70 Cases of Incomplete Pancreatic Divisum (IPD)-The Usefulness of MRCP Diagnosis and the Safety of Endoscopic Treatments via Duodenal Major and Minor Papilla
by Tadao Tsuji1*, G Sun1, T Shinobi1, K Ohishi1, Y Moriya1, H Kaihara1, S Yamamoto1, K Aoto1, Y Naritomi1, M Ono1, T Masuda1, H Shinozaki2, H Kaneda2, H Katsura2, T Mizutani2, K Miura2, M Katoh2, K Yamafuji3, K Takeshima3, N Okamoto3, S Nyuhzuki4
1Saitama Cooperative Hospital, Gastroenterology, Japan
2Saitama City Hospital, Gastroenterology, Japan
3Saitama City Hospital, Surgery, Japan
4Kaetsu Hospital, Gastroenterology, Japan
*Corresponding author: Tadao Tsuji, Saitama Cooperative Hospital, Gastroenterology, Japan 1317 Kizoro, Kawaguchi-shi, Saitama, 333-0831 Japan E-mail:t-tsuji@mcp-saitama.or.jp
Received Date: 02 September 2024
Accepted Date: 05 September 2024
Published Date: 09 September 2024
Citation: Tsuji T, Sun G, Shinobi T, Ohishi K, Moriya Y, et al (2024) 70 Cases of Incomplete Pancreatic Divisum (IPD)-The Usefulness of MRCP Diagnosis and the Safety of Endoscopic Treatments via Duodenal Major and Minor Papilla. Ann Case Report. 9: 1967. https://doi.org/10.29011/2574-7754.101967
Abstract
Incomplete Pancreatic Divisum (IPD) is a rare congenital disease caused by maljunction between the ventral duct and the dorsal duct in the 7th week in embryonic stage. In our hospital over the past 10 years, 70 cases of IPD were diagnosed. This is 3.7% (70/1915) of naïve ERP cases during this period (2014.9.~2024.3.). Many classifications were proposed in the literature. We classified them by “modified Hirooka’s classification” into stenotic fusion type 1, 2 (sf 1 7 cases, sf 2 1 case), ansa pancreatica type (0 case) and branch fusion type 1, 2, 3 (bf 1 17 cases, bf 2 0 case, bf 3 44 cases). MRCP was performed in 57 cases, and 20 cases (20/57=35%) were diagnosed by MRCP alone. Finally 49 cases could be correctly diagnosed by MRCP (49/57=86%). Symptomatic cases were treated by endoscopy -13 cases, ESWL -1 case, and ESWL + endoscopy -39 cases. Asymptomatic 14 cases had no therapy.
About the Endoscopic treatment, via major papilla were performed in 19 cases with a technical success rate of 100%, while via minor papilla were performed in 34 cases with a technical success rate of 90% (28/34) without severe complications. In difficult cases, we performed our new endoscopic procedures; rendezvous precut (RP) method and reverse balloon dilation (RBD) method in 8 cases. 81%(43/53) of symptomatic patients had a history of alcohol intake, while 71% (12/17) of asymptomatic case had no alcohol intake. So alcohol intake may make IPD symptomatic.
After endoscopic treatments, the prognosis was good in 48, poor in 4 and 1 had an operation by pain relapse. In 50 calcified cases, ESWL and/or endoscopy were performed more repeatedly than 20 non-calcified cases .EPS is still placed in 39 cases (major14, minor 25) to maintain the pancreas juice flow and to prevent the papilla occlusion.
Key Words: Incomplete pancreatic divisum, MRCP, Endoscopy
Introduction
In the literature, papers about the diagnosis and the treatment of IPD are few, so we would like to report about MRCP diagnosis and endoscopic treatment in our hospital over the past 10 years. Our aim is to clarify the usefulness of MRCP diagnosis and the safety of endoscopic treatments via the duodenal major and minor papilla.
Methods
70 cases of IPD, experienced over the past 10 years, were enrolled. MRCP diagnoses, endoscopic treatments and their prognoses were evaluated. About the prognosis, good; without irregular pain relapse, controlled with every 2 years EPS replacement, poor; irregular pain relapse uncontrolled with every 2-year EPS replacement
Results
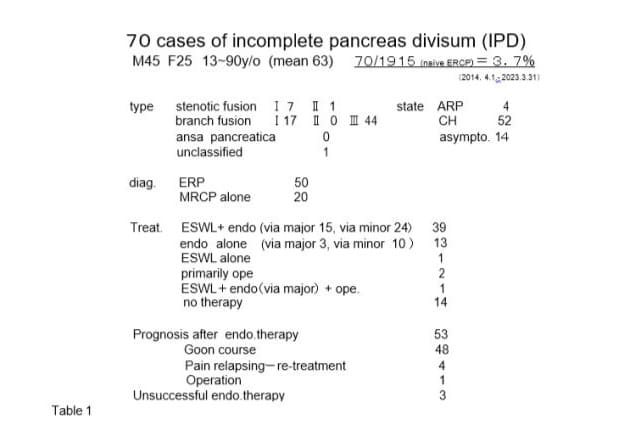
They consisted of 45 males and 25 females, aged 13-90 y/o (mean 63). It was 3.7% (70/1915) of naïve ERP cases in this period. The states of disease were 4 ARP (acute relapsing pancreatitis), 52 CH (chronic pancreatitis), and 14 asymptomatic phase (Table 1).
We classified them by “modified Hirooka’s classification” (Figure 1) into stenotic fusion type1,2, (sf1,sf2), branch fusion type 1,2,3,(bf1,2,3), and ansa pancreatica type. Each number was 7,1,17,0,44 and 0 respectively. One case was unclassified.
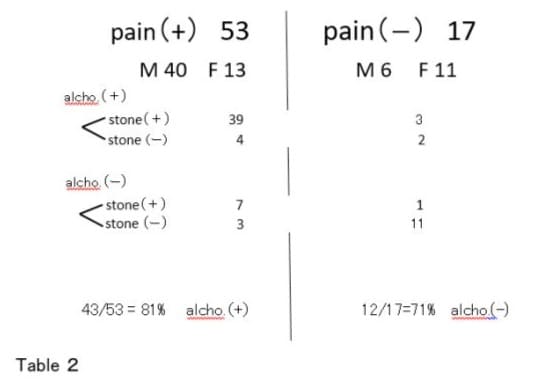
53 symptomatic cases consisted of 40 males and 13 females (alcoholic 81%). 6 severe pancreatitis cases with pseudocysts were all calcified alcoholic male cases. While 17 asymptomatic cases consisted of 6 males and 11 females (non-alcoholic 71%) (Table 2). 49 cases were diagnosed by ERP and MRCP, while 20 cases by MRCP alone. Treatment procedures consisted of 39 ESWL+endoscopy (via major papilla 15, via minor papilla 24), 13 endoscopy alone (via major 3, via minor 10), 1 ESWL alone,1 operation (tail pseudocyst) without medical treatment, and 1 pancreato-duodenectomy after medical treatment and 14 no therapy.
At the first endoscopic treatment, a pancreatic stent (5 or 7Fr. pig tail type) was placed, and 4 months later, it was replaced. Then every 2 years, ERP was performed and if necessary, the stent was replaced. The prognoses were good in 48 cases, however 4 calcified cases required treatments more repeatedly due to stone and pain relapse and a stent is still in place in 39 cases. There was 1 early complication case - duodenal wall perforation and peri- duodenal abscess formation (case E below), while there was no other complication cases such as bleeding, severe pancreatitis. One late complication- stent migration- was experienced. 1 case had an operation (pancreato-duodenectomy) after medical treatment. 3 cases were unsuccessful in endoscopic therapy. There were no cases of cancer occurrence or death after treatments.
Case presentation
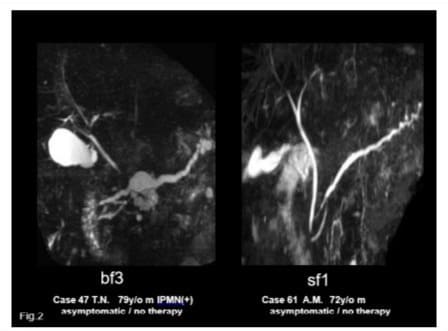
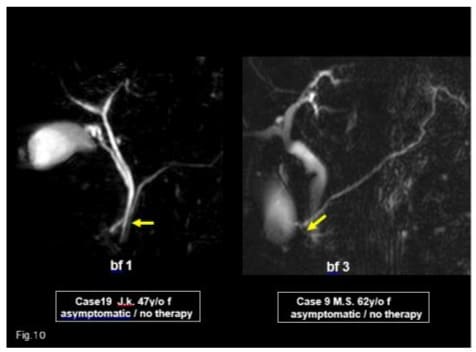
- 79 y/o m bf 3-ipmn(+) and 72 y/o m sf 1 – asymptomatic. diagnosed by MRCP alone (Figure 2).
- 30 y/o m bf 3: EPST of minor papilla, balloon dilation and EPS (Figure 3).
- Rendezvous pre-cut method: 56 y/o m bf 3: The guidewire, inserted through the major papilla, came out into the duodenum via the minor papilla. Along this guidewire, the minor papilla was cut by the needle type papillotome and the catheter was inserted into the minor papilla, then EPS was placed. This is our original procedure, a variant of the rendezvous method (Figure 4).
- Reverse Balloon Dilation Method: 13 y/o f bf 3: She entered into our hospital complaining of recurrent epigastralgia. The guidewire, inserted into the major papilla, came out via Wirsung’s duct, connecting branch, Santorini’s duct and minor papilla into the duodenum. The minor papilla was cut by needle type papillotome (rendezvous pre-cut method), then a balloon catheter was inserted along the guidewire and the minor papilla was dilated from the reverse direction by a 4mm dilation balloon, then EPS could be placed into the dorsal duct (Figures 5,6).
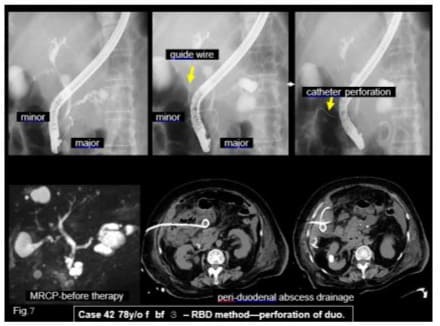
- Reverse Balloon Dilation Method: duodenal wall perfora-tion case 78 y/o f bf 3. When the catheter, proceeded into the duodenum lumen via the minor papilla under the guidewire, injury of the duodenal wall at the opposite side and made peri-duodenal abscess. Percutaneous drainage was performed, then cured. In this method, deep guidewire insertion into the duodenum via the minor papilla is necessary to prevent duodenal wall perforation by catheter (Figure 7).
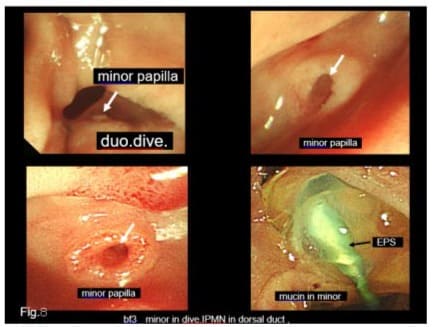
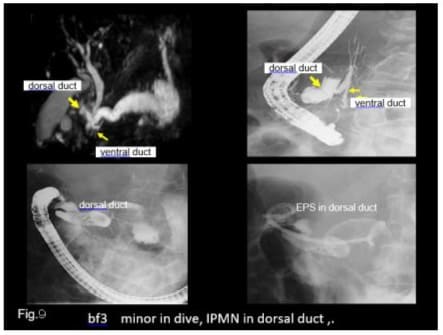
We had7cases combined with IPMN- One case was dorsal duct type IPMN. Minor papilla, located in the duodenal diverticulum, was the drainage route of mucin (Figures 8,9).
Two young females were treated - one was case D above, and the other was a 13 y/o (bf 3) combined with duodenal membranous occlusion.





Discussion
About the prevalence of IPD in the western countries, it is very low with a reported incidence of 0.13-0.9 % [1-5], on the other hands, it is much high in the recent reports from Japan and Korea [1,6].
We have no data of IPD prevalence in general Japanese population; however, 3.7% (70/1915) of naïve ERP cases were IPD in our hospital over the past 10 years. The mean age in our series was 64.6 y/o except the two young female. Kamisawa reported that the prevalence of IPD was 1.3% (41/3210) in their ERCP series and the mean age was relatively high [1,6].
In the literature, many types of IPD classification were suggested [7,8]. In this paper, we proposed a new type one -“modified Hirooka’s classification”. By this, we classified them into sf1,sf2, bf1,2,3,and ansa pancreatica type. 1 case could not be classified. In the near future, after many reports of IPD, another new useful classification will be proposed. In our reports, there is no bf 2 type, so we suppose some deviations in our diagnosis.
Recently usefulness of MRCP is reported in diagnosis of IPD [9,10]. In our series, MRCP was performed in 57 cases-49 cases (89%) could be diagnosed correctly, and 20 cases were diagnosed by MRCP alone (Figure 10). More IPD cases will be reported by MRCP diagnosis in the near future. We had no case of cancer occurrence. Kamisawa reported that the cancer occurrence rate was 9% (4/44)in complete and incomplete divisum, mainly in dorsal duct [6,11].
About the treatment, medical conservative therapies were recommended in early stages [12-15] of CPD (complete pancreatic divisum) and IPD. Formally in the symptomatic stage, surgical therapy was performed. In some reports, the therapeutic effects of surgery and endoscopy are almost equal, however, in other reports the effect of the former is superior to that of the latter [16]. In many reports, patients of ARP stage had better results than in CH stage after treatment [17].
Nowadays endoscopic procedures are the preferred choice for CPD and IPD therapy. Cotton reported minor papilla sphincterotomy in CPD [18], and Jacob reported minor papilla sphincterotomy in CPD [19]. Since then, many new techniques (wire-guided minor papilla sphincterotomy, pre-cut method, needle knife cut method, balloon dilation method) were developed and good results were reported by many authors [20-30]. New therapeutic procedures have been reported by Chavan; reverse sphincterotomy of the minor papilla, and by Artifon; reverse minor papilla balloon dilation without EPS [31,32]. From 2017, we have introduced and reported about the new therapeutic procedures for the CPD and IPD therapy: pre-cut method, balloon dilation method, freehand method, rendezvous method, rendezvous pre-cut method and reverse balloon dilation method. We reported therapeutic success rates of CPD and IPD via minor papilla was 97% (131/135) and 94% (33/36) respectively without severe complications [33-36]. However, we had to exchange EPS repeatedly and still now EPS is in place in 39 cases (major 14,minor 25). We suppose that the transient metalic stent may be useful in such cases.
Like other author’s opinion, we think that the congenital dysfunction of the minor papilla and some acquired factors (ie. alcohol intake, obesity) may make IPD symptomatic [11]. In this report, 81% of symptomatic cases had alcoholic intake histories, while 71% of asymptomatic cases had no such history [37,38].
Conclusions
In this paper, we proposed a new classification – “modified Hirooka’s classification” and reported the usefulness of MRCP diagnosis and the safety of endoscopic treatments. Our new endoscopic procedures-rendezvous pre-cut method and reverse balloon dilation method are safe and useful for IPD treatment. After ESWL and/or endoscopic treatment of IPD, the prognoses were good. Acquired factors (alcohol intake, obesity) may make IPD symptomatic.
References
- Bernard JP, Sahel J, Giovannini M, Sarles H (1990) Pancreas divisum is a probable cause of acute pancreatitis: a report of 137 cases. Pancreas. 5:248.
- Benage D, McHenry R, Hawes RH, et al. (1990) Minor papilla cannulation and dorsal ductgraphy in pancreas divisum. Gastrointes Endosc.36:553.
- Moreira VF, Merono E, Ledo L, Roman ALS, Erdozain JC, et al. (1991) Incomplete pancreas divisum. Gastrointes Endosc. 37:104.
- Ng JW, Wong MK, Huang J., Chan YT. (1992) Incomplete pancreas divisum associated with abnormal junction of pancreaticobiliary duct system. Gastrointes Endosc. 38:105.
- NO Machado. (2014) Pancreatic Divisum Beyond what is Obvious Pancreat Disord Ther. 4-139-2.
- Kamisawa T, Tu Y, Egawa N, Tsuruta K, Okamoto A, et al. (2006) Clinical Implications of Incomplete Pancreas Divisum J Pancreas7: 625-630.
- Kim MH, Lee SS, Kim CD, S K Lee, H J Kim, et al. (2001) Incomplete pancreas divisum:Is it merely a normal anatomic variant without clinical implications? Endoscopy 33: 778-785.
- Hirooka T, Kataoka S , Ohchi H , Takanori M, Toyonaga T, et al. (1994) Branch Fusion Between the Ventral and Dorsal Pancreatic Duct. Dig Endosc 6: 87-93.
- Fatih M, Akisik, K. Sandrasegaran, A.A. Aisen et al (2006) Dynamic Secretin–enhanced MR Cholangiopancreatography Radiographics. 26: 3.
- Mary A Turner, Ann S Fulcher, Jinxing Yu, et al (2013) Pancreatitis in patient with pancreas divisum:Imaging features at MRI and MRCP World J Gastroenterol, 19: 4907-4916.
- Takuma K, Kamisawa T, Tabata T, Egawa N, Igarashi Y, et al. (2010) Pancreatic Diseases Associated with Pancreas Divisum. Dig Surg 27: 144-148.
- Warshaw AL, Richter JM, Shapiro RH. (1983) The Cause and Treatment of Pancreatitis Associated with Pancreas Divisum. Ann. Surg 198: 443-450.
- Gregg JA (1977) Pancreas divisum: its association with pancreatitis. Am J Surg 134: 539-643.
- Blair AJ, Russel CG, Cotton PB (1984) Resection for pancreatitis in patients with pancreas divisum. Ann, Surg 200: 590-594.
- Russel RC, Wong NW, Cotton PB (1984) Accessory sphincterotomy (endoscopic and surgical) in patients with pancreas divisum. Br J Surg 71: 954-957.
- Hafezi M, Mayschak B, Probst P, Markus W Büchler, et al. (2017) A systematic review and quantitative analysis of different therapies for pancreas divisum -56 observational studies.Am J Surgery 214: 525537.
- Liao Z, Gao R, Wang W, Z Ye, XW Lai, et al. (2009) A systemic review on endoscopic detection rate, endotherapy, and surgery for pancreas divisum. Endoscopy. 41:439-444.
- Cotton PB (1978) Duodenoscopic papillotomy at the minor papilla of Vater for recurrent dorsal pancreatitis. Endosc Dig 3: 27-30.
- Jacob L, Geenen JE, Catalano MF, G Kenneth Johnson, Daniel J Geenen, et al. (1999) Clinical presentation and short-term outcome of endoscopic therapy of patients with symptomatic incomplete pancreas divisum. Gastrointest Endosc 49: 53-57.
- Kamisawa T (2004) Clinical Significance of the minor duodenal papilla and accessory pancreatic duct. Gastroenterol 39: 605-615.
- Testoni PA, Mariani A, Aabakken L, Marianna A, Erwan B, et al. (2016) Papillary cannulation and sphincterotomy technique at ERCP:European Society of Gastrointestinal Endoscopy Clinical Guidelines. Endoscopy 48: 657-693.
- Wilcox CM, Monkemuller KF (2001) Wire assisted minor papilla – precut papillotomy Gastrointest Endosc 54: 83-86.
- Lehman GA, Sherman S, Nisi R, R H Hawes (1993) Pancreas divisum;results of minor papilla sphincterotomy. Gastrointest. Endosc 39: 1-8.
- Heyries L, Barthet M, Delvast C, Christophe Z, Jean-Paul B (2002) Long term results of endoscopic management of pancreas divisum with recurrent acute pancreatitis. Gastrointest Endosc 55: 376-381.
- Soehendra N, Kempeneers I, Nam VC, Grimm H (1986) Endoscopic dilation and papillotomy of the accessory papilla and internal drainage in pancreas divisum. Endoscopy 18: 129-132.
- Yamamoto N, Isayama H, Sasahira N, Tsujino T, Nakai Y, et al. (2014) Endoscopic Minor Papilla Balloon Dilation for the Treatment of Symptomatic Pancreas Divisum. Pancreas 43: 927-930.
- Kamisawa T (2006) Endoscopic approach to the duodenal minor papilla; special emphasis on endoscopic management on pancreas divisum Dig.Endosc 18: 252-255.
- Lans JI, Geenen JE, Johanson JF, W J Hogan (1992) Endoscopic therapy in patient with pancreas divisum and acute pancreatitis; a prospective, randomized, controlled clinical trial. Gastrointest Endosc 38: 430-434.
- Gerke H, Byrne MF, Stiffler HL, Jorge V Obando, Robert M Mitchell, et al. (2004) Outcome of endoscopic minor papillotomy in patients with symptomatic pancreas divisum. JOP. 5: 122-131.
- Adutya G, Evan F, Stuart Sh (2013) Identification and Management of Pancreas Divisum Expert Rev Gastroenterol Hepatol.13: 1089-1105
- Chavan R, Kalapala R, Nabi Z, Sundeep L, D Nageshwar R(2017) Reverse sphincterotomy of the minor papilla via the major papilla for chronic pancreatitis with incomplete pancreas divisum. Endoscopy. 49: E119-E120.
- Artifon A, Mariana S, Frazao V, Flavio Coelho Ferreira (2012) A Novel Endoscopic Treatment of Pancreas Divisum Rev. Gastroenterol. PERU 32: 184-186.
- Tsuji T, Nyuhzuki S, Sun G et al. (2017) Usefulness and safety of endoscopic pancreatic duct balloon dilation (EPDBD) for treatment of pancreatic diseases-pancreatic stone,divisum and pseudocyst. Liver Pancreat Sci 2: 1-9.
- Tsuji T, Sun G, Sugiyama A, et al. (2019) Endoscopic treatment of pancreatic diseases via duodenal minor papilla : 135 cases treated by sphincterotomy, endoscopic pancreatic duct balloon dilation (EPDBD), and Pancreatic Stenting(EPS). Ann Clin Gastroenterol Hepatol 3: 012019.
- Tsuji T, Sun G, Sugiyama A, et al. (2020) Endoscopic Treatments of Pancreatic Incomplete Divisum in 20 cases–especially about our new procedures: Rendezvous Pre-cut method and Reverse Balloon Method. Gastro Med Res 4: 314-316.
- Tsuji T, Sun G, Sugiyama A. et al (2021) A Case Report -Endoscopic Treatments of 47 Incomplete Pancreatic Divisum (IPD) Cases in our Hospital- Special Emphasis on our New Procedures : Rendezvous Pre-cut method and Reverse Balloon Method. J Gast Hepa Rep 2:1-4.
- Tsuji T, Sun G, Shinobi T et al. (2023) Our New Endoscopic Treatments for Incomplete Pancreatic Divisum (IPD): Rendezvous Pre-cut method and Reverse Balloon Method. J Gastroenterol Hepatol Rep. 2:1-4.
- Tsuji T, Sun G, Sugiyama A, Amano Y, Mano S, et al. (2023) “62 Cases of Incomplete Pancreatic Divisum (IPD)–the Usefulness of MRCP Diagnosis and Safety of Endoscopic Treatments-Special Emphasis on our New Endoscopic Procedures-Rendezvous Pre-Cut Method and Reverse Balloon Dilation Method “ JOP . Journal of the Pancreas. 24.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.