Spontaneous Regression of Massive Lumbar Disc Herniations: Report of Six Cases and Review of the Literature
Authors: Dimitrios V. Papadopoulos1, Athanasios Karageorgos2*, Dimitrios Kosmas1, Ioannis Gkiatas1, Aristomenis Tsovilis1, Emilios Pakos1, Anastasios V. Korompilias1, Ioannis D. Gelalis1
*Corresponding Author: Athanasios Karageorgos, Ortopaedic Department Olympion Therapeutirion Patron, Volou & Milichou Patra, Dragatsaniou 21 & Papaflessa Pirgos Ilias Greece, Postal code: 27131, Greece.
1Department of Οrthopedics, University Hospital Of Ioannina, Stavros Niarchos Avenue, 45500 Ioannina, Greece
2Ortopaedic Department Olympion Therapeutirion Patron, Volou & Milichou Patra, Greece
Received Date: 16 December, 2021
Accepted Date: 30 December, 2021
Published Date: 31 December, 2021
Citation: Papadopoulos DV, Karageorgos A, Kosmas D, Gkiatas I, Tsovilis A, et al. (2021) Spontaneous Regression of Massive Lumbar Disc Herniations: Report of Six Cases and Review of the Literature. J Orthop Res Ther 6: 1208. DOI: https://doi.org/10.29011/2575-8241.001208
Abstract
Background: Spontaneous regression of massive disc herniations is considered to be a highly likely scenario in the natural course of disc herniations, but there is sparse evidence regarding the treatment strategy and their natural history.
Material and Method: This is a report of six cases with massive disc herniations that treated conservatively and in which complete resolution of symptoms along with nearly total regression of the herniated discs on Magnetic Resonance Imaging (MRI) was achieved, even in those cases with positive but not progressive neurological symptoms. Although it is mainly unclear what determines if a herniated disc will resolve or not, there is some evidence that large disc herniations regress in a higher rate than the smaller ones. Many surgeons, under the fear of cauda equina syndrome advise patients with massive disc herniations on surgical treatment.
Conclusion: The decision for surgical treatment based on just the size of the herniation and not based on clinical ground is not recommended, since these massive herniations may resolute as well as shown in this study.
Keywords: Massive disc herniation; Spontaneous regression
Introduction
The natural course of lumbar disc herniation is not fully elucidated. There is evidence that the natural history of this pathology may be more benign than previously thought and that most herniated discs eventually regress. The incidence of spontaneous regression is estimated to be up to 66% according to recent studies [1]. Although it is mainly unknown what are the main determinants for the spontaneous regression of disc herniations, rim enhancement thickness on Magnetic Resonance Imaging (MRI), higher degree of herniated nucleus pulposus displacement in the Komori classification, and age category 41-50 years are associated with a higher resorption rate [2]. Conversely, spontaneous resorption is less likely to occur in cases with associated lumbar degenerative changes [3].
Although smaller disc herniations that do not produce progressive neurologic deficits are managed conservatively, symptomatic massive tears are usually treated surgically under the fear of cauda equina syndrome. The large size of several massive disc herniations may mislead surgeons to operate patients with no clear indications for surgical management. A chance for conservative treatment must be given initially to patients with massive or large disc herniations and radicular pain as long as there are no progressive neurologic deficits. If there are signs of improvement, conservative treatment should be continued and subsequent MRI evaluation must be performed. We present six cases of large herniated discs that treated non-operatively and in whom subsequent MRI evaluation a year later showed almost complete resorption of disc material.
Cases Presentation
Case 1
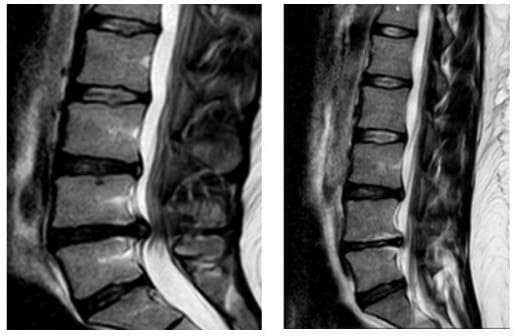
A 45-year-old male patient presented to outpatient clinic complaining of intermittent back and radicular pain along L5 dermatomal distribution for the past month. On physical examination there was no muscle strength impairment or altered sensation but straight leg raising test was positive at 20º. MRI of the lumbar spine was done and demonstrated a significant L4-5 disc herniation (Figure 1a). The patient treated conservatively with short term bed rest, NSAID, analgesics and physical therapy. The patient returned for re-evaluation three weeks after the initial assessment and mentioned slight improvement of his symptoms. Due to remaining symptoms, an epidural corticosteroid injection was given and the patient was advised to continue physical therapy. Within two weeks since the epidural injection, the patient reported marked improvement and remained free of pain for the following period. MRI of lumbar spine was repeated one year after the initial MRI, which revealed regression of the herniated lumbar disc (Figure 1b).
Case 2
A 33-year-old man with a history of mild, recurrent low back pain presented with several months of new right leg pain and numbness in the S1 dermatomal distribution. The patient denied weakness or bowel and bladder symptoms. On physical examination strength and reflexes were normal in the bilateral lower extremities and a positive straight leg raising test was reproduced at 30º. Palpation of the right lumbar paraspinal musculature produced mild discomfort and myofascial spasm. MRI of the lumbar spine revealed a large L4-L5 disc herniation (Figure 2a). Conservative treatment including short term bed rest, NSAID, analgesics, and physical therapy was advised. Near complete resolution of symptoms was achieved with a subsequent steroid injection.cRepeat MRI of the lumbar spine ten months later demonstrated resolution of the disc extrusion (Figure 2b). The patient continued to have mild intermittent symptoms, but largely remained pain free.
Case 3
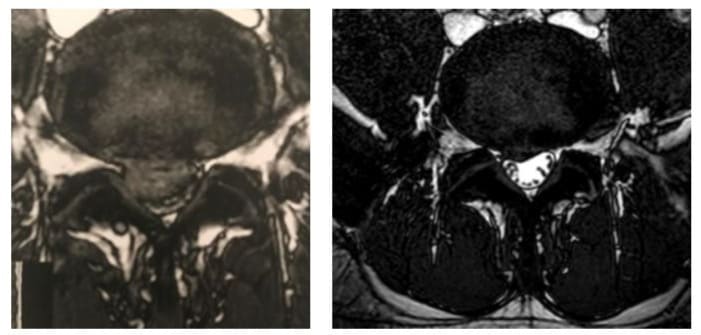
A 38-year-old female patient presented to the outpatient clinic of our department with complaints of constant back and right buttock pain with “Shooting” sensations extending distally in her right lower limb for the past six weeks. The patient also mentioned numbness and tingling sensation along the lateral side of her lower leg, but she denied any bowel or bladder dysfunction. Physical examination revealed a positive straight leg raising test at 15°, while sensory and reflex examination was unremarkable. Objective weakness of the great toe extension and ankle plantar flexion was present, graded as 3/5 (according to MRC classification) for both actions An MRI of her lumbar spine was done and showed a massive L5-S1 disc herniation occupying more than half of the spinal canal (Figure 3a). Although the patient was advised to undergo a miscodiscectomy, she refused any surgical intervention and preferred to be treated conservatively. A course of NSAIDS, analgesics and physical therapy was initiated for the following three weeks. After this period the patient returned to the office and reported slight improvement of her symptoms. Physical examination demonstrated that the noted weakness of great toe extension and ankle plantar flexion during the previous examination was restored. Due to the residual symptoms, an epidural corticosteroid injection was given and physical therapy was continued for another three weeks. The patient was contacted by telephone at six weeks after the initial presentation and she reported complete resolution of the symptoms. The patient was re-evaluated a year after her first visit to our outpatient clinic and a second MRI of her lumbar spine was performed. The new MRI demonstrated almost total resorption of the herniated disc, consistent with the complete resolution of her symptoms (Figure 3b).
Case 4
A 21-year-old female patient presented to the outpatient clinic of our department complaining of recurrent low back pain the last three weeks and constant buttock pain the last ten days. The patient denied any bowel and bladder dysfunction. Physical examination revealed a positive straight leg raising test at 20o, but no muscle strength impairment or altered sensation, while reflex examination was unremarkable. MRI of the lumbar spine displayed a large L4-L5 central disc herniation (Figure 4a). She treated conservatively with NSAIDS, analgesic and physical therapy for the next three weeks. One month later she presented to the office with marked improvement of her symptoms. She was advised to continue physical therapy for three more weeks. At the last evaluation, eight weeks after her first presentation, the patient was presented with almost complete resolution of symptoms. MRI of the lumbar spine was repeated ten months later and was revealed almost complete resorption of the herniated L4-L5 disc (Figure 4b).
Case 5
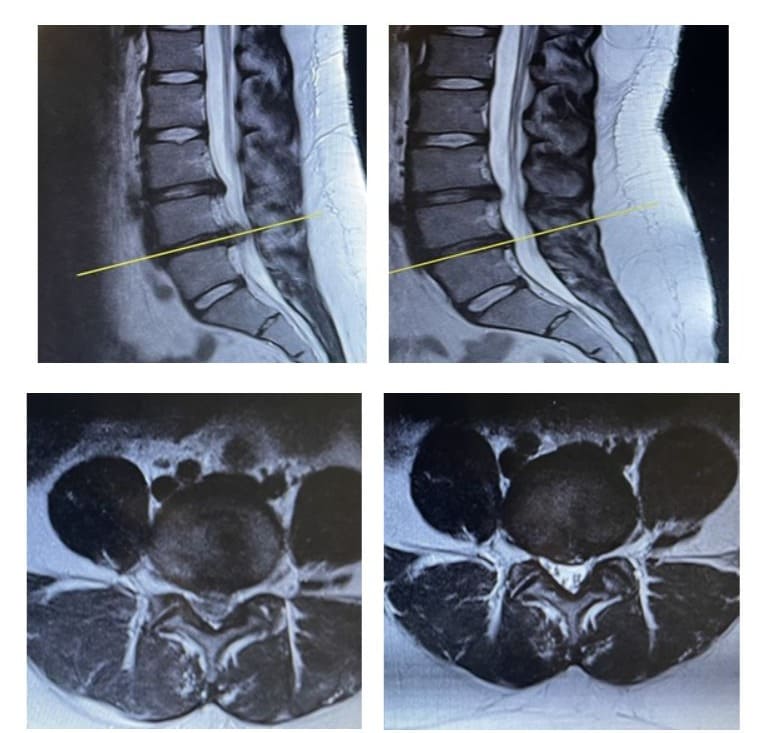
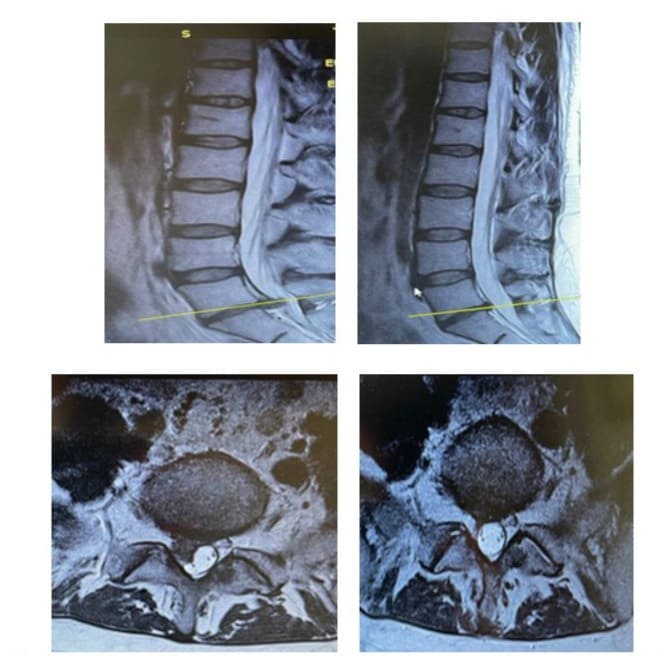
A 40-year-old female presented to the outpatient clinic of our department complaining of constant back pain reflecting to the right calf the past three weeks. The patient also mentioned numbness in the L5 dermatomal distribution of her right leg. She denied any bowel and bladder dysfunction. Weakness of the right great toe extension and ankle plantar flexion was present, graded as 4/5 (according to MRC classification) for both actions. Reflex examination was unremarkable. Furthermore a positive straight leg raising test was reproduced at 20º to the contralateral leg. A lumbar spine MRI depicted a massive central L4-L5 disc herniation (Figure 5a, c). Due to muscle strength impairment she was advised to undergo microdiscectomy, but she refused any surgical intervention. The patient treated with short term bed rest, NSAID, analgesics, physical therapy and activity modification for a month. Four months after the initial presentation the patient revealed significant improvement of the pain and after six months complete resolution of the symptoms and muscle strength restoration was noted. A second MRI of the lumbar spine was performed one year after the initial diagnosis and demonstrated great reduction of the L4-L5 disc herniation (Figure 5b, d).
Case 6
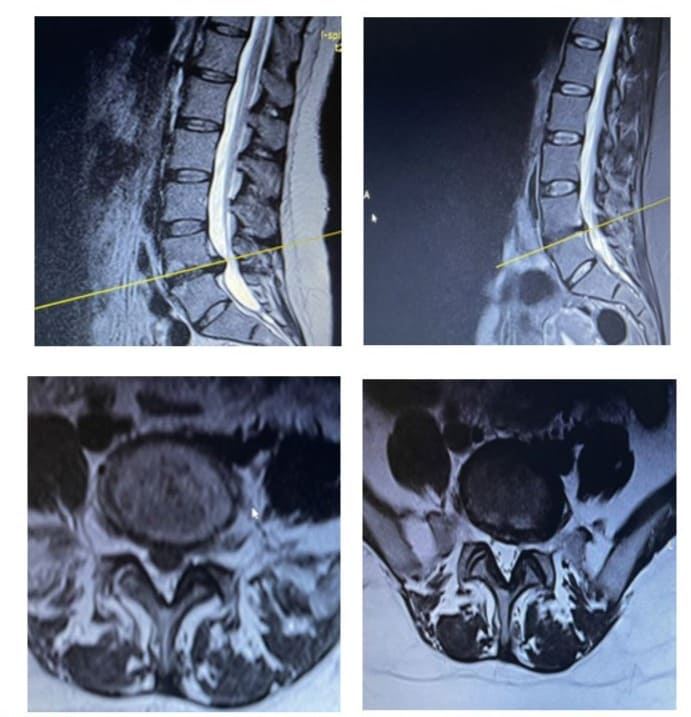
A 35-year-old female presented to the outpatient clinic of our department and reported low back pain the last three weeks, which was treated with NSAIDS. The last three days despite low back pain improvement, she developed ‘Shooting’ sensation, numbness and pain, extending distally to the right calf and foot. Her bladder and bowel function was unremarkable. Clinical evaluation revealed a positive straight leg raising test at 20o, absence of right Achilles tendon reflex, and weakness of right ankle plantar flexion, grated as (3/5) (according to MRC classification). . A lumbar spine MRI depicted a massive right-centrally located L5-S1 disc herniation (Figure 6a, c). A L5-S1 microdiscectomy was suggested to the patient, but she refused any surgical intervention. She treated with short term bed rest, continuation of NSAIDS for one more week, physical therapy and activity modification for a month. After this period she presented for re-evaluation. She had remarkable improvement in muscle strength (4/5), but still she complained for aching pain to the right calf and foot. Due to these symptoms, an epidural injection was given and physical therapy was continued for 1 more month. Six weeks later she presented with restored muscle strength, and great improvement in leg pain. MRI of the lumbar spine was repeated ten months later and revealed almost complete resorption of the herniated L5-S1 disc (Figure 6b, d).
Discussion
There is no absolute correlation between MRI findings and clinical symptoms. In up to 76% of asymptomatic individuals MRI imaging will demonstrate disc herniation. The most significant factor correlating MRI findings with clinical symptoms is whether neural elements like exiting nerve roots are compressed by the disc material or not [4]. Cauda equina syndrome belongs to a category of the most serious diseases of spinal cord, and is an absolute indication for urgent surgery [5]. Cauda equine syndrome due to lumbar disc herniation is 1-3% of all disc herniation [6]. According to searches there is a minimal space occupied by the dural sac, necessary for the nerve roots of the cauda equine, constituting almost 44% of the normal cross sectional area. Therefore a small reduction can cause an abrupt increase in the pressure inside the dural sac [7]. Although there is evidence that most herniated discs, even the large ones, eventually resolve, surgeons must be very cautious with regards to the recommended treatment plan for disc herniations.
There are two different proposed theories regarding the resorption mechanism of herniated discs. According to the first theory regression occurs through dehydration of the nucleus pulposus and shrinkage, while the herniated material retracts back into the annulus fibrous [8]. The pathophysiology of the second proposed theory includes an inflammatory process occurring at the outermost layer of herniation in which macrophages play a major role as the main phagocyting cell population. The signal that is observed around the rim of herniated discs on contrast-enhanced MRI probably represents neovascularization due to macrophage infiltration [9].
There are several studies evaluating the natural course of disc herniations, but there is sparse evidence regarding the possibility of regression of large or massive disc herniations. Jensen et al evaluated the progression of herniated discs in 154 patients with sciatica. They found that broad-based protrusions, extrusions and sequestrations improved more than bulges and focal protrusions [10]. Cribb et al showed that in 14 out of 15 patients with massive herniations who treated non-operatively, repeat MRI scanning after a mean 24 months depicted dramatic resolution of the herniation [11]. In another study regarding massive disc herniations, Bozzao et al presented 8 patients with disc herniations occupying more than 50% of the canal [12]. Follow up MRI demonstrated more than 70% reduction in size in 6 of those patients. There is also a recent meta-analysis assessing the incidence of spontaneous resorption of lumbar herniated discs that includes 11 studies. Authors found that the overall incidence of spontaneous resorption is 66.66% [1].
There is evidence that larger or extruded discs are resorpted in a higher rate than small protrusions [12,13]. Chiu et al evaluated the probability of spontaneous regression of lumbar herniated discs and showed that the incidence of regression is 96% for disc sequestration, 70% for disc extrusion, 41% for disc protrusion, and 13% for disc bulging [14]. The increased rate of resorption in these large herniations may be explained by the fact that the extruded disc lacks the immune protection provided by the outermost layer of annulus fibrosus, thus macrophages are freer to act [11].
The decision regarding surgical or conservative management of disc herniations depends on several factors including clinical symptoms, imaging findings and personal preferences of each patient. In general initial management of herniated discs consists of conservative measures including bed rest, NSAID, physical therapy and corticosteroid injections. Should symptoms remain for over two months, progressive neurologic deficit or cauda equina syndrome develop, surgical treatment is advised [8]. In cases of symptomatic massive disc herniations, surgeons more liberally recommend surgical treatment because cauda equina syndrome is a more likely event. This report of six cases indicate that large or massive herniations may not justify its fearsome reputation and surgeons must advise for surgical treatment based on the same indications that apply for the rest types of disc herniations.
Figures

References
- Zhong M, Liu JT, Jiang H, Mo W, Yu PF, et al. (2017) Incidence of Spontaneous Resorption of Lumbar Disc Herniation: A Meta-Analysis. Pain Physician 20: E45-E52.
- Autio RA, Karppinen J, Niinimäki J, Ojala R, Kurunlahti M, et al. (2006) Determinants of spontaneous resorption of intervertebral disc herniations. Spine (Phila Pa 1976) 31: 1247-1252.
- Shan Z, Fan S, Xie Q, Suyou L, Liu J, et al. (2014) Spontaneous resorption of lumbar disc herniation is less likely when modic changes are present. Spine (Phila Pa 1976) 39: 736-744.
- Janardhana AP, Rajagopal, Rao S, Kamath A (2010) Correlation between clinical features and magnetic resonance imaging findings in lumbar disc prolapsed. Indian J Orthop 44: 263-269.
- Siebert E, Prüss H, Klingebiel R, Failli V, Einhäupl KM, et al. (2009) Lumbar spinal stenosis: syndrome, diagnostics and treatment. Nat Rev Neurol 5: 392-403.
- Fraser S, Roberts L, Murphy E (2009) Cauda equina syndrome: a literature review of its definition and clinical presentation. Arch Phys Med Rehabil 90: 1964-1968.
- Chau AM, Xu LL, Pelzer NR, Gragnaniello C (2014) Timing of surgical intervention in cauda equina syndrome: a systematic critical review. World Neurosurg 81: 640-650.
- Hakan T, Gürcan S (2016) Spontaneous Regression of Herniated Lumbar Disc with New Disc Protrusion in the Adjacent Level. Case Rep Orthop 2016: 1538072.
- Cunha C, Silva AJ, Pereira P, Vaz R, Gonçalves RM, et al. (2018) The inflammatory response in the regression of lumbar disc herniation. Arthritis Res Ther 20: 251.
- Jensen TS, Albert HB, Soerensen JS, Manniche C, Leboeuf-Yde C (2006) Natural course of disc morphology in patients with sciatica: an MRI study using a standardized qualitative classification system. Spine 31:1605-1612.
- Cribb GL, Jaffray DC, Cassar-Pullicino VN (2007) Observations on the natural history of massive lumbar disc herniation. J Bone Joint Surg Br 89: 782-784.
- Bozzao A, Gallucci M, Masciocchi C (1992) Lumbar disc herniation: MR imaging assessment of natural history in patients treated without surgery. Radiology 185: 135-141.
- Macki M, Hernandez-Hermann M, Bydon M, Gokaslan A, McGovern K, et al. (2014) Spontaneous regression of sequestrated lumbar disc herniations: Literature review. Clin Neurol Neurosurg 120: 136-141.
- Chiu CC, Chuang TY, Chang KH, Wu CH, Lin PW, et al. (2015) The probability of spontaneous regression of lumbar herniated disc: a systematic review Clin Rehabil 29: 184-195.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.