPAA is associated with different postoperative complications, such as strictures (14%), small bowel obstruction (20%), fistulas (30%) and pouchitis (40-50%). [5, 8, 9] Obstruction secondary to volvulus of the proximal small bowel or ileal pouch is rare, but nonetheless important potential problem caused by rotation of the pouch around the axis of the SMA, that can cause interruption to the blood supply to the bowel resulting in venous congestion, obstruction, ischemia, and eventually necrosis. [10] It is more common in women as there is more space in the pelvis and perhaps more opportunity for the pouch to twist. Other risk factors for pouch mobility are low BMI and laparoscopic surgery. As explained in an article by Landish, in this type of surgical approach there are fewer adhesions that could fix the pouch and the visualization was sometimes not adequate, allowing technical error during the creation of the anastomosis. [11] This may result in having to place the mesentery posterior or to the left of the created pouch. [4] Our experience confirms what is reported in literature: our patient has the common risk factors listed above, such as female sex, low BMI, history of laparoscopic proctocolectomy and IPAA. During explorative laparoscopy we didn’t observe any adhesions that could fix the pouch, allowing its torsion and herniation of the bowel under the AMS axis. Stefan's et al. reported volvulus as a different entity from twisted pouch syndrome, which can be distinguished between outlet and inlet twist. The outlet twist is characterized by distal pouch twisted > 90° with partial occlusion of the lumen, due to an unrecognized twist of the distal pouch during construction of the anastomosis. The inlet twist instead shows as the entire pouch is rotated 360° and the mesentery of the pouch stand posteriorly. The etiology of this form involves passing the pouch down into the pelvis with a loop of the small bowel wrapped around the SMA somewhere between the pelvic inlet and the duodenum. This emphasize the importance of tracing the mesenteric cut edge from the duodenum to the pouch body [6]. On the other hand, in our case, the pouch was established in a non-twisted manner, but an internal hernia resulted in a pouch volvulus. Regarding this complication in pregnant women, data in literature are very limited. Pregnant women with IPAA are patients not common to encounter, due to the >20% reduction in fertility observed after IPAA, as reported in a survey by Bradford et al [12].
The reason for this is unclear, but may be partly due to pelvic adhesions, resulting in obstruction of the fallopian tubes or ovaries and may be lower in women undergoing a laparoscopic than open IPAA. [13] Furthermore, alterations in sexual function could be related to nerve plexuses injury or distortion of the pelvic anatomy. In dependency, dyspareunia increased after restorative proctocolectomy from 8 to 25 percent. [14-16] Compared to previous surgical procedures for inflammatory bowel disease, such as ileostomy or Kock pouch, women who become pregnant after IPAA experience fewer complications (29% and 53%, respectively, vs. 12.7%) as reported in Seligman’s review [2].
Approximately one third of subjects experienced disturbances of pouch function during the pregnancy, almost exclusively during the third trimester. [17] This contrasts with our experience, in which we found earlier occlusions during the second trimester of the second pregnancy and the first trimester of the third pregnancy. Mechanical intestinal occlusion has a variety of underlying aetiologies, including stricture disease, adhesions and pouch twists and may occur due to the space-occupying effect of the gravid uterus. [2] Diagnosis is often delayed because symptoms such as nausea, vomiting and abdominal distension can be confused with normal pregnancy [18]. In our reported case, however, the diagnosis was made early through pouchscopy, given the personal history of mechanical occlusion in the previous pregnancy. Modern diagnostic aids should now allow a more nuanced therapeutic approach, balancing timely care of the mother with the maturation needs of the foetus (it is estimated that each week over 30 weeks’ gestation saves 2 weeks of neonatal intensive care). [19] CT scan isn’t indicated because it exposes the foetus to ionizing radiation. MRE, IUS and pouchoscopy are safe in pregnancy and can complementarily define the cause of a mechanical complication. [20, 21] In general, there are different types of treatment depending on the severity of the ischaemia of the intestinal loops. After the assessment of the viability of the mucosa by pouchoscopy, endoscopic decompression and transanal catheter placement can be performed. This is a conservative method of resolving acute obstruction but is associated with a hight risk of recurrence. [22] It may be employed in isolation or as a bridge to definitive surgical intervention (i.e. pouch excision, bilateral pouchopexy, diversion or redo IPAA), with or without simultaneous delivery. [15] Also in our case, we first attempted a conservative approach with endoscopic decompression. The recurrence and the presence of localized superficial mucosal ischaemia led us to intervene surgically. During explorative laparoscopy we found an internal herniation of small intestine below the mesenteric axis that twisted the pouch. This wasn’t reducible laparoscopically, so we decided to convert it to open surgery. After hernia reduction, we assessed the viability of the intestine also by pouchscopy, so pouch resection was avoided. Then closure of the passage between the mesentery and retroperitoneum was performed to prevent recurrence and proximal diversion ileostomy was carried out. This is the first time that rotation of the pouch due to an internal hernia during pregnancy has been described. In general, the treatment of pouch volvulus varies depending on the viability of the pouch. As reported in a case report of Myrelid et al., since a prerequisite for the occurrence of volvulus is the absence of adhesions in the pelvis, if the pouch is viable after de-rotation and anastomotic site healthy, a pexy of the pouch must be done. [23] In contrast, the cases observed by Jain and Patel show that the presence of gangrene in the pouch or proximal intestine should justify redoing the pouch anastomosis with a preferable proximal diversion ileostomy. [3, 10, 24] As noted in literature, urgent surgical intervention is necessary in cases of severe gestational intestinal obstruction to avoid the maternal and fetal mortality and morbidity related to this condition. [19] Premature delivery could be a consequence of laparotomy during the third trimester or a way to obviate the need for surgery in case of small-bowel obstruction caused by the direct uterine compression of the pouch [18].
Conclusion
Volvulus of the ileal pouch in conjunction with internal hernia is a very rare occurrence following IPAA for ulcerative colitis in pregnant women. Early diagnosis and treatment are necessary to prevent the development of local ischaemia. We believed that also in pregnant women, if the pouch is viable, closure of the passage between the mesentery and the retroperitoneum and pouchpexy are valid treatment to avoid recurrence allowing pouch preservation.
Consent
A written informed consent was obtained from the patient.
Conflict of Interests
The authors declare that there is no conflict of interests.
References
- Parks AG, Nicholls RJ, P. Belliveau. (1980). “Proctocolectomy with ileal reservoir and anal anastomosis,” Br. J. Surg. 67: 533-538.
- Seligman NS, Sbar W, Berghella V. (2011). “Pouch function and gastrointestinal complications during pregnancy after ileal pouch-anal anastomosis,” J. Matern. Neonatal Med. 24: 525-530.
- G Tyagi. (2014). “Volvulus of ileal S-pouch: A rare complication of ileal pouch anal anastomoses,” Int. J. Surg. Case Rep. 5: 717-719.
- Pokala S, Shen B. (2022). “Endoscopic management of obstructing pouch twist,” Gastroenterol. Rep. 10.
- KS Ng, Gonsalves SJ, Sagar PM. (2019). “Ileal-anal pouches: A review of its history, indications, and complications” World J. Gastroenterol. 25: 4320-4342.
- SD Holubar. (2024) “Unraveling Twisted Pouch Syndrome: A Narrative Review of Classification, Diagnosis, Treatment, and Prevention,” Inflamm Bowel Dis. PP: 850-856.
- de Castelbajac F, Billet N, Monnier-Chollet L, Zaanan A, Seksik P, X Dray. (2025). “An ileo-anal pouch doing the twist (with video),” Clin. Res. Hepatol. Gastroenterol. 49: 102511.
- Buettner H, MX Kiely, M Yao, J Yoo, L Chen. (2018). “Unique surgical approach to a twisted ileal-anal pouch,” J. Surg. Case Reports, 2018: 1-3.
- Shannon A. (2016). “Long-term follow up of ileal pouch anal anastomosis in a large cohort of pediatric and young adult patients with ulcerative colitis” J. Pediatr. Surg. 51: 1181-1186.
- Patel S, G Salotera, S Gurjar, J Hewes, I Ahmed, B Andrews. (2008). “Ileo-anal pouch necrosis secondary to small bowel volvulus: A case report,” World J. Emerg. Surg. 3: 1-4.
- Landisch RM, PM Knechtges, MF Otterson, KA Ludwig, TJ Ridolfi. (2018). “Pouch volvulus in patients having undergone restorative proctocolectomy for ulcerative colitis: A case series,” Dis. Colon Rectum. 61: 713-718.
- Bradford K, GY Melmed, P Fleshner, M Dubinsky. (2012). “107 Significant Variation in Care for Women of Reproductive Age With Ulcerative Colitis,” Gastroenterology. 142: S-26.
- Campigotto M, A Braini, MM Casarotto, SL Crocè, R Sablich. (2022). “Childbearing and Delivery in Women With Ulcerative Colitis and Ileostomy or Ileal Pouch-Anal Anastomosis,” ACG Case Reports J. 9: e00805.
- Cornish JA. (2007) “The effect of restorative proctocolectomy on sexual function, urinary function, fertility, pregnancy and delivery: A systematic review,” Dis. Colon Rectum. 50: 1128-1138.
- Prentice RE. (2023). “Evaluation and management of ileal pouch-Anal anastamosis (IPAA) complications in pregnancy, and the impacts of an IPAA on fertility,” Eur. J. Gastroenterol. Hepatol. 35: 609-612.
- Sriranganathan D, Poo S, JP Segal. (2022). “The impact of the ileoanal pouch on female fertility in ulcerative colitis: A systematic review and meta-analysis,” Color. Dis. 24: 918-924.
- Ravid A. (2002). “Pregnancy, delivery, and pouch function after ileal pouch-anal anastomosis for ulcerative colitis,” Dis. Colon Rectum, 45: 1283-1288.
- Walker M, Sylvain J, Stern H. (1997). “Bowel obstruction in a pregnant patient with ileal pouch-anal anastomosis,” Can. J. Surg. 40: 471-473.
- Spring A, M Lee, S Patchett, J Deasy, I Wilson. (2012). “Ileostomy obstruction in the third trimester of pregnancy,” Color. Dis. 14: 631-632.
- Mahadevan U. (2019). “Inflammatory Bowel Disease in Pregnancy Clinical Care Pathway: A Report From the American Gastroenterological Association IBD Parenthood Project Working Group,” Gastroenterology, 156: 1508-1524.
- Shen B. (2024). “Endoscopic diagnosis and management of adult inflammatory bowel disease: a consensus document from the American Society for Gastrointestinal Endoscopy IBD Endoscopy Consensus Panel,” Gastrointest. Endosc., PP: 1-20.
- Warren C, ME O’Donnell, KR Gardiner, T Irwin. (2011). “Successful management of ileo-anal pouch volvulus,” Color. Dis. 13: 106-107.
- Myrelid P, Druvefors P, Andersson P. (2014). “Recurrent Volvulus of an Ileal Pouch Requiring Repeat Pouchopexy: A Lesson Learnt,” Case Rep. Surg. 2014: 1-3.
- Jain A, MA Abbas, HK Sekhon, JA Rayhanabad. (2010). “Volvulus of an ileal J-pouch,” Inflamm. Bowel Dis. vol. 16: 3-4.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.