Atypical Presentation of Epstein-Barr Virus Infectious Mononucleosis with Cholestatic Hepatitis and Hyperbilirubinemia in a Young Adult: A Case Report
by Chinmayi Pamala1,Sachdev Avinash2, Mohamed Orabi3, Ibrahim Kamel4*
1Tufts University School of Medicine, Boston, USA
2Internal Medicine, Steward Carney Hospital, Dorchester, USA
3Internal Medicine, Tufts Medical Center, Boston, USA
4Internal Medicine, Steward Carney Hospital, Boston, USA
*Corresponding author: Ibrahim Kamel, Internal Medicine, Steward Carney hospital, Boston, USA
Received Date: 10 September 2024
Accepted Date: 14 September 2024
Published Date: 17 September 2024
Citation: Pamala C, Avinash S, Orabi M, Kamel I (2024) Atypical Presentation of Epstein-Barr Virus Infectious Mononucleosis with Cholestatic Hepatitis and Hyperbilirubinemia in a Young Adult: A Case Report. Ann Case Report. 9: 1975. DOI: https://doi.org/10.29011/2574-7754.101975
Abstract
This case report details the presentation of a 24-year-old male of South Asian descent with an atypical manifestation of Epstein-Barr Virus (EBV) infectious mononucleosis, characterized by cholestatic hepatitis and hyperbilirubinemia. The patient initially presented with common symptoms of sore throat, intermittent fever, and general malaise, which subsequently progressed to include nausea and vomiting. Laboratory investigations revealed significantly elevated liver enzymes and bilirubin levels. Comprehensive serological testing confirmed an EBV infection. Despite the absence of typical risk factors, this case underscores the importance of considering EBV in the differential diagnosis for young adults presenting with both infectious symptoms and abnormal liver function tests. Early recognition of such atypical presentations is crucial for guiding appropriate management and avoiding unnecessary diagnostic procedures.
Categories: Internal Medicine, Infectious Disease.
Keywords: Case Report; Hyperbilirubinemia; Cholestatic Hepatitis; Infectious Mononucleosis; Epstein Barr Virus.
Introduction
Epstein-Barr Virus (EBV) is a prevalent human herpesvirus responsible for infectious mononucleosis, commonly known as "mono." This condition is often characterized by symptoms such as fever, sore throat, and lymphadenopathy, and is most frequently observed in adolescents and young adults. EBV is transmitted primarily through saliva, which is why it is sometimes referred to as the "kissing disease" [1,2].
While most EBV infections are self-limiting and resolve without complications, they can occasionally present with atypical features, such as cholestatic hepatitis and hyperbilirubinemia. Hepatic involvement is common in EBV infections, with mild to moderate liver enzyme elevations occurring in 80-90% of cases. However, the development of cholestatic hepatitis, marked by significant jaundice and elevated bilirubin levels, is rare, occurring in less than 5% of cases [3,4,5].
This case report focuses on a 24-year-old male who presented with atypical EBV infectious mononucleosis, including cholestatic hepatitis and hyperbilirubinemia. Such presentations can complicate the diagnostic process, as they may mimic other hepatic or biliary conditions. The report emphasizes the importance of considering EBV in the differential diagnosis of young adults with infectious symptoms and abnormal liver function tests, even in the absence of typical risk factors [3,5].
Case Presentation
An otherwise healthy 24-year-old male of South Asian descent who presented to the emergency department after six days of infectious symptoms, including a sore throat, intermittent fevers, headache, and general malaise. The patient denied cough, rhinorrhea, or congestion and reported taking one 650 mg dose of acetaminophen during the past week. Three days prior to presentation, he began experiencing nausea and vomiting. He endorsed post-tussive epigastric pain but denied abdominal pain, diarrhea, or constipation. Multiple home COVID-19 tests were negative. There was no history of intravenous drug use, recent travel, or sick contacts. He had a new tattoo three months prior but no rash or skin changes. The patient reported a new sexual partner two months ago but denied genital pruritus, lesions, or penile discharge. He had not been in an environment with potential tick exposure.
On presentation, he was afebrile (37.3 °C), tachycardic (106 bpm), with a blood pressure of 137/91 mmHg, respiratory rate of 18 breaths/minute, and oxygen saturation of 100% on room air. After administration of fluids, his heart rate normalized to 88 bpm. The patient was in no acute distress, and no scleral icterus was present. His mucous membranes were moist, and tonsillar hypertrophy with exudates was visible. Mild cervical lymphadenopathy was palpated. Cardiovascular, respiratory, and abdominal examinations were unremarkable.
Investigations: Bloodwork on admission was notable for [Table 1].
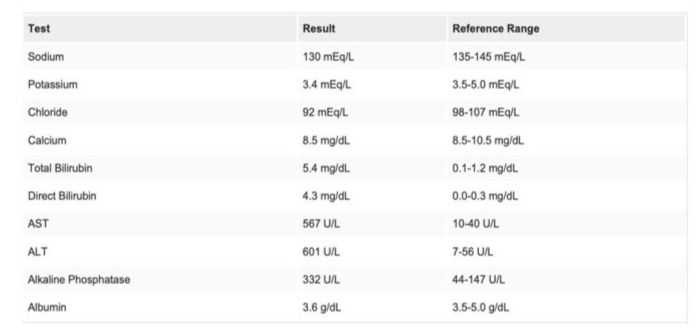
Table 1: Labs on admission.
Blood cell count was within normal limits, but the white blood cell differential showed lymphocytosis (6.1 x 10^9/L). Urinalysis was notable for moderate bilirubin. Hepatitis serologies were negative for Hepatitis A IgM antibody, Hepatitis B surface antigen, Hepatitis B core IgM antibody, and Hepatitis C antibody. Tests for syphilis, chlamydia, gonorrhea, and HIV were negative. An extensive viral respiratory panel was also negative for adenovirus, pertussis, SARS-CoV-2, and other respiratory pathogens. The rapid strep test was negative. Gamma-glutamyl transferase (GGT) and prothrombin time/INR were normal.
An abdominal ultrasound showed no evidence of cholecystitis. ERCP demonstrated a contracted gallbladder without gallstones, a normal common bile duct [Figure 1], and splenomegaly (15 cm).
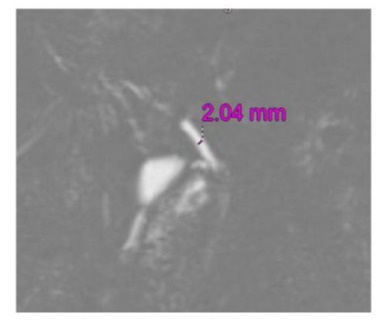
Figure 1: T2 3D MRCP showing Biliary ducts: Normal in caliber (CBD=2 mm).
On day four of hospitalization, EBV serology returned positive, with an EBV capsid antigen IgM antibody >160 and EBV early antigen 48.8. The monoscreen was also positive. Bloodwork on day five showed a peak bilirubin level of 6.9 mg/dL, with decreasing liver function tests (AST 298 U/L, ALT 629 U/L).
Past Medical History: The patient had no diagnosed medical conditions and was not taking any medications. He reported rare alcohol consumption, occasional marijuana use, and denied tobacco or illicit drug use. He had no history of sexually transmitted infections but reported sexual activity with a new partner within the past three months.
Differential Diagnosis: The differential diagnosis included a viral upper respiratory illness, with a high suspicion for EBV or influenza. Gastroenteritis was also considered given the vomiting and the patient's recent consumption of food from a new restaurant. Viral hepatitis was considered due to the recent tattoo and sexual activity. The rising AST/ALT and bilirubin levels raised concerns for choledocholithiasis or resolving cholangitis.
Management: The patient was managed conservatively due to the lack of evidence supporting the use of antivirals or steroids for EBV-related mononucleosis. IV fluids and IV ketorolac were administered for pain. Given his reduced PO intake from a sore throat, he received phenol spray and benzocaine lozenges. Ondansetron was given for nausea. On day five of hospitalization, the patient developed a fever of 102.9 °F, which resolved with acetaminophen. Due to the fever and a rising white blood cell count (from 8.5 to 10.4), blood cultures were obtained, and an ENT consultation was requested to evaluate the risk of superimposed bacterial pharyngitis.
Discussion
Epstein-Barr Virus (EBV) is a common infectious agent responsible for infectious mononucleosis, primarily affecting adolescents and young adults. The classic symptoms include fever, sore throat, fatigue, and lymphadenopathy. While most EBV infections are self-limiting, atypical presentations, such as cholestatic hepatitis and hyperbilirubinemia, are rare but significant. Cholestatic hepatitis is a rare complication of EBV infection, and jaundice is infrequently reported, particularly in younger individuals; it is more commonly observed in patients aged 35 and older [6-8]. When jaundice occurs in the context of EBV, it may be attributed to various causes, including autoimmune hemolytic anemia, cholestasis due to acalculous cholecystitis, biliary duct obstruction from abdominal lymphadenopathy, or direct cholestatic hepatitis [9,10]. The exact pathogenesis of cholestatic hepatitis associated with EBV remains unclear. It is unlikely that EBV directly infects hepatocytes, biliary epithelium, or vascular endothelium. Some theories suggest that cholestasis in EBV cases may be related to lipid peroxidation and the subsequent production of free radicals, contributing to liver injury [6,9].
Although mild elevations in liver enzymes are common, significant hyperbilirubinemia is unusual and can complicate the clinical picture, often prompting consideration of other etiologies, including viral hepatitis or biliary obstruction, before confirming EBV as the cause [5,11].
Current guidelines emphasize the importance of supportive care in managing EBV infections, as there is no specific antiviral treatment proven to reduce the severity or duration of the disease. Symptomatic management, including hydration, rest, and analgesics, remains the cornerstone of treatment. The use of corticosteroids is generally reserved for severe complications, such as airway obstruction or severe hemolytic anemia [5,12].
This case underscores the necessity of including EBV in the differential diagnosis for young adults presenting with both infectious symptoms and abnormal liver function tests, even in the absence of typical risk factors. Awareness of such atypical presentations can prevent unnecessary investigations and guide appropriate management strategies [5,12].
Conclusions
This case highlights the importance of recognizing EBV as a potential cause of cholestatic hepatitis and hyperbilirubinemia, even in young adults without typical risk factors for liver disease. The unusual presentation of EBV in this patient emphasizes the need for clinicians to consider a broad differential diagnosis when encountering elevated liver enzymes and bilirubin levels in the context of infectious symptoms. Prompt identification of EBV can prevent unnecessary diagnostic investigations and support timely, appropriate management. This case contributes to the growing awareness of the diverse clinical manifestations of EBV and reinforces the value of a thorough and systematic approach in the evaluation of atypical cases.
Additional Information
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study. Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
- Centers for Disease Control and Prevention. (n.d.). About infectious mononucleosis (mono). Centers for Disease Control and Prevention. Accessed: 8/8/2024.
- Gequelin LC, Riediger IN, Nakatani SM, Biondo AW, Bonfim CM (2011) Epstein-Barr virus: general factors, virus- related diseases and measurement of viral load after transplant. Rev Bras Hematol Hemoter. 2011:383-8.
- Lin J, Sivasubramanian G (2022) Double Trouble: A Primary Epstein-Barr Virus Infection Causing Cholestatic Hepatitis and Hemophagocytic Lymphohistiocytosis. Cureus. 14:31014-10.
- Jadah, R. H. S, Shaikho, N. M. G, & Hasan, S. A (2021) Unusual Presentation of Epstein-Barr Virus-Associated Cholestatic Hepatitis in an Infant. JPGN reports, 2: e089.
- Jerome, A., Khanna V, Akagi E, Bhargava A (2023) A rare presentation of infectious mononucleosis: cholestatic hepatitis with hyperbilirubinemia. Germs. 13:80-85.
- Hinedi TB, Koff RS (2005) Cholestatic hepatitis induced by Epstein-Barr virus infection in an adult. Dig Dis Sci. 3:539-41.
- Shaukat A, Tsai H, Rutherford R, Anania FA (2005) Epstein-Barr virus induced hepatitis: an important cause of cholestasis. Hepatol Res. 1:24-6.
- Shkalim-Zemer V, Shahar-Nissan K, Ashkenazi-Hoffnung L, Amir J, Bilavsky E (2015) Cholestatic hepatitis induced by Epstein- Barr virus in a pediatric population. Clin Pediatr (Phila. 12:1153-7.
- Agergaard J, Larsen C (2015) Acute acalculous cholecystitis in a patient with primary Epstein-Barr virus infection: a case report and literature review. Int J Infect Dis. 67:72.
- Salva, I., Silva, I. V, & Cunha, F (2013) Epstein-Barr virus-associated cholestatic hepatitis. BMJ case reports. 2013: bcr2013202213.
- Jaya Sureshbabu M (Pediatric mononucleosis and Epstein-Barr virus infection. Practice Essentials, Background, Pathophysiology). Accessed: 8/8/2024.
- Edoute Y, Baruch Y, Lachter J, Furman E, Bassan L, et al (1998) Severe cholestatic jaundice induced by Epstein-Barr virus infection in the elderly. J Gastroenterol Hepatol. 8:821-4.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.